Abstract
BACKGROUND/OBJECTIVES
Glutathione S-transferase (GST) forms a multigene family of phase II detoxification enzymes which are involved in the detoxification of xenobiotics by conjugating substances with glutathione. The aim of this study is to assess the antioxidative status and the degree of DNA damage in the subclinical hypertensive patients in Korea using glutathione S-transferase polymorphisms.
SUBJECTS/METHODS
We examined whether DNA damage and antioxidative status show a difference between GSTM1 or GSTT1 genotype in 227 newly diagnosed, untreated (systolic blood pressure (BP) ≥ 130 mmHg or diastolic BP ≥ 85 mmHg) subclinical hypertensive patients and 130 normotensive subjects (systolic BP < 120 mmHg and diastolic BP < 80 mmHg). From the blood of the subjects, the degree of the DNA damage in lymphocyte, the activities of erythrocyte superoxide dismutase, the catalase, and the glutathione peroxidase, the level of glutathione, plasma total radical-trapping antioxidant potential (TRAP), anti-oxidative vitamins, as well as plasma lipid profiles and conjugated diene (CD) were analyzed.
RESULTS
Of the 227 subjects studied, 68.3% were GSTM1 null genotype and 66.5% were GSTT1 null genotype. GSTM1 null genotype had an increased risk of hypertension (OR: 2.104, CI: 1.38-3.35), but no significant association in GSTT1 null genotype (OR 0.982, CI: 0.62-1.55). No difference in erythrocyte activities of superoxide dismutase, catalase, or glutathione peroxidase, and plasma TRAP, CD, lipid profiles, and GSH levels were observed between GSTM1 or GSTT1 genotype. Plasma levels of α-tocopherol increased significantly in GSTT1 wild genotype (P < 0.05); however, plasma level of β-carotene increased significantly in GSTT1 null genotype (P < 0.01). DNA damage assessed by the Comet assay was significantly higher in GSTM1 null genotype than wild genotype (P < 0.05).
Essential hypertension is a complex, multifactorial, polygenic disease whose genetic influences (i.e. genetic components) have not been revealed [1]. Oxidative stress is suspected to play an important role in the pathogenesis of hypertension, with many studies on the association between hypertension and oxidative stress being conducted [2345]. It was reported that the level of oxidative stress in patients with hypertension was higher than in individuals with normal blood pressure and that total antioxidative status (TAS), an antioxidant index, was low while the level of Malondialdehyde (MDA), a lipid peroxide produced by reactive oxygen, was high [34]. In previous studies, the plasma levels of antioxidants, such as α-tocopherol, β-carotene, total radical-trapping antioxidant potential (TRAP), and activity of glutathione peroxidase (GSH-Px), which is an erythrocyte antioxidant enzyme, were low in the hypertensive patient group compared to the control group, whereas the degree of DNA damage and lipid peroxidation were significantly higher [5]. In addition, blood pressure had an inverse correlation with plasma α-tocopherol and TRAP, and a positive correlation with the level of conjugated diene (CD) produced through DNA damage and lipid peroxidation. Thus, it was demonstrated that there is a strong correlation between blood pressure and biomarkers related to oxidative stress, and therefore between hypertension and oxidative stress.
Glutathione S-transferase is a phase II enzyme in the antioxidant system. It combines carcinogens entering the body with glutathione (GSH) to make a water-soluble compound and to excrete the compound from the body for detoxification. The GST family includes alpha (GSTA), mu (GSTM), kappa (GSTK), omega (GSTO), pi (GSTP), sigma (GSTS), theta (GSTT), and zeta (GSTZ), and it was reported that, in particular, GSTM1 and GSTT1 polymorphisms affected DNA damage and level of antioxidation [6789]. Enzyme polymorphism has been found in those enzymes and it varies depending on individuals. Thus, the susceptibility to disease does, too. In 43 of 95 literatures on a correlation between DNA damage and GST polymorphism, the effect of genotype was confirmed [10]. In one study including women in North Bohemia, GSTM1 genotype had an effect on DNA damage [11]. In another study investigating healthy adults, the effect of GST genotype was not shown [12]. Therefore, the effect of GST polymorphism on DNA damage is discordant.
It was reported that GST polymorphism was substantially associated with hypertension incidence frequency and hypertension risk factors and that GSTM1 rather than GSTT1 had a stronger association [1314]. In elderly patients with hypertension, the frequency of GSTM1 null genotype was significantly higher than that of GSTM1 wild genotype [13]. Saadat et al. [14] also reported that GSTM1 polymorphism rather than GSTT1 had a stronger effect on systolic blood pressure in the control group. However, some studies claimed that GSTT1 polymorphism rather than GSTM1 was more associated with hypertension and that both GSTM1 and GSTT1 polymorphism had an effect on hypertension [1516]. Marinho et al. [16] reported that there was no difference in GSTM1 genotype between patients with hypertension and individuals with normal blood pressure and that GSTT1 deletion had a protective effect against hypertension. Conversely, Oniki et al. [15] claimed that GSTA1, GSTM1, and GSTT1 deletion (null) were associated with the risk of hypertension. Incompatible results for a correlation between hypertension and GST polymorphism are still being reported, and therefore more studies are needed to reach a conclusion. In Korean studies, a correlation between GST polymorphism and the risk of bladder cancer [17] or etiology of coronary heart disease [18] was investigated but oxidative stress biomarkers related to GSTM1 and GSTT1 polymorphism in Korean patients with hypertension have not been studied yet. Hence, we investigated the effect of GST polymorphism on the incidence of hypertension in adults with borderline hypertension or hypertension who did not take medication, and we evaluated the difference in antioxidant nutriture and level of oxidative stress in patients with hypertension depending on GSTM1 and GSTT1 polymorphisms.
