Abstract
BACKGROUND/OBJECTIVES
This study was performed to measure fat-soluble vitamins and minerals in breast milk of Korean lactating mothers who exclusively breastfed their babies.
SUBJECTS/METHODS
Breast milk samples were collected from 334 mothers. Concentrations of retinol and α-tocopherol were analyzed by high performance liquid chromatography ultraviolet spectrometry while concentrations of minerals were measured by inductively coupled plasma optical emission spectrometry.
RESULTS
Retinol and α-tocopherol contents of breast milk were 39.58 ± 19.64 µg/dL and 0.23 ± 0.13 mg/dL, respectively. Average sodium, potassium, calcium, phosphorus, and magnesium levels in breast milk were 11.11 ± 5.16, 38.56 ± 9.01, 27.87 ± 6.10, 13.56 ± 3.30, and 3.05 ± 0.65 mg/dL, respectively. Contents of trace elements such as iron, zinc, copper, and manganese were 40.26 ± 46.21, 98.40 ± 62.47, 24.09 ± 9.03, and 0.90 ± 1.63 µg/dL, respectively. Fat-soluble vitamin concentration was positively correlated with total fat in milk samples, but no significant differences were observed in levels of retinol, α-tocopherol, or minerals based on whether or not lactating women were taking dietary supplements.
Human breast milk contains essential nutrients and biologically active components [1] and plays an important role in determining the growth and neurocognitive development of infants [23]. Human milk from healthy and well-nourished women is as the healthiest for feeding healthy infants during the early stages of life [4]. Correspondingly, the World Health Organization (WHO) [5] recommends mothers worldwide to exclusively breastfeed infants up to 6 months of age, and this recommendation is accepted by numerous countries [67] as well as South Korea [8].
Despite recent heightened interest in breastfeeding practices, there is a scarcity of available reports on the micronutrient composition of human milk in Korea. Most studies on the micronutrient contents of human milk in Korea were performed in the 1980s and 1990s [91011] and involved only small sample sizes. Han et al. [12] reported changes in zinc concentrations during lactation, and other investigators have reported increased incidences of anemia and vitamin D deficiency among breastfed infants due to low iron and vitamin D levels in breast milk [1314151617].
Korea has experienced tremendous changes in anthropometry, diet, and lifestyle behaviors, which may have influenced the micronutrient composition of breast milk. Certain micronutrients are homeostatically regulated and maintained at constant levels, whereas others can vary due to lifestyle behaviors such as body mass index (BMI) [18], socioeconomic status [19], food consumption patterns [20], and use of dietary supplements [21] in lactating women. Compared with 20 years ago, a report from a recent national level dietary survey showed that the proportion of the general population in Korea consuming nutritional supplements has increased [22]. New and improved methods using high performance liquid chromatography (HPLC) and inductively coupled plasma with high sensitivity detectors have been developed and adopted by the Association of Official Analytical Chemists for analysis of vitamins and minerals in human milk. All of these factors now demand new determination of the micronutrient composition in breast milk from Korean lactating women.
Determination of the micronutrient composition in human breast milk is important since breast milk provides essential vitamins and minerals essential for the survival, growth and development, and optimum health and well-being of infants. Here, we report the concentrations of selected vitamins and minerals in mature milk of Korean lactating women (n = 334) who were exclusively breastfeeding their babies. We also compared micronutrient levels among breast milk samples from lactating mothers regardless of dietary supplement consumption.
A total of 546 lactating women were recruited from October 2012 to March 2015 through an online site. Study participants were mothers living in eight metropolitan cities [Seoul (n = 192), Busan (n = 17), Daejeon (n = 12), Daegu (n = 11), Gwangju (n = 3), Incheon (n = 42), Ulsan (n = 2), Jeju (n = 2)] and 42 smaller cities from five provinces [Gyeonggi, 26 cities (n = 241); Gangwon, one city (n = 2); Chungcheong, five cities (n = 9); Gyeongsang, eight cities (n = 11); Jeonla, one city (n = 2)]. Of these women, we excluded 27 women whose pregnancy lasted less than 37 or greater than 42 weeks, nine women who delivered infants weighing < 2.5 kg or > 4.5 kg, 15 women whose infant's age was < 30 days old or > 360 days old at sample collection, 157 women who did not exclusively breastfeed, and four women without data on use of dietary supplements. Thus, after all exclusions, 334 women and their babies were included in this study.
The study protocol was approved by the Institutional Review Board (0627-201408-HRBR-002-03) at Maeil Asia Human Milk Research Center, and all subjects provided their written informed consent to participate in the study. The method used to survey for general characteristics has been described in detail elsewhere [23]. Subjects were asked if they were currently taking any dietary supplements such as vitamins or minerals, and users were asked to report details regarding brand names and frequency of consumption.
