Abstract
This study was carried out to determine whether a short-term zinc supplementation contributes to beneficial changes in glycemic control among type 2 diabetic patients. Seventy-six diabetic subjects and 72 normal adults participated in this study. Subjects were divided into supplemented and control groups. Forty-four diabetic patients and 34 normal subjects were supplemented with 50 mg zinc daily as zinc gluconate for 4 weeks. Zinc status was assessed from fasting plasma levels and urinary excretion. The effects of zinc supplementation on fasting blood glucose, HbA1c, insulin, and C-peptide were measured at the beginning of the study and after 4 weeks of supplementation. The changes in glycemic control indicators were compared between diabetic groups, classified by baseline HbA1c levels, and by diabetic duration. At baseline, the incidence of marginal zinc deficiency in the diabetic group, as determined by plasma zinc level, was approximately twice as high as in the normal adult group. The changes of HbA1c concentration, and fasting blood glucose following supplementation were not statistically significant in diabetic subjects. In normal subjects, a significant decrease of HbA1c occurred only in the zinc supplemented group. No significant changes were observed for serum insulin and C-peptide in diabetic as well as normal subjects. However, when the changes were compared by baseline HbA1c level, we found that diabetic subjects with HbA1c ≥ 7.5% showed significantly improved levels of HbA1c and fasting glucose after Zn supplementation. While such improvement in fasting blood glucose was significant among diabetics with shorter diabetic duration, significant levels of increase in serum insulin and C-peptide were observed in zinc supplemented subjects with longer diabetic duration. Fasting blood glucose was significantly decreased, whereas serum insulin and C-peptide were increased in diabetics with marginal zinc status. Therefore, we suggest that Zn supplementation for a short-term period may improve glycemic control in diabetic patients with higher HbA1c levels and marginal zinc status.
Zinc is involved in numerous metabolic pathways as an cofactor for more than 300 enzymes (Rink & Kirchner, 2000). It also plays an important role for insulin action, carbohydrate and protein metabolism (Chausmer, 1998). Insulin, which contains a variable number of zinc atoms, are stored in β-cells of the pancreas and released into the portal venous system at the time of β-cells degranulation. Type 2 diabetes mellitus is a metabolic disorder with hyperglycemia as the dominant feature (Chausmer, 1998).
Several investigators have shown the perturbation of zinc metabolism in diabetics (Golik et al., 1993; Kinlaw et al., 1983; Levine et al., 1983; Walter et al., 1991). It has been suggested that hyperzincuria and impaired absorption are major causes of zinc deficiency among diabetics (Cunningham et al., 1994; Heise et al., 1988; Kazi et al., 2008; Salgueiro et al., 2001; Walter et al., 1991). Clinical manifestations including delayed wound healing, decreased cell immunity and deterioration of taste acuity in this population have been also reported (Keen & Gershwin, 1990; Kinlaw et al., 1983; Salgueiro et al., 2001).
It was suggested that the marginal zinc deficiency may be related with impaired immunity and taste (Salgueiro et al., 2001). Hence, zinc supplementation is receiving growing attention as a way to improve the immune function as well as the marginal zinc deficiency (Anderson et al., 2001; Faure et al., 1995).
Few studies have been conducted on the effects of zinc supplementation on hyperglycemia of diabetics and their results are inconsistent. Zinc supplementation has improved fasting insulin level and fasting glucose in genetically obese mice models (Chen et al., 1998; Simon & Taylor, 2001). Improved fasting glucose levels up to 30% in patients with cirrhosis through supplementation of zinc for 2 months has been reported (Marchesini et al., 1998). Supplementation of 30 mg zinc for 3 months in type 2 diabetics showed a decrease in HbA1c concentration. Meanwhile, others reported that neither fasting glucose nor HbA1c levels was changed by a short-term supplementation with zinc for type 1 diabetics (Cunningham et al., 1994; de Sena et al., 2005).
Type 2 diabetic patients are characterized by reduced secretion of insulin and increased insulin resistance, resulting in elevated blood glucose levels (Roth & Kirchgessner, 1981; Salgueiro et al., 2001). It has not been clearly elucidated whether zinc deficiency is a consequence of hyperglycemia or, alternatively, whether zinc deficiency contributes to the pathogenesis of diabetes.