In the study, 227 adult patients with hypertension and 130 healthy adults were recruited from E University Hospital located in Daejeon. Posters for subject recruitment were distributed in the medical examination center of E University Hospital. The candidates were selected from the visitors whose systolic blood pressure was ≥ 130 mmHg or diastolic blood pressure was ≥ 85 mmHg and who had not taken any antihypertensive. Among them, the subjects who showed interest and gave written consent were finally included. The study was conducted according to a study protocol that passed the standards of the Institutional Review Board at Hannam University (2010-01k), South Korea. Sample size determined from below calculation formula.
Information regarding individual characteristics, health status, and lifestyle factors including smoking, alcohol, and exercise were collected by questionnaires. Blood pressure was the mean of two measurements in a seated position, using an automatic BP monitor (BP-8800C, Colin Electronics Co. Ltd., Komaki, Japan). The participants' weight, height, and waist and hip circumferences were measured using standard protocols. Body fat was measured by Bio-electrical Impedance Fatness Analyzer (Inbody 720, Biospace, Seoul, South Korea).
Blood samples drawn from the survey participants after a minimum of 8 h overnight fasting were put in the 10 mL heparinated sterile tube (Becton Dickinson and Co, Franklin Lakes, NJ). The process of blood separation was the same as in the previous study [5]. The erythrocyte suspension and plasma were divided for each analysis and kept at −80℃ in a freezer until used.
The GSTM1 and GSTT1 genotypes were determined as previously described without any modification [1319]. The β-globin primer pair (sense: 5′-CAACTTCATCCACGTTCACC-3′ and antisense: 5′-GAAGAGCCAAGGACAGGTAC-3′), which had not been deleted, was used as an internal control. The primers for amplifying the GSTM1 gene were (sense) 5'-CGCCATCTTGTGCTACATTGGCCGTC-3' and (antisense) 5'-TTCTGGATTGTAGCAGATCA-3'. The primers for the GSTT1 gene were (sense) 5'-TTCCTTACTGGTCCTCACATCTC-3' and (antisense) 5'-TCACCGGATCATGGCCAGCA-3'. The polymerase chain reaction (PCR) was performed in a 20 µL reaction mix containing 0.1 µg DNA, 10 pmol of each primer, 5 mM deoxyribonucleoside triphosphates, 0.5 Unit Taq polymerase(Takara rTaq), 200 mM Tris-HCl (pH 8.3), 500 mM KCl, and 30 mM MgCl2. After 2 minutes of pretreatment at 95℃ the reaction was subjected to 30 cycles of amplification at 94℃ for 1 minute, annealing at 64℃ for 1 minute, and 1 minute of elongation at 72℃. A final extension step of 7 min at 72℃ terminated the process. The products of the PCR amplification were separated by electrophoresis in a 1% agarose gel and stained with ethidium bromide (0.1 µg/mL). The internal standard fragment amplified from β-globin gene was 268 bp. A 215 bp fragment was amplified for the GSTM1 gene, and a 480 bp fragment was obtained for the GSTT1 gene. The absence of amplified product was consistent with the null genotypes. All reagents and chemicals for the genetic polymorphism were purchased from Bioneer (South Korea).
Plasma concentrations of vitamin C were measured spectrophotometrically by a chromogen using the 2,4-dinitrophenylhydrazine method [5]. Plasma levels of a-tocopherol, γ-tocopherol, α-carotene, and β-carotene were analyzed with high-performance liquid chromatography with fluorometric detection using a modified version of a previously described method [5].
Plasma total radical-trapping antioxidant potential (TRAP) was measured as the Trolox equivalent antioxidant capacity by the method of Rice-Evans and Miller [18].
Glutathione (GSH) was measured by modifying the DTNB [5,5′-dithiobis (2-nitrobenzoic acid)] method (QuantiChrom Glutathione Assay kit; BioAssay Systems, Hayward, CA, USA). The whole blood was diluted 20 times with distilled water to prepare samples, and reagent A 120 µL and sample 120 µL were mixed and centrifuged at 14,000 rpm for 5 minutes. Reagent A contained EDTA to prevent blood coagulation and to eliminate color development and proteins. After centrifugation, the supernatant was collected and placed in a 96-well plate, and then reagent B was added and left at room temperature for 25 minutes. The absorbance was measured at 412 nm using enzyme-linked immunosorbent assay and enzyme-linked immunospecific assay (ELISA), while the calibration curve was made using GSH as a standard.
The analysis of catalase, glutathione peroxidase (GSH-Px), and superoxide dismutase (SOD) in the red blood cell was carried out as previously described [20].
The alkaline Comet assay was conducted as described by Singh et al. [21], with little modifications. DNA damage of lymphocyte was observed by the 3 analysis indexes of tail length (TL), which is the distance of the DNA fragment moved from the nucleus, DNA in tail (% DNA), and tail moment (TM), which is the multiplied value of TL and % DNA. The DNA damage degree was measured by a total of 100 lymphocytes and 50 cells from each of the two replicate slides.
All the data were entered into Microsoft's Excel database, and the statistical tasks were performed with SPSS-PC+ statistics package (version 20.0). The mean and standard error of the mean (SE) were obtained for each item, and the mean difference among the 4 types of polymorphism of the 2 groups (GSTM1 wild and null types; GSTT1 wild and null types) was verified by independent t-test. The mean difference among the 3 groups was verified by Scheffé after one-way ANOVA, and all the statistical significance was evaluated at the level of α = 0.05. Multiple logistic regression analyses were used to evaluate the associations of frequency of GSTM1 and GSTT1 genotypes of the subjects and hypertension. Odds ratios and their 95% confidence intervals were computed to assess the strength of the association.
The general characteristics of the subjects are presented in Table 1. Among 357 subjects, 227 were hypertensive patients (average age: 41.9 ± 0.6, range: 26-63) and 130 were control subjects (average age: 40.6 ± 0.6, range 24-59). The proportion of male subjects was 80.2% in the hypertensive patient group and 76.9% in the control group and the proportion of female subjects was 19.8% and 23.1%. There was no significant difference between the two groups. Weight, body fat percentage (%), BMI, and WHR in the hypertensive patient group were significantly higher than those in the control group (P < 0.001). The proportion of smokers was 32.3% in the control group and, similarly, 30.0% in the hypertensive patient group. The mean history of smoking was 16.7 ± 1.0 years in the hypertensive patient group and 20.2 ± 1.2 years in the control group, which is significantly higher (P < 0.05). With consideration for smoking quantity and years of smoking, history of smoking (pack years) calculated based on one pack per year (20 cigarettes) was not different between the hypertensive patient group (13.8 ± 1.7 years) and the control group (14.4 ± 1.6 years). In addition, there was no difference in the rate of drinking, drinking quantity, rate of subjects who exercised regularly, and exercise hours.
