Abstract
BACKGROUND/OBJECTIVES
Atopic dermatitis (AD), a chronic inflammatory skin disease, is accompanied by disruption of the epidermal lipid barrier, of which ceramide (Cer) is the major component. Recently it was reported that vitamin C is essential for de novo synthesis of Cer in the epidermis and that the level of vitamin C in plasma is decreased in AD. The objective of this study was to determine the associations among clinical severity, vitamin C in either plasma or epidermis, and Cer in the epidermis of patients with AD.
SUBJECTS/METHODS
A total of 17 patients (11 male and 6 female) aged 20-42 years were enrolled. The clinical severity of AD was assessed according to the SCORAD (SCORing Atopic Dermatitis) system. Levels of vitamin C were determined in plasma and biopsies of lesional epidermis. Levels of epidermal lipids, including Cer, were determined from tape-stripped lesional epidermis.
RESULTS
The clinical severity of patients ranged between 0.1 and 45 (mild to severe AD) based on the SCORAD system. As the SCORAD score increased, the level of vitamin C in the plasma, but not in the epidermis, decreased, and levels of total Cer and Cer2, the major Cer species in the epidermis, also decreased. There was also a positive association between level of vitamin C in the plasma and level of total Cer in the epidermis. However, levels of epidermal total lipids including triglyceride, cholesterol, and free fatty acid (FFA) were not associated with either SCORAD score or level of vitamin C in the plasma of all subjects.
Atopic dermatitis (AD) is a chronic inflammatory skin disease characterized by dried pruritic and eczematous skin lesions [1]. Genetic and environmental factors contribute to some extent, however an aberrant immune response of elevated immunoglobulin E (IgE) and impairment of the epidermal lipid barrier, in which ceramide (Cer), combined with triglyceride (TG), cholesterol and free fatty acid (FFA) forms intercellular lamellae, is frequently involved in the pathogenesis of AD [234]. As the main lipid of the stratum corneum (SC), the outermost layer of epidermis, Cer plays a critical role in maintaining the lamellae of the epidermal barrier, and depletion of Cer is thought be an etiological factor for impaired integrity of the epidermal barrier in AD [567]. During differentiation of the epidermis, Cer is synthesized de novo with the enzymatic condensation of serine and palmitoyl-CoA to sphingoid bases by serine palmitoyl transferase (SPT), followed by hydroxylation and esterification of long-chain FA by ceramide synthase (CerS) [8]. Several dietary factors including essential fatty acid [9], vitamin D [10], calcium [11], and vitamin C [1213] play a role in the epidermal differentiation process. Of these, calcium has received much interest as a putative epidermal differentiation factor; however, the 0.07-1.2 mM calcium gradient from the basal layer to the granular layer of the epidermis does not extend to the SC [11]. As a cofactor, vitamin C increases the activity and expression of CerS for hydroxylation of sphingoid bases and long-chain FA for de novo Cer synthesis in the SC. Recent cutaneous studies have reported decreased levels of vitamin C in the plasma and dermis of patients with AD [1415], and inhibition of de novo Cer synthesis in lesional skin of AD [16]. However, information about the associations among vitamin C, Cer, and clinical severity of AD is limited. Therefore, in this study, we determined the clinical severity, vitamin C levels in plasma and epidermis, and Cer level in the epidermis of patients of AD and further examined their associations.
The study protocol was approved by the Clinical Research Institutional Review Board of K University Hospital (KMC IRB 1235-02). Participants met the following criteria: nonsmokers; not suffering from acute and serious chronic diseases other than AD; not taking systemic or topical medications for at least 2 months prior to this study; not taking dietary supplements such as vitamins, antioxidants, and minerals. A total of 17 patients (11 male and 6 female) ranging in age from 20 to 42 years, who had AD with no other history of skin disease as determined through clinical and histological assessment, were enrolled and provided informed consent. Body mass index (BMI) was calculated using the equation: weight (kg)/height (m2).
Of 17 patients, 10 patients (9 male and 1 female) provided informed consent for skin biopsy of lesional epidermis. Using a 4-mm punch, biopsies were obtained from the lesional skin of the lower extremities, back, or arms. The epidermis was separated from whole-skin biopsies by overnight incubation at 4℃ in a 1:1 (v/v) mixture of dispase solution (Dispase II, Roche Diagnostics, Mannheim, Germany) and Hank's balanced salt solution (HBSS, Life Technologies, Grand Island, NY, USA). The separated epidermis for vitamin C analysis was stored at -80℃ for up to 1.5 months [17].