The National Health and Nutrition Examination Survey for Koreans conducted in 2005 showed that the prevalence of diabetes was 9.0% for male adults and 7.2% for female adults (Ministry of Health & Welfare, 2006). Previous studies indicated that marginal zinc deficiency is more prevalent among diabetic adults compared to the normal adult population (Lee et al., 2005; Yoon & Lee, 2007). Therefore, we intended to determine whether zinc supplementation for a short-term period could improve the levels of fasting glucose and HbA1c as well as the insulin levels in Korean type 2 diabetics. Moreover, this study aimed to find out whether the changes in glycemic control by zinc supplementation are associated with diabetic duration or zinc status.
This study was conducted on 76 type 2 diabetic adults attending local clinics and public heath centers. Characteristics of the diabetic subjects have been reported elsewhere (Yoon, 2008). For comparison, 72 apparently healthy normal adults living in the same city were also recruited during the same period. Informed consent was obtained from each subject before the beginning of the study. Exclusion criteria of the subjects were pregnancy, lactation, consuming mineral supplements or prescribed drugs for diseases. The subjects were divided into zinc supplementation groups and control groups. Among diabetic participants, 44 subjects took zinc supplements. Among 72 normal adults, 32 subjects took zinc supplements.
Information on age, education levels, diabetic duration, drug usage, diabetic complications was interviewed by a trained dietitian.
Height, weight, circumferences of waist and hip, and body fat were measured from each subject. BMI (body mass index) was calculated with measured height and weight. Body fat content and percentage body fat were assessed using the Bio-electrical Impedance Fatness Analyzer (HBF-300, OMRON Corporation, Japan).
Overnight fasting blood samples were collected either into evacuated heparin coated tubes or into serum tubes and were stored at -70℃. HbA1c, fasting blood glucose, serum insulin, and C-peptide were measured as the indicators of glycemic regulation using routine laboratory methods (Roussel et al., 2003). Plasma level of zinc was assessed by atomic absorption spectrometry (Lee et al., 2005). Urine samples for 24 hours were collected for one day from each subject. Urinary zinc was analyzed by Inductively Coupled Plasma Emission Spectroscopy (ICP) (Jobin Yvon, 38 plus, France). We followed the criteria for marginal zinc deficiency from the previous studies (King & Keen, 1994).
Selection of chemical form, dose level, and duration of zinc supplementation in this study were based on the reports of other investigators (Anderson et al., 2001; Bonham et al., 2003; Chandra, 1984; Roussel et al., 2003). Capsules containing 50 mg of zinc gluconate (Labcatal, Pharmaceutical), reported as the safe level for supplementation for 3 months, were given to the diabetic and normal subjects for 4 weeks. Each subject was encouraged to take the supplement everyday. Compliance with the supplementation trial was confirmed at the end of the study. Subjects who reported consuming less than 80% of the total amounts were excluded from the data analysis.
The Statistical Analysis System (SAS) Package was used to analyze the relationship of glycemic control status and zinc supplementation. Data were presented as mean ± SD. The statistical significance of the differences between the diabetic and the normal subjects was tested by the Student's t test. The changes in glycemic indicators were compared between the two diabetic patients groups, first classified by baseline HbA1c levels (<7.5% vs ≥7.5%), then by zinc status (marginal vs normal), and, lastly, by diabetic duration (<4 years vs ≥4 years). Differences in the distribution of variables between the two diabetic groups were tested by the Student's t test. The effects of zinc supplementation on hyperglycemia of diabetics were tested by paired t-test. When any variables show significant differences between supplemented and non-supplemented groups at baseline, analysis of covariance (ANCOVA) was used to determine the effects of supplementation.
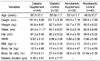