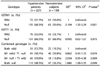
The frequency of GSTM1 and GSTT1 in the hypertensive patient group and the control group is shown in Table 2. The rate of GSTM1 null genotype was 68.3% in the hypertensive patient group and 50.0% in the control group, which shows a significant difference in the rate of null genotype and wild genotype (P = 0.001). However, the rate of GSTT1 null genotype was 66.5% in the hypertensive patient group and 66.9% in the control group, which reveals no significant difference. In the result of logistic regression analysis, the risk of hypertension in GSTM1 null genotype was 2.1-fold higher than in wild genotype (P = 0.001), and the risk in GSTT1 null genotype was 0.99-fold higher than in wild genotype (not significant). In addition, the risk of hypertension in GSTM1 and GSTT1 combined null genotype was 1.89-fold higher than in combined wild genotype (P = 0.049).
The level of plasma antioxidant vitamin depending on GST polymorphism in the hypertensive patient group is presented in Table 3. The level of α-tocopherol in GSTT1 wild genotype was significantly higher than in null genotype, and α-tocopherol in GSTM1 wild genotype was also higher than in null genotype but the difference was not significant. The level of β-carotene in GSTT1 null genotype was significantly higher than in wild genotype, whereas β-carotene in GSTM1 was not significantly different between null genotype and wild genotype. In addition, there was no significant difference in the level of vitamin C, γ-tocopherol, and α-carotene between GSTM1 or GSTT1 null genotype and wild genotype. The level of GSH and TRAP which shows plasma total antioxidant capacity was not significantly different between GSTM1 or GSTT1 null genotype and wild genotype.
The activity of erythrocyte antioxidant enzymes was investigated including catalase, superoxide dismutase, and glutathione peroxidase. In the hypertensive patient group, the activity of catalase, SOD, and GSH-Px was not significantly different depending on GST polymorphism between GSTM1 null genotype and wild genotype and between GSTT1 null genotype and wild genotype.
In the Comet assay, the degree of DNA damage was investigated by using three damage biomarkers such as DNA in tail, tail length (TL), and tail moment (TM). According to the tail length, the degree of DNA damage was significantly higher in GSTM1 null genotype than in wild genotype (Table 3, Fig. 1). TM and TD also showed a comparable trend to TL but there was no significant difference. The degree of DNA damage was not different between GSTT1 wild genotype and GSTT1 null genotype. Plasma TC, LDL-C, HDL-C, and TG were not significantly different depending on GSTM1 and GSTT1 genotypes. Plasma CD to determine the degree of oxidation for LDL was also not different depending on GSTM1 and GSTT1 genotypes.
GSTM1 and GSTT1 combined genotype was classified into three groups to investigate the level of biomarkers related to antioxidative activity and oxidative stress. In the result of plasma antioxidant vitamin, the level of α-tocopherol was the highest in both wild genotype than in either null genotype or both null genotype, whereas the level of TRAP determining plasma total antioxidant capacity was also significantly higher in both wild genotype than in either null genotype (Table 4, Fig. 1). There was no significant difference in other biomarkers among the three groups.
This study was conducted to investigate whether a high level of oxidative stress in patients with subclinical hypertension is different depending on GSTM1 and GSTT1 polymorphisms. In Korean patients with borderline hypertension, the risk of hypertension in GSTM1 null genotype was 2.1-fold higher than in wild genotype (OR: 2.104, P = 0.001), which suggests that GSTM1 genotype rather than GSTT1 genotype has a strong effect on the incidence of hypertension. Capoluongo et al. [13] reported that there was a correlation between GSTM1 null genotype and hypertension in the elderly when a difference depending on GSTM1 and GSTT1 polymorphism was investigated. In the study of Saadat et al. [14], GSTM1 polymorphism rather than GSTT1 had a stronger effect on the systolic blood pressure of adult subjects with normal blood pressure. Those results correspond with ours. However, Lee et al. [22] reported that GSTT1 genotype rather than GSTM1 genotype was more associated with hypertension in workers exposed to lead, while the risk of hypertension in GSTT1 wild genotype was 1.6-fold higher than in null genotype. In addition, Marinho et al. [16] suggested that the deletion of GSTT1 gene might be a protection factor against hypertension. Thus, there are also incompatible results with ours. A correlation between hypertension and GST polymorphism still varies, and therefore more studies are needed. Those opposed results might be caused by a different frequency of GST polymorphism depending on race and disease [23]. Thus, future studies with a larger group of Koreans will be needed to get a clear correlation with hypertension.
GST is a highly important enzyme to regulate oxidative stress, and therefore it is natural that biomarkers in the oxidative and antioxidative processes affect GST genotype [24]. In the result, plasma α-tocopherol level was significantly lower in GSTT1 null genotype than that in wild genotype. On the contrary, plasma β-carotene level was higher in GSTT1 null genotype. In most of the previous studies, GSTM1 and GSTT1 genotypes did not have an effect on plasma antioxidant vitamin. In some studies with healthy adults, smokers and non-smokers, plasma α-tocopherol, γ-tocopherol, α-carotene, and β-carotene were not different depending on GSTT1 genotype, as well as GSTM1 genotype [2425]. In this study, there was no correlation between plasma antioxidant vitamin and GSTM1 genotype while the level of α-tocopherol in GSTT1 wild genotype and plasma β-carotene in GSTT1 null genotype were higher. In the study of Tang et al. [26], plasma total antioxidative status (TAOS) in the patients with coronary artery disease was higher in both GSTM1 and GSTT1 wild genotypes but plasma glutathione (GSH) was significantly higher in GSTT1 null genotype. In general, GST null genotype leads to the reduction of GST enzyme to diminish detoxification against oxidants, with the antioxidant capacity consequently decreasing [26]. We expected increased plasma α-tocopherol in wild genotype, but increased plasma β-carotene in GSTT1 null type was unexpected. Based on the previous study which revealed overexpression of alpha, mu, and pi class transferase in the lack of GSTA4 and GSTZ1 in mice, a certain adaptive mechanism against extraneous agents is suspected [262728]. The mutant detoxification enzymes such as GSTs may result in the induction of other GST transferases and antioxidant proteins, which represents a compensatory to increase the intracellular levels of antioxidative products [26].