The severity of AD was assessed according to the SCORAD (SCORing Atopic Dermatitis) system, which computes scores on a scale of 0-83 using the following algorithm: SCORAD=A/5 +7(B/2), in which A is the percentage of body area affected by lesions as determined by the "Rule of Nines" and B is intensity scored on a relative scale from 0 to 3 for each of the following six signs: redness, swelling, oozing/crusting, scratch marks, skin thickening (lichenification), and dryness [18]. The following cutoff values for objective SCORAD scores were suggested for rating the clinical severity of AD: mild, < 15; moderate, 15-40; and severe > 40 [18].
After fasting overnight, blood was collected and delivered to the laboratory on the same day. Routine biochemical variables for nutritional status were analyzed, and factors related to AD diagnosis, including erythrocyte sedimentation rate (ESR), anti-streptolysin (ASO) level, and immunoglobulin E (IgE) level [219], were determined using routine methods at the Department of Laboratory Medicine at K University Hospital (Seoul, Korea).
Blood was collected in heparin-treated test tubes. Plasma was separated by centrifugation at 1,000 × g for 15 min at 4℃ and stored at -80℃ within 1.5 months (the same storage period of the epidermis) with no intermediate thawing/refreezing [1720]. One volume of plasma was mixed with two volumes of 90% methanol (MeOH) in H2O containing 0.05% ethylenediaminetetraacetic acid (EDTA), incubated for 10 min at 4℃, and supernatant was collected after centrifugation at 1,000 × g for 8 min at 4℃ [21]. Biopsied epidermis was homogenized with ice-cold 90% MeOH in H2O containing 1mM EDTA, 50 µM deferoxamine mesylate, and 1.5mM butylated hydroxytoluene bubbled with argon gas. After centrifugation at 3,000 × g for 3 min at 4℃, supernatant was collected for vitamin C analysis [17], and the debris was used for measurement of protein concentration using a modified Lowry method [22].
Vitamin C analysis of supernatants was performed using high performance liquid chromatography-electrochemical detection (HPLC-ECD) using a C18 column (3 × 250 mm, ID 5 µm, Shiseido, Yokohama, Japan), as described previously [21]. Vitamin C was eluted with isocratic mobile phase (MeOH: H2O, 25:75, v/v, pH4.8) containing 0.05 M sodium phosphate, 0.05 M sodium acetate, 189 µM dodecyl trimethyl ammonium chloride, and 36.6 µM tetraoctyl ammonium bromide at a flow rate of 0.4 ml/min, and detected at 254 nm in an electron capture detector (Shiseido). The separated vitamin C was identified and quantified by calibration curves using various concentrations of vitamin C (L-ascorbic acid: A7506, Sigma-Aldrich, St. Louis, MO, USA). Levels of vitamin C were expressed as either µmol/L (plasma) or µmol/mg protein (epidermis).
Epidermis was stripped from lesional forearms using tape strips (22-mm D-SQUAME Tape, Cu Derm, Dallas, TX, USA) and stored at -20℃ until further analysis. Corneocytes were removed from the tapes by sonication in MeOH, and the lipids were extracted in Folch solution (CHCl3: MeOH (2:1, v/v) as reported previously [23]. The top phase was used for measurement of protein concentration using a modified Lowry method [22]. The extracted lipids (lower phase) were subjected to high- performance thin layer chromatography (HPTLC) on 0.20-mm silica gel 60-coated plates (Merck, Darmstadt, Germany). Fractionation of TG, cholesterol, FFA, and total Cer was performed using the modified method of Uchida et al. [24]. Specifically, the samples applied on the plates were first eluted up to 2 cm using CHCl3: MeOH: H2O (10: 2.5: 0.25, v/v/v), up to 5 cm using CHCl3: MeOH: acetic acid (11.25: 1.25: 0.13, v/v/v), up to 7 cm using hexane: diethyl ether: acetone (2.5: 10: 0.63, v/v/v) and finally up to the top (9.5 cm) using hexane: diethyl ether (12: 0.37, v/v). Individual Cer species (Cer1-7) were fractionated first using CHCl3: MeOH: H2O (40:10:1, v/v/v) to 2 cm and again to 5 cm, followed by CHCl3: MeOH: acetic acid (47:2:0.5, v/v/v) to 8.5 cm and finally n-hexane: diethyl ether: acetic acid (30:15:0.5, v/v/v) to the top, as described previously [25]. The fractions containing TG, cholesterol, FFA, total Cer, or individual Cer species that comigrated with respective standards were treated with cupric acetate-phosphoric acid, heated to 160℃ for 15 min and scanned using a TLC III scanner (CAMAG, Muttenz, Switzerland). Levels of fractionated lipid were expressed as µg/mg protein.
Statistical analysis was performed using SPSS software (ver. 21.0, IBM, Armonk, NY, USA) and values were expressed as mean ± SEM (standard error of the mean). Pearson's correlation analysis was performed to determine associations among clinical severity, the level of vitamin C in plasma or epidermis, and epidermal lipid levels (Table 3: Fig. 1). Two-sided P-values < 0.05 were considered statistically significant.