Details on the collection (150 mL) of breast milk samples have been described previously [23]. Retinol and α-tocopherol were analyzed using the Nanospace SI-2-HPLC (Shiseido, Tokyo, Japan) photodiode array detector (Thermo Scientific Accela PDA 80 Hz Detector, Thermo Fisher Scientific, San Jose, USA) system. Breast milk was completely thawed and thoroughly mixed prior to aliquoting samples. A combination of 30 mL of ethyl alcohol and 1 mL ethyl alcohol solution of pyrogallol was added to 10 mL of homogenized breast milk and mixed. After adding 3 mL of 90% potassium hydroxide solution (w/v), the saponified mixture was transferred to a separating funnel, rinsed with water, and extracted five times with three fractions containing 100 mL of petroleum ether and two fractions containing 50 mL of petroleum ether. The combined ether extract was cleaned with 50 mL fractions of water, followed by addition of 2-3 drops of phenolphthalein until the aqueous layer appeared colored. The extract was passed through a layer of anhydrous sodium sulfate using a Whatman No.4 filter and then concentrated by rotary evaporator at 40℃. Finally, the evaporated residue was reconstituted with 5 mL of methanol, passed through a 0.45 µm filter, and then injected into the C18 column (4.6 × 250 mm, 5 µm) of the HPLC. All-trans retinol and α-tocopherol were detected at 298 nm, simultaneously. Limits of detection were 1 µg/dL and 0.01 mg/dL, respectively.
Minerals were analyzed by the inductively coupled plasma optical emission spectrometry (ICP-OES) method using an Optima 5300DV (Perkin Elmer Corp., Norwalk, CT, USA). Breast milk samples were added to the digester, followed by 4 mL of HNO3, and 1 mL of H2O2. The mixture was shaken gently and then incubated at room temperature. The digester was sealed tightly and placed in the container. Microwave conditions for the combustion procedure were 180℃ for 15 min, 180℃ for 35 min, and cooling for 3-4 hours. The volume was adjusted to 50 mL with deionized water after sample digestion. Specific wavelengths used for detection of each mineral were sodium, 589.592 nm; potassium, 766.490 nm; calcium, 317.947 nm; phosphorus, 213.617 nm; magnesium, 285.213 nm; iron, 238.204 nm; zinc, 206.200 nm; copper, 324.752 nm; and manganese, 257.610 nm. The limits of detection were 0.042, 0.055, 0.012, 0.050, and 0.021 mg/dL as well as 0.001, 0.003, 0.010, and 0.010 µg/dL, respectively.
The data were expressed as mean ± standard deviation (SD) for continuous variables or as numbers and percentages for categorical variables. One-way analysis of variance (ANOVA) test was used to compare vitamin and mineral concentrations in breast milk in each lactation period, followed by Scheffe's post-hoc test. Student's t-test was employed to determine differences in vitamin and mineral concentrations in breast milk between supplement users and non-users. General linear model (GLM) test was performed to analyze the differences in vitamin and mineral concentrations in breast milk among the two groups after adjustment for confounding factors, such as infant age, maternal BMI, and caloric intake. Partial correlation analyses, adjusted for confounding factors, were used to examine the relationships between retinol and α-tocopherol as well as fat concentration in breast milk. All analyses were performed using SAS 9.3 software (SAS Inc., Cary, NC, USA). The level of significance was set at P < 0.05.
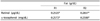
Our lactating women were aged 31.7 ± 3.1 years, and average BMI was 22.1 ± 3.1 kg/m2 (Table 1). Approximately 50.6% of lactating women took dietary supplements, and the proportion of dietary supplement users did not significantly differ with the infant age group [30-179 days (51.1%) vs 180-360 days (48.6%)] (data not shown).
The average energy content of mature milk (30-360 days) was 62.26 ± 11.95 kcal/dL, and the mean macronutrient concentrations were 6.96 ± 0.40 g/dL for lactose, 1.19 ± 0.26 g/dL for protein, and 3.30 ± 1.42 g/dL for fat (Table 2). Retinol and α-tocopherol contents were 39.58 ± 19.64 µg/dL and 0.23 ± 0.13 mg/dL, respectively. Potassium level (38.56 ± 9.01 mg/dL) was at least three times higher than that of sodium level (11.11 ± 5.16 mg/dL). Calcium and phosphorus contents were 27.87 ± 6.10 mg/dL and 13.56 ± 3.30 mg/dL, respectively, maintaining 2:1 ratio by weight, and magnesium level was 3.05 ± 0.65 mg/dL. Iron, zinc, copper, and manganese contents were 40.26 ± 46.21, 98.40 ± 62.47, 24.09 ± 9.03, and 0.90 ± 1.63 µg/dL, respectively.
Mean sodium and potassium levels varied according to lactation period; compared to milk samples at 1-2 months, sodium and potassium levels at 3 months, 4 months, 5 months, 6 months, and 7-11 months presented no significant differences. Zinc concentration was significantly lower in samples at 3 months, 4 months, 5 months, 6 months, and 7-11 months than those at 1-2 months and did not differ among samples at 3 months, 4 months, 5 months, 6 months, and 7-11 months. Copper concentration was significantly lower in samples at 4 months, 5 months, and 7-11 months than those at 1-2 months.
There were no differences in the levels of retinol, α-tocopherol, and minerals between supplement users and non-users after adjustment for confounding factors, such as infant age, maternal BMI, and caloric intake (Table 3).
Retinol and α-tocopherol concentrations were positively correlated with total fat contents of milk samples even when values were adjusted for infant age, maternal BMI, and caloric intake (P < 0.0001) (Table 4). Retinol and α-tocopherol levels were also highly correlated (r = 0.6-0.7).
Retinol content of breast milk was 39.6 µg/dL, which was similar to those of Korean (32 µg/dL, 47 µg/dL) [2425] and US (57 ± 25 µg/dL) women [26]. The mean vitamin E (α-tocopherol) content of breast milk was 226 µg/dL, which was low compared to those in Korean mothers from other reports, e.g. Lee et al. [24] (300 µg/dL); or Lee et al. [27] (351 µg/dL); or US mothers, 7.2 ± 4.2 µg/mL [26]. Retinol and α-tocopherol concentrations were positively correlated with total fat contents in milk samples even when values were adjusted for infant age, maternal BMI, and caloric intake. Retinol and α-tocopherol levels were also highly correlated (r = 0.6-0.7).