There are studies which suggest a certain effect of GST polymorphism on plasma vitamin C and, conversely, which suggests no effect. Jo et al. [23] reported that there was no difference in plasma vitamin C depending on GSTM1 and GSTT1 genotypes in young adults but Dusinská et al. [24] claimed that only plasma vitamin C among several antioxidant vitamins was affected by GST polymorphism in middle-aged male subjects in Slovakia. Plasma vitamin C was significantly higher in GSTM1 null genotype and GSTT1 wild genotype. On the contrary, Lin et al. [29] reported that the level of vitamin C was significantly higher in GSTM1 wild genotype than in null genotype in hemodialysis patients. Thus, a correlation between plasma vitamin C and GST polymorphism was not consistent.
Based on previous result, a correlation between GST polymorphism and antioxidant vitamins has not been determined clearly. Antioxidant vitamin nutriture of an individual substantially affected diet and, in particular, intake of dietary fat, excessive intake of polyunsaturated fatty acid, drinking, and smoking have a great effect on fat-soluble vitamins [30]. In this study, it was shown that the level of antioxidant vitamin in patients with hypertension was more affected by GSTT1 rather than GSTM1. However, it was not clear which GSTT1 genotype (null or wild) is better for antioxidant nutriture; therefore, further extensive studies to compare more biomarkers are needed.
The level of TRAP which shows plasma total antioxidant capacity and glutathione (GSH) was not significantly different depending on GSTM1 and GSTT1 polymorphisms. In the study of Hayek et al. [31], there was no difference in plasma total antioxidative status (TAS) depending on GSTM1 and GSTT1 genotypes. Jeon et al. [12] reported that TRAP was not significantly different depending on GSTM1 and GSTT1 genotypes, which corresponds with our result. In addition, Rahman et al. [32] reported that there was no significant difference in GSH between GSTT1 null genotype and wild genotype in both the chronic pancreatitis patient group and the control group, which supports our result. However, in the study of Tang et al. [26], plasma GSH was higher in GSTT1 null genotype in patients with coronary artery disease. Dusinska et al. [24] reported that the level of GSH was significantly high in GSTM1 wild genotype. GSH is an antioxidant which undergoes oxidation-reduction reaction in the body. GSH is combined with carcinogens by GST and then it is excreted for detoxification. When toxic substances enter the body, the activity of GST enzyme is enhanced and cell GSH increases rapidly. Thus, it is expected that the level of GSH would be low in null genotype where the activity of GST is reduced. There are, however, some previous studies with incompatible results. Thus, various biomarkers need to be analyzed to clarify an association between GST polymorphism and GSH.
The activity of erythrocyte SOD, GSH-Px, and catalase was not different depending on GSTM1 and GSTT1 polymorphisms and this result corresponds with some previous studies [24,27,33]. Bessa et al. [33] found that the activity of SOD and GSH-Px did not change depending on GSTM1 and GSTT1 genotypes in patients with hypertension. Dusinská et al. [24] reported that the activity of SOD, GSH-Px, and catalase was not different depending on GSTM1 and GSTT1 genotypes in healthy adults. In the previous case-control study with lung cancer patients, there was no difference in the activity of SOD and GSH-Px depending on GSTM1 and GSTT1 polymorphisms in both the patient group and the control group [27]. On the contrary, Jeon et al. [12] reported that the activity of GSH-Px was significantly higher in GSTM1 null genotype than in wild genotype in Korean adults. The activity of antioxidant enzyme was dissimilarly affected by the GST polymorphism based on the investigator. It may be because each investigator had different subjects. In addition, there is homeostatic regulation in the in vivo antioxidant system including antioxidant enzymes. Thus, when the body undergoes oxidative stress, a lot of antioxidant enzymes are used to overcome the event and then enzyme activity decreases. According to circumstances, antioxidant enzymes are more activated for homeostatic regulation to relieve oxidative stress [23]. Thus, antioxidant enzyme activity is not a generally proper biomarker to show the antioxidative status of the body [34].
DNA damage in the patients with hypertension was significantly higher in GSTM1 null genotype than that in wild genotype. DNA damage is highly related to oxidative stress biomarkers and in the previous studies, oxidative stress-related parameters among patients with hypertension were lower in GSTM1 null genotype, which was expected [33]. However, studies on the correlation between the degree of DNA damage and GST polymorphism in patients with hypertension have been rarely conducted and, therefore, more studies are needed. In the study of Lin et al. [29], the degree of DNA damage based on 8-OHdG was higher in GSTM1 null genotype than in wild genotype in hemodialysis patients. Tang et al. [28] reported that the degree of DNA damage based on 8-OHdG was higher in GSTM1 null genotype and GSTT1 null genotype in infertile men with varicoceles in Northwestern China. However, in the study of Jeon et al. [12], there was no difference in the degree of DNA damage depending on GSTM1 genotype in healthy adults, whereas DNA damage was significantly higher in GSTT1 null genotype than in wild genotype, which does not correspond with our result. The study of Jeon et al. [12] recruited healthy adults unlike our study. If patients with high oxidative stress were investigated, the result would be different. In this study, the degree of DNA damage was affected by GSTM1 among patients with hypertension. In case of GSTM1 null genotype, enzyme activity might be lost or very low and, therefore, the detoxification of the products of oxidative stress would decrease compared to wild genotype, which leads to the increased degree of DNA damage.