Baseline characteristics of the participants such as age, diabetic duration, are shown in Table 1. Details on the characteristics of the diabetic subjects were described in previous reports (Yoon, 2008). Among diabetic participants, 44 subjects were provided with zinc supplement, while 32 subjects participated as the control group. Among the 72 normal adults, 32 subjects took zinc supplement. The average age of the zinc supplemented diabetics was 58.7 ± 10.1 years and that of the diabetic control group was 58.5 ± 11.7 years. The average age of the zinc supplemented normal adults group was 53.1 ± 11.7 years and that of the diabetic control group was 49.6 ± 10.7 years. There were no significant differences in baseline physical characteristics such as age, height, weight, body mass index (BMI), circumferences of waist and hip, or body fat (%) between the diabetic and the non-diabetic adults groups. All of these variables were not significantly different between the supplemented and the control group in diabetic or non-diabetic subjects. Diabetic duration was 5.38 ± 3.61 years for the diabetic supplemented group, 6.51 ± 7.77 years for the diabetic control group. All the physical characteristics were similar between subgroups of the subjects classified by diabetic duration.
Table 2 shows the incidence of marginal zinc deficiency at baseline by plasma zinc level and urinary excretion. In the diabetic group, more than 40% of the subjects had marginal zinc deficiency by plasma zinc level. By contrast, the incidence of marginal zinc deficiency was 22.6% in the normal supplemented, and 24.3% in the normal control adults. After 4 weeks of zinc supplementation, incidence of marginal zinc deficiency decreased to 22.5% in the diabetic supplement group. When the incidence of zinc deficiency was evaluated by urinary zinc level, 33.3% of the diabetic supplement group, and 20% of the diabetic control group were diagnosed to have marginal zinc deficiency at baseline. More than 30% of normal adults were found to have marginal zinc deficiency by urinary zinc excretion.
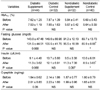
Table 3 compares the baseline results of HbA1c, fasting blood glucose, insulin, and C-peptide, which are possible indicators of glycemic control and insulin resistance, in diabetic and non-diabetic subjects. All of these variables at baseline were not significantly different between the supplemented and the control groups in diabetic or non-diabetic subjects. The fasting blood glucose and HbA1c in the diabetic group were significantly higher than the values of the normal group. However, there were no significant differences in insulin and C-peptide levels between the two groups. Serum levels of insulin and C-peptide in diabetic subjects were within normal ranges (insulin : 2~25 uIU/mL and C-peptide : 0.48~3.30 ng/mL). The average HbA1c of diabetics was higher than the normal range (4~6%), however, it did not belong to the level of action suggested for the treatment (>8.0%) (Palumbo, 2001).
The representative long term indicator, HbA1c did not change by 4 weeks zinc supplementation as is shown in Table 3. While HbA1c of the diabetic group slightly decreased from 7.62% to 7.53% following zinc supplementation, without statistical significance, no changes occurred in diabetic control groups. By contrast, a significant decrease of HbA1c was observed for zinc supplemented normal adults after 4 weeks of supplementation. While the fasting plasma glucose level decreased from 143.1 mg/dL to 131.5 mg/dL (p=0.068) in diabetic patients, serum levels of insulin as well as C-peptide were slightly increased after zinc supplementation (p=0.068, p=0.06).
When the effect of zinc supplementation on glycemic control was further analyzed by the baseline HbA1c level of the diabetic subjects (HbA1c<7.5% vs HbA1c≥7.5%) as shown in Table 4, significant decreases (p<0.05) of fasting glucose and HbA1c were found in the higher HbA1c group after 4 weeks of supplementation. HbA1c level changed from 8.57% to 8.30% and fasting glucose changed from 169.7 mg/dL to 150.7 mg/dL. Marginal changes of insulin and C-peptide were also shown in higher HbA1c.
In order to figure out whether glycemic control indicators respond to the zinc supplementation differently by diabetic duration, we compared the changes of HbA1c, fasting glucose, insulin and C-peptide by the diabetic duration period as shown in Table 5. The fasting glucose was significantly reduced, after supplementation, among diabetics with less than 4 years of duration (Table 5). Meanwhile, insulin and C-peptide were significantly increased by supplementation in diabetics with more than 4 years of duration (p<0.001, p<0.05). Marginal improvement with supplementation was observed for HbA1c (p=0.076). The changes of glycemic control indicators after zinc supplementation was compared by plasma zinc levels of the subjects as presented in Table 6. When we compared the HbA1c, fasting plasma glucose, insulin and C-peptide between the two groups classified by baseline plasma level of zinc, significant changes in fasting blood glucose, insulin and C-peptide were observed for zinc supplemented diabetics with lower zinc status (p<0.05).