Due to tight regulation of maternal blood level, which determines uptake of vitamin A by the mammary glands, retinol content of mature breast milk has been reported to be stable without daily fluctuations due to the dietary intake of lactating women [28]. In contrast to the breast milk of US lactating women [26], the mean retinol concentration in this study was higher for supplement users than non-users. However, retinol values of the two groups were similar when adjusted for infant age, maternal BMI, and total energy intake.
Vitamin E level of breast milk from lactating mothers in Korea was similar to that of breast milk from motehrs in Canada (2.32 µg/mL) [29] but considerably lower-one third to one half-than that reported elsewhere [3031]. The α-tocopherol level was positively correlated with total fat level, which corroborates another investigation [32]. The α-tocopherol level is known to vary with the amount of fat in breast milk, particularly polyunsaturated fatty acids [33], which will be investigated in a further study.
Sodium and potassium contents in our milk samples were comparable to those of other reports from Korea [3435] as well as other nations [3637]. Interestingly, the potassium level (38.56 ±9.01 mg/dL) was at least three times higher than that of sodium (11.11 ±5.16 mg/dL). The molar ratio of sodium to potassium in breast milk was 0.46:1.10 for supplement users, which was significantly different from that for non-users (0.51:1.10). It is interesting that the molar ratio of sodium to potassium in human milk was approximately 2.0. Despite the known mass and molar ratios of sodium to potassium content in breast milk (13.7:46 and 2, respectively), the dietary reference intakes for Koreans (KDRI) [38] have always recommended a molar ratio of sodium to potassium intake of 1:1 for breastfed infants. Therefore, we may need to revise current standards and reestablish the recommended molar ratio of sodium to potassium as 1:2 based on the levels of these minerals present in breast milk. Sodium and potassium levels in breast milk from Japanese women were 13.9 ±7.2 and 10.7 ±6.9 mg/dL as well as 46.6 ±8.3 and 43.4 ±10.3 mg/dL, respectively, with molar ratios of 0.6:1.33 and 0.47:1.24 for lactation periods of 21-89 days and 90-180 days, respectively [36]. Considering Sandor's (1998) [39] equivalency law regarding metal requirements of living organisms, these may indeed be optimal intake ratios of sodium and potassium for survival and growth of human infants.
Calcium and phosphorus contents of our milk samples were 27.87 ±6.10 and 13.56 ±3.30 mg/dL, respectively, maintaining a 2:1 ratio by weight. These were very close to values reported previously for breast milk from Korean [4041] and Japanese mothers (23.0 ±7.4 and 13.8 ±3.7 mg/dL, respectively) [36]. The magnesium level of our milk samples was 3.05 mg/dL, which is similar to that reported by other investigators [1036].
Breast milk levels of iron, zinc, copper, and manganese were 40.26 ±46.21, 98.40 ±62.47, 24.09 ±9.03, and 0.90 ±1.63 µg/dL, respectively, which were comparable to previous levels in breast milk from Korean [124243] and Japanese mothers [36] but were highly variable by individual. Iron, zinc, and copper levels in mature milk from our study were considerably lower than those in transitional milk from South Korea in a recent study [44]. However, iron, zinc, and copper contents in breast milk (145 days postpartum) were higher than those from 9 month postpartum mothers from Honduras and Sweden (0.21 ±0.25 and 0.29 ±0.21, 0.70 ±0.18 and 0.46 ±0.26, and 0.16 ±0.21 and 0.12 ±0.22 mg/L for iron, zinc, and copper, respectively) [45]. Our findings that mineral contents of breast milk samples did not significantly differ by dietary supplementation use are similar to previous observations by other investigators who reported no significant correlation between iron, zinc, and copper levels in breast milk and maternal plasma [4546].
There are some limitations to this study. First, although our subjects were recruited from all regions in Korea, the results may be inadequate for interpretation and application to the general population since our data were generated through convenience sampling. Second, we did not obtain data on maternal dietary intake (e.g. food consumption pattern) or socioeconomic status, factors which might affect micronutrient levels in breast milk. Furthermore, many substances such as vitamins and minerals in breast milk are known to have diurnal variation [474849], which makes the time of day for milk collection important. In this study, the specific time of day at which breast milk was expressed and collected was not standardized. However, lactating women were asked to express their milk samples at times other than their baby's feeding time.
Our study results are in agreement with previous reports on the micronutrient composition of human milk. These data on breast milk composition have practical implications such as setting specific nutritional standards for infants and for designing an infant formula that closely resembles mother's breast milk. Further research is needed to explore different factors that might be associated with variations in micronutrient contents of human milk.
Figures and Tables
References
1. Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am. 2013; 60:49–74.
2. Isaacs EB, Fischl BR, Quinn BT, Chong WK, Gadian DG, Lucas A. Impact of breast milk on intelligence quotient, brain size, and white matter development. Pediatr Res. 2010; 67:357–362.