The level of conjugated diene (CD) produced by oxidation of LDL was not significantly different between GSTM1 null genotype and wild genotype and between GSTT1 null genotype and wild genotype. The result corresponds with the study of Bessa et al. [33] which investigated the patients with hypertension. Besides hypertension, in the study of Suvakov et al. [35], the level of MDA which shows lipid peroxidation damage was not significantly different depending on GSTM1 and GSTT1 genotypes in hemodialysis patients. However, Hayek et al. [31] reported that the level of oxidized LDL in diabetes patients was significantly higher in GSTT1 wild genotype than that in null genotype, while Tang et al. [28] found that the level of MDA was significantly higher in GSTM1 and GSTT1 null genotypes in infertile men with varicoceles who lived in Northwestern China. In this study, the degree of DNA damage and the level of CD, which are biomarkers to determine oxidative stress, were investigated among patients with hypertension. In the result, the degree of DNA damage was different depending on the GST polymorphism while the level of CD was not. It may be because DNA damage rather than CD is a more sensitive biomarker to decide oxidative stress.
GSTM1 and GSTT1 combined genotype was classified into three groups: both wild, either null, and both null genotypes. In the level of antioxidation, α-tocopherol among antioxidant vitamins and plasma TRAP to determine total antioxidant capacity were the highest in both wild genotype. However, there was no difference in antioxidant enzyme activity, the degree of DNA damage, and the level of CD, TRAP, and GSH among three groups. In the study of Tang et al. [28], total antioxidant capacity (TAC) was the highest and MDA was the lowest in null/null genotype, which partially corresponds with our result. Silva et al. [36] compared the level of TEAC to determine plasma antioxidant capacity in both wild, null/wild, wild/null, and both null genotype; there was no significant difference, which is different from our result. In the study of Bessa et al. [33], the level of MDA, GSH, CAT, SOD, and GSH-Px among patients with hypertension was not significantly different among four GST genotype groups. In this study, the level of TRAP and α-tocopherol was the highest in both wild genotype, and therefore it could be suggested that the activity of both GSTM1 and GSTT1 rather than the activity of one of them enhances antioxidation. However, other biomarkers did not show this trend.
Decrease GSTM1 expression may reduce antioxidant defenses, resulting low GSTM1 levels may lead to increased superoxide formation and reduced nitric oxide bioavailability [37]. Endothelial dysfunction is defined as the imbalance between the production and bioavailability of endothelium-derived relaxing factors (EDRFs) and endothelium derived contractile factors (EDCFs), associated with increased bioavailability of oxygen reactive species (ROS) and decreased antioxidant capacity characterized as oxidative stress [38]. NO is an important mediator released by endothelial cells, and that is produced by NO synthases (NOS). Peroxynitrite(ONOO−) and hydrogen peroxide(H2O2) increase arginase activity/expression in the endothelialcells, this should lead to NOS uncoupling with reduced NO production and augmented superoxide anion(O2 −) production [39]. Decreased NO availability along with enhanced EDCFs production by ROS contribute to the endothelium dysfunction and impaired vascular relaxation in hypertension [38]. Further studies on the correlation between biomarkers and GST are needed.
There are some limitations in this study. Although the total number of subjects was large, the number of subjects in some genotype classes was small, and therefore it was not enough to see the difference in antioxidant biomarkers between GSTM1 and GSTT1 genotypes. In addition, the use of various biomarkers deeply related to the mechanism of hypertension was limited. Thus, studies with more subjects and various antioxidant biomakers are required.
In conclusion, when we investigated the antioxidative status in the borderline patients with hypertension depending on GST polymorphism, the risk of hypertension increased in GSTM1 null genotype. The degree of DNA damage was found to increase in GSTM1 null genotype. However, the difference might not be caused by the antioxidative status of the subjects, and the antioxidative status was partially affected by GSTT1 polymorphism rather than GSTM1. As a result, the patients with hypertension were more susceptible to oxidative stress in GSTM1 null genotype and, therefore, the susceptibility of the patients with hypertension for antioxidant nutriture and the level of DNA damage was affected by GST polymorphism. Based on the result, a high susceptibility to DNA damage in GSTM1 null genotype would facilitate a personalized design according to GST polymorphism in programs or nutrition intervention studies to decrease oxidative stress among patients with hypertension. In addition, the antioxidative status in the subjects with GSTM1 null genotype would be highly improved.
Figures and Tables
 | Fig. 1Level of plasma (A) TRAP, (B) β-carotene, (C) α-tocopherol and (D) lymphocyte DNA damage reflected by tail length according to the GSTM1/GSTT1 combined genotype, and each genotype in the hypertensive patients. Values with different letters within a row are significantly different at P < 0.05 after Scheffe test followed by ANOVA. *P < 0.05, **P < 0.01 |
References
1. Dominiczak AF, Negrin DC, Clark JS, Brosnan MJ, McBride MW, Alexander MY. Genes and hypertension: from gene mapping in experimental models to vascular gene transfer strategies. Hypertension. 2000; 35:164–172.
3. Ahmad A, Singhal U, Hossain MM, Islam N, Rizvi I. The role of the endogenous antioxidant enzymes and malondialdehyde in essential hypertension. J Clin Diagn Res. 2013; 7:987–990.