The Korean National Health and Nutrition Examination Survey indicated that the prevalence of diabetes mellitus has continuously increased in Korea (Ministry of Health & Welfare, 2006). Accordingly, public awareness on dietary practice to control the blood glucose level is growing, because maintaining the blood glucose in the normal range is essential to prevent or reduce the risk for diabetic complication (Kim et al., 1998; Franz et al., 2003). In this study, the average level of HbA1c for diabetic subjects (7.62%, 7.87%) were higher than normal range (5.0~6.0%), whereas that of normal subjects were 5.84% and 5.69. Fasting glucose level of diabetics were above normal range (70~120 mg/L). Both HbA1c and fasting glucose were significantly higher in diabetics than normal subjects (p<0.001). These results indicated that most of diabetic participants in this study were not under a tight glycemic control. Most of the diabetic subjects did not participate in a diabetic management program or visit doctors regularly. It seemed that they were not aware of the importance of dietary practice to control blood glucose level. Thus, inappropriate food choices might have resulted in the deterioration of zinc status.
As hyperzincuria has been frequently reported among diabetics, which might be potential indications of zinc deficiency, zinc supplementation has been suggested to ameliorate the metabolic disturbance of diabetics (Salgueiro et al., 2001). Baseline levels of insulin and C-peptide in diabetic subjects were within normal range. Our study showed that serum insulin and C-peptide were significantly increased after zinc supplementation in patients with more than 4 years history of diabetics. Previous investigators have hypothesized that zinc enhances tyrosine kinase phosphorylation in the insulin signal transduction from in vitro studies (Simon & Taylor, 2000). However, it is hard to conclude from our results that the changes of insulin level following 4 weeks of supplementation reflect an improvement in insulin resistance. This is because we did not collect the data on insulin receptor and/or the changes of insulin-stimulated enzyme activities.
In this study, marginal changes of blood glucose level (p=0.068) following supplementation was observed in diabetic subjects. An animal study showed that dietary zinc supplementation attenuated fasting hyperglycemia whereas a marginally Zn-deficient diet exacerbated fasting hyperglycemia in db/db mice (Simon & Taylor, 2001).
HbA1c concentration of diabetic patients did not change significantly after 4 weeks of zinc supplementation. Considering the fact that HbA1c reflects 2-3 months of glycemic control, our results are not unexpected. Our findings on the changes of HbA1c after 4 weeks of supplementation are consistent with the previous studies. It has been reported that zinc supplementation did not improve the level of HbA1c, while it was beneficial to maintaining immunity in type 2 patients (Niewoehner et al., 1986). Others also found that six months of zinc supplementation (=30 mg/day) did not modify the level of HbA1c nor glucose homeostasis significantly (Anderson et al., 2001; Roussel et al., 2003).
When we attempted to compare the magnitude of the supplementation effects by the status of glycemic control or diabetic duration, we observed that more significant effects occurred in less controlled groups or those with a longer medical history of diabetes. Higher levels of HbA1c and fasting glucose with longer diabetic duration have been noted by other investigators (Rho & Ko, 1997). Therefore, we suggest that a short-term zinc supplementation may be effective on glycemic control for diabetic patients with higher HbA1c% concentration and shorter history of diabetes.
Significant changes in fasting blood glucose, insulin and C-peptide were observed for zinc supplemented diabetics with lower zinc status (p<0.05) in our study. A recent randomized, clinical trial reported that 3 months of zinc supplementation (30 mg/day) for type 2 diabetics may have beneficial effects in elevating serum zinc level, and improving their glycemic control as shown by decreasing their HbA1c% concentration (Al-Maroof & Al-Shabatti, 2006).
In summary, our study indicated that significant improvement of fasting glucose as well as HbA1c were observed in zinc supplemented diabetic patients with shorter diabetic duration, poorer glycemic control, and marginal zinc status. However, further investigation is needed before a firm conclusion could be drawn for the relationship between zinc supplementation and glycemic control. At present, more attention must be paid to improving the zinc status and glycemic control of Korean diabetic patients in order to prevent or minimize complications.
Figures and Tables
References
1. Anderson RA, Roussel AM, Zouari N, Mahjoub S, Matheau JM, Kerkeni A. Potential antioxidant effects of zinc and chromium supplementation in people with type 2 diabetes mellitus. J Am Coll Nutr. 2001. 20:212–218.