3. Rozé JC, Darmaun D, Boquien CY, Flamant C, Picaud JC, Savagner C, Claris O, Lapillonne A, Mitanchez D, Branger B, Simeoni U, Kaminski M, Ancel PY. The apparent breastfeeding paradox in very preterm infants: relationship between breast feeding, early weight gain and neurodevelopment based on results from two cohorts, EPIPAGE and LIFT. BMJ Open. 2012; 2:e000834.

4. ESPGAN committee on nutrition. Guidelines on infant nutrition. III. Recommendations for infant feeding. Acta Paediatr Scand Suppl. 1982; 302:1–27.
5. World Health Organization. Unicef. Global Strategy for Infant and Young Child Feeding. Geneva: World Health Organization;2003.
6. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012; 129:e827–e841.
7. Department of Health (GB). Infant feeding recommendation [Internet]. London: Department of Health;2003. cited 2015 June 1. Available from: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4096999.pdf.
8. Ministry of Health and Welfare, Korea Center for Disease Prevention and Control. National Health Insurance Service (KR). Manual of Pediatric Physical Examination 2015. Cheongju: Korea Center for Disease Prevention and Control;2015.
9. Bai HS, Lee DH, Ahn HS. Nutrient intakes of infants according to feeding pattern at 2 month age. Korean J Nutr. 1996; 29:77–88.
10. Ahn HS, Jeong JY. Ecological studies of maternal-infant Nutrition and feeding in urban low income areas: III. Infant's nutrient intakes and growth pattern. Korean J Community Nutr. 1998; 3:174–189.
11. Kim ES, Kim SB, Lee DH. The yields of volume, thiamin and riboflavin from the milk of cesarian-section women, and their ingestion in infants. Korean J Nutr. 1999; 32:83–89.
12. Han YH, Yon M, Han HS, Johnston KE, Tamura T, Hyun T. Zinc status and growth of Korean infants fed human milk, casein-based, or soy-based formula: three-year longitudinal study. Nutr Res Pract. 2011; 5:46–51.