4. Gur M, Yildiz A, Demirbag R, Yilmaz R, Koçyigit A, Celik H, Aksoy N. Relationship between left ventricle geometric patterns and lymphocyte DNA damage in patients with untreated essential hypertension. Clin Biochem. 2007; 40:454–459.

5. Han JH, Lee HJ, Choi HJ, Yun KE, Kang MH. Association between oxidative stress and blood pressure in Korean subclinical hypertensive patients. Korean J Nutr. 2013; 46:126–136.

6. Hayes JD, Strange RC. Glutathione S-transferase polymorphisms and their biological consequences. Pharmacology. 2000; 61:154–166.

7. Rebbeck TR. Molecular epidemiology of the human glutathione S-transferase genotypes GSTM1 and GSTT1 in cancer susceptibility. Cancer Epidemiol Biomarkers Prev. 1997; 6:733–743.
8. Han JH, Lee HJ, Kim TS, Kang MH. The effect of glutathione S-transferase M1 and T1 polymorphisms on blood pressure, blood glucose, and lipid profiles following the supplementation of kale (Brassica oleracea acephala) juice in South Korean subclinical hypertensive patients. Nutr Res Pract. 2015; 9:49–56.

9. Cho MR, Han JH, Lee HJ, Park YK, Kang MH. Purple grape juice supplementation in smokers and antioxidant status according to different types of GST polymorphisms. J Clin Biochem Nutr. 2015; 56:49–56.