2. Al-Maroof RA, Al-Sharbatti SS. Serum zinc levels in diabetic patients and effect of zinc supplementation on glycemic control of type 2 diabetics. Saudi Med J. 2006. 27:344–350.
3. Bonham M, O'Connor JM, Alexander HD, Coulter J, Walsh PM, McAnena LB, Downes CS, Hannigan BM, Strain JJ. Zinc supplementation has no effect on circulating levels of peripheral blood leucocytes and lymphocyte subsets in healthy adult men. Br J Nutr. 2003. 89:695–703.

4. Chandra RK. Excessive intake of zinc impairs immune responses. J Am Med Assoc. 1984. 252:1443–1446.

6. Chen MD, Liou SJ, Lin PY, Yang VC, Alexander PS, Lin WH. Effect of zinc supplementation on the plasma glucose level and insulin activity in genetically obese (ob/ob) mice. Biol Trace Elem Res. 1998. 61:303–311.

7. Cunningham JJ, Fu A, Mearkle PL, Brown RG. Hyperzincuria in individuals with insulin-dependent diabetes mellitus : concurrent zinc status and the effect of high-dose zinc supplementation. Metabolism. 1994. 43:1558–1562.

8. de Sena KC, Arrais RF, das Graças Almeida M, de Araújo DM, dos Santos MM, de Lima VT, de Fãtima Campos Pedrosa L. Effects of zinc supplementation in patients with type 1 diabetes. Biol Trace Elem Res. 2005. 105:1–9.

9. Faure P, Benhamou PY, Perard A, Halimi S, Roussel AM. Lipid peroxidation in insulin-dependent diabetic patients with early retina degenerative lesions: effects of an oral zinc supplementation. Eur J Clin Nutr. 1995. 49:282–288.
10. Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, Holzmeister LA, Hoogwerf B, Mayer-Davis E, Mooradian AD, Purnell JQ, Wheeler M. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2003. 26:S51–S61.

11. Golik A, Cohen N, Ramot Y, Maor J, Moses R, Weissgarten J, Leonov Y, Modai D. Type II diabetes mellitus, congestive heart failure, and zinc metabolism. Biol Trace Elem Res. 1993. 39:171–175.

12. Heise CC, King JC, Costa FM, Kitzmiller JL. Hyperzincuria in IDDM women : Relationship to measure of glycemic control, renal function, and tissue catabolism. Diabetes care. 1988. 11:780–786.