13. Shin PJ, Bae CW, Choi YM. A comparative study of red blood cell indices and anemia by feeding patterns. J Korean Pediatr Soc. 1999; 42:1104–1110.
14. Choi EH, Jung SH, Jun YH, Lee YJ, Park JY, You JS, Chang KJ, Kim SK. Iron deficiency anemia and vitamin D deficiency in breastfed infants. Korean J Pediatr Gastroenterol Nutr. 2010; 13:164–171.

15. Kim YJ. Comparison of the serum vitamin D level between breastfed and formula-fed infants: several factors which can affect serum vitamin D concentration. Korean J Pediatr. 2013; 56:202–204.

16. Jin HJ, Lee JH, Kim MK. The prevalence of vitamin D deficiency in iron-deficient and normal children under the age of 24 months. Blood Res. 2013; 48:40–45.

17. Kang YS, Kim JH, Ahn EH, Yoo EG, Kim MK. Iron and vitamin D status in breastfed infants and their mothers. Korean J Pediatr. 2015; 58:283–287.

18. Qian L, Wang B, Tang N, Zhang W, Cai W. Polymorphisms of SLC30A2 and selected perinatal factors associated with low milk zinc in Chinese breastfeeding women. Early Hum Dev. 2012; 88:663–668.

19. Nikniaz L, Mahdavi R, Gargari BP, Gayem Magami SJ, Nikniaz Z. Maternal body mass index, dietary intake and socioeconomic status: differential effects on breast milk zinc, copper and iron content. Health Promot Perspect. 2011; 1:140–146.
20. Lönnerdal B. Effects of maternal dietary intake on human milk composition. J Nutr. 1986; 116:499–513.

21. Chierici R, Saccomandi D, Vigi V. Dietary supplements for the lactating mother: influence on the trace element content of milk. Acta Paediatr Suppl. 1999; 88:7–13.

22. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2014: Korea National Health and Nutrition Examination Survey (KNHANES VI-2). Cheongju: Korea Centers for Disease Control and Prevention;2015.
23. Chang N, Jung JA, Kim H, Jo A, Kang S, Lee SW, Yi H, Kim J, Yim JG, Jung BM. Macronutrient composition of human milk from Korean mothers of full term infants born at 37-42 gestational weeks. Nutr Res Pract. 2015; 9:433–438.

24. Lee SW, In YM, Choi JC, Yang HJ. Determination of the fatty acid and vitamin content of Korean human milk during lactation period. J Korean Soc Food Sci Anim Resour. 1997; 17:17–25.
25. Kim ES. Vitamin A intake of exclusively breast-fed infants in Cheongju and Anseong areas. Korean J Nutr. 2003; 36:743–748.
26. Kim Y, English C, Reich P, Gerber LE, Simpson KL. Vitamin A and carotenoids in human milk. J Agric Food Chem. 1990; 38:1930–1933.