10. Pavanello S, Clonfero E. Biological indicators of genotoxic risk and metabolic polymorphisms. Mutat Res. 2000; 463:285–308.

11. Binková B, Lewtas J, Mísková I, Rössner P, Cerná M, Mrácková G, Peterková K, Mumford J, Meyer S, Srám R. Biomarker studies in northern Bohemia. Environ Health Perspect. 1996; 104:Suppl 3. 591–597.

12. Jeon GI, Park EJ. Effect of glutathione s-transferase polymorphisms on the antioxidant system. J Korean Soc Food Sci Nutr. 2007; 36:708–719.

13. Capoluongo E, Onder G, Concolino P, Russo A, Santonocito C, Bernabei R, Zuppi C, Ameglio F, Landi F. GSTM1-null polymorphism as possible risk marker for hypertension: results from the aging and longevity study in the Sirente Geographic Area (ilSIRENTE study). Clin Chim Acta. 2009; 399:92–96.

14. Saadat M, Dadbine-Pour A. Influence of polymorphism of glutathione S-transferase M1 on systolic blood pressure of normotensive individuals. Biochem Biophys Res Commun. 2005; 326:449–454.

15. Oniki K, Hori M, Takata K, Yokoyama T, Mihara S, Marubayashi T, Nakagawa K. Association between glutathione S-transferase A1, M1 and T1 polymorphisms and hypertension. Pharmacogenet Genomics. 2008; 18:275–277.

16. Marinho C, Alho I, Arduíno D, Falcão LM, Brás-Nogueira J, Bicho M. GST M1/T1 and MTHFR polymorphisms as risk factors for hypertension. Biochem Biophys Res Commun. 2007; 353:344–350.

17. Kim H, Kim WJ, Lee HL, Lee MS, Kim CH, Kim RS, Nam HM. A case-control study on the effects of the genetic polymorphisms of N-acetyltransferase 2 and glutathione S-transferase mu and theta on the risk of bladder cancer. Korean J Prev Med. 1998; 31:275–284.
18. Kim SJ, Kim MG, Kim KS, Song JS, Yim SV, Chung JH. Impact of glutathione S-transferase M1 and T1 gene polymorphisms on the smoking-related coronary artery disease. J Korean Med Sci. 2008; 23:365–372.

19. Bell DA, Taylor JA, Paulson DF, Robertson CN, Mohler JL, Lucier GW. Genetic risk and carcinogen exposure: a common inherited defect of the carcinogen-metabolism gene glutathione S-transferase M1 (GSTM1) that increases susceptibility to bladder cancer. J Natl Cancer Inst. 1993; 85:1159–1164.

20. Lee HJ, Park YK, Kang MH. The effect of carrot juice, β-carotene supplementation on lymphocyte DNA damage, erythrocyte antioxidant enzymes and plasma lipid profiles in Korean smoker. Nutr Res Pract. 2011; 5:540–547.