13. Kazi TG, Afridi HI, Kazi N, Jamali MK, Arain MB, Jalbani N, Kandhro GA. Copper, chromium, manganese, iron, nickel, and zinc levels in biological samples of diabetes mellitus patients. Biol Trace Elem Res. 2008. 122:1–18.

15. Kim YI, Choi CS, Kim SW, Lee JS, Kim HH, Lee MS, Lee SI, Park JY, Hong SK, Lee KU. Prevalence of Diabetes Mellitus and impaired glucose tolerance in Korean adults living in Jungup District, South Korea. J Kor Diabetic Associ. 1998. 22:363–371.
16. Kinlaw WB, Levine AS, Morley JE, Silivis SE, McClain CJ. Abnormal zinc metabolism in type II diabetes mellitus. Am J Med. 1983. 75:273–277.

17. King JC, Keen CL. Shils ME, Olson JA, Shike M, editors. Zinc. Modern nutrition in health and disease. 1994. 8th ed. Malvern. UK: Lea & Febiger;214–230.
18. Lee JH, Lee HJ, Lee IK, Yoon JS. Zinc and copper status of middle- and old-aged woman in type 2 diabetes. The Korean Journal of Nutrition. 2005. 38:56–66.
19. Levine AS, McClain CJ, Handwerger BS, Brown DM, Morley JE. Tissue zinc status of genetically diabetic and streptozotocin-induced diabetic mice. Am J Clin Nutr. 1983. 37:382–386.

20. Marchesini G, Bugianesi E, Ronchi M, Flamia R, Thomaseth K, Pacini G. Zinc supplementation improves glucose disposal in patients with cirrhosis. Metabolism. 1998. 47:792–798.

21. Ministry of Health & Welfare. Report on 2005 National health and nutritional survey. 2006. Seoul, Korea:
22. Niewoehner CB, Allen JI, Boosalis M, Levine AS, Morley JE. Role of zinc supplementation in type II diabetes mellitus. Am J Med. 1986. 81:63–68.

23. Palumbo PJ. Glycemic control, mealtime glucose excursions, and diabetic complications in type 2 diabetes mellitus. Mayo Clin Proc. 2001. 76:608–618.

24. Rink L, Kirchner H. Zinc-altered immune function and cytokine production. J Nutr. 2000. 130:1407s–1411s.

25. Rho SN, Ko HS. A clinical properties on nutrients intake and serum concentration of diabetic subjects by duration in Ansung Kyunggi-do. The Korean Journal of Nutrition. 1997. 30:1203–1210.
26. Roussel AM, Kerkeni A, Zouari N, Mahjoub S, Matheau JM, Anderson RA. Antioxidant effects of zinc supplementation in Tunisians with type 2 diabetes mellitus. J Am Coll Nutr. 2003. 22:316–321.

28. Salgueiro MJ, Krebs N, Zubillaga MB, Weill R, Postaire E, Lysionek AE, Caro RA, Paoli TD, Hager A, Boccio J. Zinc and Diabetes Mellitus. Is there a need of zinc supplementation in diabetes mellitus patients? Biol Trace Elem Res. 2001. 81:215–228.

29. Simon SF, Taylor CG. Dietary zinc supplementation attenuates hyperglycemia in db/db mice. Exp Biol Med. 2001. 226:43–51.

30. Walter RM, Uriu-Hare JY, Olin KL, Oster MH, Anawalt BD, Critchfield JW, Keen CL. Copper, zinc, manganese, and magnesium status and complications of diabetes mellitus. Diabetes Care. 1991. 14:1050–1056.

31. Yoon JS. Zinc status and dietary quality of type 2 diabetic patients: implication of physical activity levels. Nutrition Research and Practice. 2008. 2:41–45.

32. Yoon JS, Lee JH. A suggestion to improve zinc status of type 2 diabetic women: relation among zinc, protein and phytate intake. Journal of Korean Dietetic Association. 2007. 13:301–310.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download