27. Lee JS, Kim ES. Study on vitamin E intake of exclusively breast-fed infants. Korean J Nutr. 1998; 31:1440–1445.
29. Tijerina-Sáenz A, Innis SM, Kitts DD. Antioxidant capacity of human milk and its association with vitamins A and E and fatty acid composition. Acta Paediatr. 2009; 98:1793–1798.

30. Quiles JL, Ochoa JJ, Ramirez-Tortosa MC, Linde J, Bompadre S, Battino M, Narbona E, Maldonado J, Mataix J. Coenzyme Q concentration and total antioxidant capacity of human milk at different stages of lactation in mothers of preterm and full-term infants. Free Radic Res. 2006; 40:199–206.

31. Schweigert FJ, Bathe K, Chen F, Büscher U, Dudenhausen JW. Effect of the stage of lactation in humans on carotenoid levels in milk, blood plasma and plasma lipoprotein fractions. Eur J Nutr. 2004; 43:39–44.

33. Lima MS, Dimenstein R, Ribeiro KD. Vitamin E concentration in human milk and associated factors: a literature review. J Pediatr (Rio J). 2014; 90:440–448.

34. Choi KH, Moon J, Keum HK, Kim ES. Milk, sodium and potassium intaken of breastfed infants during lactation. Korean J Nutr. 1995; 28:612–619.
35. Lee JS, Lee YN, Kim ES. Study on sodium and potassium intakes of breast-fed infants during the first 5 months of lactation. Korean J Nutr. 2001; 34:23–29.
36. Yamawaki N, Yamada M, Kan-no T, Kojima T, Kaneko T, Yonekubo A. Macronutrient, mineral and trace element composition of breast milk from Japanese women. J Trace Elem Med Biol. 2005; 19:171–181.

37. Qian J, Chen T, Lu W, Wu S, Zhu J. Breast milk macro- and micronutrient composition in lactating mothers from suburban and urban Shanghai. J Paediatr Child Health. 2010; 46:115–120.

38. Ministry of Health and Welfare (KR). The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2015. Sejong: Ministry of Health and Welfare;2016. p. 659–666.
39. Sandor Z. Equivalency law in the metal requirement of the living organisms. Acta Aliment. 1998; 27:389–395.
40. Koo JO, Choi K. A longitudinal study of calcium and phosphorus intakes of Korean infants from 1 to 3 months in breast-fed vs formula-fed infants. Korean J Community Nutr. 2000; 5:273–279.
41. Kim ES, Keum HK. Protein, Ca, Mg and P intakes of breast-fed infants during lactation. Korean J Nutr. 2003; 36:942–949.
42. Kim ES, Cho KH. Iron, copper and zinc levels in human milk and estimated intake of the minerals by breast-fed infants during the early lactation. J East Asian Soc Diet Life. 2004; 14:27–33.
43. Moon SJ, Kang JS, Lee MJ, Lee JH, Ahn HS. A longitudinal study of micro-mineral concentration in human milk. Korean J Nutr. 1995; 28:620–628.
44. Choi YK, Kim JM, Lee JE, Cho MS, Kang BS, Choi H, Kim Y. Association of maternal diet with zinc, copper, and iron concentrations in transitional human milk produced by Korean mothers. Clin Nutr Res. 2016; 5:15–25.

45. Domellöf M, Lönnerdal B, Dewey KG, Cohen RJ, Hernell O. Iron, zinc, and copper concentrations in breast milk are independent of maternal mineral status. Am J Clin Nutr. 2004; 79:111–115.

46. Celada A, Busset R, Gutierrez J, Herreros V. No correlation between iron concentration in breast milk and maternal iron stores. Helv Paediatr Acta. 1982; 37:11–16.
47. Barkova EN, Nazarenko EV, Zhdanova EV. Diurnal variations in qualitative composition of breast milk in women with iron deficiency. Bull Exp Biol Med. 2005; 140:394–396.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download