21. Park EJ, Kim JS, Jeon EJ, Kim HY, Park YK, Kang MH. The effects of purple grape juice supplementation on improvement of antioxidant status and lymphocyte DNA damage in Korean smokers. Korean J Nutr. 2004; 37:281–290.
22. Lee BK, Lee SJ, Joo JS, Cho KS, Kim NS, Kim HJ. Association of Glutathione S-transferase genes (GSTM1 and GSTT1) polymorphisms with hypertension in lead-exposed workers. Mol Cell Toxicol. 2012; 8:203–208.

23. Jo HR, Lee HJ, Kang MH. Antioxidative status, DNA damage and lipid profiles in Korean young adults by glutathione S-transferase polymorphisms. Korean J Nutr. 2011; 44:16–28.

24. Dusinská M, Ficek A, Horská A, Raslová K, Petrovská H, Vallová B, Drlicková M, Wood SG, Stupáková A, Gasparovic J, Bobek P, Nagyová A, Kováciková Z, Blazícek P, Liegebel U, Collins AR. Glutathione S-transferase polymorphisms influence the level of oxidative DNA damage and antioxidant protection in humans. Mutat Res. 2001; 482:47–55.

25. Block G, Shaikh N, Jensen CD, Volberg V, Holland N. Serum vitamin C and other biomarkers differ by genotype of phase 2 enzyme genes GSTM1 and GSTT1. Am J Clin Nutr. 2011; 94:929–937.

26. Tang JJ, Wang MW, Jia EZ, Yan JJ, Wang QM, Zhu J, Yang ZJ, Lu X, Wang LS. The common variant in the GSTM1 and GSTT1 genes is related to markers of oxidative stress and inflammation in patients with coronary artery disease: a case-only study. Mol Biol Rep. 2010; 37:405–410.

27. Reszka E, Wasowicz W, Gromadzinska J. Antioxidant defense markers modulated by glutathione S-transferase genetic polymorphism: results of lung cancer case-control study. Genes Nutr. 2007; 2:287–294.

28. Tang K, Xue W, Xing Y, Xu S, Wu Q, Liu R, Wang X, Xing J. Genetic polymorphisms of glutathione S-transferase M1, T1, and P1, and the assessment of oxidative damage in infertile men with varicoceles from northwestern China. J Androl. 2012; 33:257–263.

29. Lin YS, Hung SC, Wei YH, Tarng DC. GST M1 polymorphism associates with DNA oxidative damage and mortality among hemodialysis patients. J Am Soc Nephrol. 2009; 20:405–415.

31. Hayek T, Stephens JW, Hubbart CS, Acharya J, Caslake MJ, Hawe E, Miller GJ, Hurel SJ, Humphries SE. A common variant in the glutathione S transferase gene is associated with elevated markers of inflammation and lipid peroxidation in subjects with diabetes mellitus. Atherosclerosis. 2006; 184:404–412.

32. Rahman SH, Nanny C, Ibrahim K, O'Reilly D, Larvin M, Kingsnorth AJ, McMahon MJ. Genetic polymorphisms of GSTT1, GSTM1, GSTP1, MnSOD, and catalase in nonhereditary chronic pancreatitis: evidence of xenobiotic stress and impaired antioxidant capacity. Dig Dis Sci. 2005; 50:1376–1383.

33. Bessa SS, Ali EM, Hamdy SM. The role of glutathione S- transferase M1 and T1 gene polymorphisms and oxidative stress-related parameters in Egyptian patients with essential hypertension. Eur J Intern Med. 2009; 20:625–630.

34. Kang MH, Yun JS. The effects of exercise and other relating factors on the activity of erythrocyte antioxidant enzymes and plasma TRAP levels in male college students. Korean J Nutr. 2002; 35:30–36.
35. Suvakov S, Damjanovic T, Stefanovic A, Pekmezovic T, Savic-Radojevic A, Pljesa-Ercegovac M, Matic M, Djukic T, Coric V, Jakovljevic J, Ivanisevic J, Pljesa S, Jelic-Ivanovic Z, Mimic-Oka J, Dimkovic N, Simic T. Glutathione S-transferase A1, M1, P1 and T1 null or low-activity genotypes are associated with enhanced oxidative damage among haemodialysis patients. Nephrol Dial Transplant. 2013; 28:202–212.

36. Silva DG, Belini Junior E, Torres LS, Ricci Júnior O, Lobo CC, Bonini-Domingos CR, de Almeida EA. Relationship between oxidative stress, glutathione S-transferase polymorphisms and hydroxyurea treatment in sickle cell anemia. Blood Cells Mol Dis. 2011; 47:23–28.

37. Cruz-Gonzalez I, Corral E, Sanchez-Ledesma M, Sanchez-Rodriguez A, Martin-Luengo C, Gonzalez-Sarmiento R. An association between resistant hypertension and the null GSTM1 genotype. J Hum Hypertens. 2009; 23:556–558.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download