A total of 17 patients (11 male, 6 female) aged between 20 and 42 years participated in this study. The mean age of male and female subjects was mid to late 20s, and BMI was in the normal range. Based on SCORAD scores, male subjects had moderate to severe AD, while female subjects had mild to moderate AD (Table 1). In routine biochemical analysis of blood, the means and the minimum-maximum ranges for all variables of nutritional status in male and female subjects were within the normal ranges (Table 2). In analysis of factors related to AD diagnosis, ESR and ASO were still within the normal ranges; however, the means and the maximum levels of IgE were highly elevated above the normal range in both male and female subjects.
Detailed data on SCORAD scores, vitamin C level in the plasma or epidermis, and epidermal lipid levels in individual subjects are shown in Table 3. The SCORAD scores of male subjects ranged between 15.0 and 45.0, corresponding to moderate to severe AD, while scores of female subjects ranged between 0.1 and 18.5, indicating mild to moderate AD. Vitamin C levels in the plasma of male subjects ranged between 6.84 and 29.72 (µmol/L), and showed inverse association with SCORAD scores (r = -0.621, P = 0.041). Vitamin C levels in the plasma of all subjects ranged between 6.84 and 31.34 (µmol/L), and despite no association between SCORAD score and vitamin C levels in the plasma of female subjects, a significant inverse association of these two parameters was observed for all subjects (r = -0.512, P = 0.035). The mean level of vitamin C in lesional epidermal biopsies of 10 subjects was higher than that in plasma, but there was no association between SCORAD score and vitamin C levels in the epidermis.
Vitamin C is a cofactor of CerS, an enzyme for de novo synthesis of Cer, the major component of the epidermal lipid barrier, which is frequently implicated in the pathogenesis of AD [234], therefore we reasoned that altered levels of epidermal lipids might also be associated with the clinical severity of AD. However, analysis of epidermal lipids showed that the levels of epidermal total lipids including TG, cholesterol, FFA, and Cer [234], were not associated with clinical severity of AD (Table 3). When epidermal total lipids were further fractionated, level of FFA (r = 0.612, P = 0.045) showed positive association, and level of total Cer (r = -0.667, P = 0.025) showed inverse association with SCORAD score in male subjects. In addition, levels of total Cer (r = -0.659, P = 0.004) and Cer2 (r = -0.706, P = 0.002), the major Cer species in epidermis [26], showed inverse association with SCORAD score in all subjects. Other Cer species, including Cer1 and Cer3-7, were fractionated as minor Cer species, but were not associated with SCORAD score (data not shown). Other major epidermal lipids, including TG and cholesterol, showed no association with SCORAD score. Together, these data indicate that levels of total Cer, particularly Cer2 in the epidermis as well as level of vitamin C in the plasma, were negatively associated with clinical severity (mild to severe) of AD in all subjects. Level of FFA in the epidermis showed a positive association in cases of moderate to severe AD in male subjects.
In contrast to the positive association of epidermal FFA with SCORAD score in male subjects with moderate to severe AD, an inverse association of either vitamin C level in the plasma or Cer level in the epidermis with SCORAD score was observed in all subjects with mild to severe AD. Therefore, we further examined the association between vitamin C in plasma and epidermal Cer (Fig. 1). A decreased level of vitamin C in plasma showed positive association with a decrease in total Cer of epidermis (r = 0.528, P = 0.029). Although Cer2, the major Cer species in the epidermis, showed inverse correlation with SCORAD score of all subjects, there was no association between vitamin C level in plasma and epidermal Cer2 level. These results indicate that as the clinical severity of AD progressed, vitamin C level in the plasma decreased in parallel with a decrease in total Cer of epidermis.
In AD, abnormal immune responses increase the levels of cytokines such as IL-2, leading to increased generation of reactive oxygen species (ROS) and lipid peroxides such as malondialdehyde [15]. As protection against these harmful factors, antioxidants such as vitamin C and E, and glutathione function as proton (H+) acceptors and directly neutralize these factors. This antioxidant function may explain the low levels of vitamin C and elevated levels of malondialdehyde in the plasma of patients with AD [14]. On the other hand, vitamin C levels in the plasma of adult patients with AD and healthy subjects are similar, but vitamin C levels in the dermis of patients with AD are significantly lower than those of healthy subjects [15], suggesting an association between the pathogenesis of AD and vitamin C level either in plasma or skin. Compared to a normal vitamin C range of 25-80 µmol/L in the plasma of healthy subjects [1527], 14 of 17 AD subjects (82.4%) in the current study had a plasma vitamin C level of < 25 µmol/L; only 3 of 17 subjects with mild to moderate AD had a normal vitamin C level of > 25 µmol/L, while two subjects with severe AD had extremely low plasma vitamin C levels (8.24 and 12.30 µmol/L, respectively). These results, coupled with the inverse association between vitamin C levels in plasma and SCORAD scores of all subjects, indicate that as the clinical severity progressed from mild to severe AD, the decrease in vitamin C level in the plasma was further aggravated. Alterations in dietary intake, gastrointestinal absorption, renal excretion, or antioxidant utilization of vitamin C could explain the low vitamin C levels in the plasma of AD patients [27], however this remains to be elucidated in future studies. In contrast to vitamin C level in plasma, there was no association of vitamin C level in epidermis with clinical severity of AD. Epidermal biopsies were obtained for a limited SCORAD range from moderate to severe AD and mostly from male subjects, which might explain the lack of association between clinical severity of AD and vitamin C level in epidermis. Vitamin C analysis in epidermal biopsies from patients with mild AD and large scale analyses of vitamin C levels in epidermal biopsies from patients with mild to severe AD should be included in future studies.
In addition to vitamin C level in plasma, the levels of total Cer and Cer2 in the epidermis were negatively associated with clinical severity ranging from mild to severe AD (all subjects) or from moderate to severe AD (male subjects). Levels of epidermal lipids other than total Cer and Cer2 were not associated with mild to severe AD, which is consistent with a previous study that reported no significant difference in total skin surface lipid content between AD patients and normal subjects [28]. Decreases in the level of Cer are associated with dryness and epidermal barrier disruption in AD [6]. Regarding Cer metabolism, extremely high activities of ceramidase, an enzyme of Cer degradation or of sphingomyelin (SM) deacylase and glucosylceramide (GC) deacylase, enzymes that hydrolyze GC and SM, two major precursor lipids of Cer generation, have been demonstrated to be metabolic features leading to decreased levels of Cer in AD [29]. Decreased expression of CerS is paralleled by reduced levels of total Cer in the epidermis of AD [30]. In male subjects with moderate to severe AD, levels of FFA in epidermis were positively associated with clinical severity. This association was not observed in female subjects with mild to moderate AD, suggesting that the increased levels of FFA become more relevant with progression of AD to more than moderate severity. The negative association of either total Cer or Cer2 in epidermis with clinical severity of AD, together with previous reports of decreased Cer generation and elevated Cer degradation in AD [6], suggests that the decreased levels of total Cer or Cer2 may be an indicator of clinical severity of AD.
Although the SCORAD scoring system is used routinely in clinics, it remains a subjective evaluation, in which scores vary depending on the clinicians involved in evaluation. Epidermal lipid analysis is objective, but requires complicated procedures over a long period of time, emphasizing the need for objective and simple biomarkers that reflect the clinical severity of AD and the Cer level in the epidermis. As a cofactor of CerS in de novo Cer synthesis, which is similar as a cofactor of proline hydroxylation in collagen synthesis [31], vitamin C facilitates the hydroxylation of sphingoid bases and FA generating α-hydroxy FA, ω-hydroxy FA, or various sphingoid bases [1213], which are major structural moieties of Cer providing the driving force for lamellar integrity of the epidermal barrier [38]. In keratinocytes, the major cells of the epidermis, vitamin C treatment increases Cer generation and induces differentiation into normal SC [12]. Alterations in dietary intake, gastrointestinal absorption, renal excretion, or antioxidant utilization of vitamin C should be determined in order to explain the low vitamin C levels in the plasma of AD patients, however, we demonstrate for the first time that levels of vitamin C in the plasma and Cer in the epidermis decreased as the clinical severity of AD increased, and that there is a positive association between these two parameters, implying associations among plasma vitamin C, epidermal Cer, and the clinical severity of AD.
Figures and Tables
Fig. 1
Association of plasma vitamin C with total ceramide in the epidermis of subjects with atopic dermatitis
Vitamin C level in plasma was determined by high performance liquid chromatography-electrochemical detection (HPLC-ECD). Epidermal lipids of subjects with atopic dermatitis (AD) (n = 17) were collected by tape stripping and total ceramide (Cer) was fractionated by high-performance thin-layer chromatography (HPTLC). Association of plasma vitamin C with total Cer in the epidermis of subjects with AD was determined by Pearson's correlation analysis.
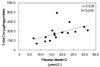
Table 2
Blood analysis of nutritional status in subjects with atopic dermatitis

1) Mean ± SEM; range (minimum-maximum) in parentheses
2) Values in parentheses indicate the normal range of each variable for male (M), female (F) or all subjects
3) AST, aspartate aminotransferase; ALT, alanine aminotransferase; BUN, blood urea nitrogen; ALP, alkaline phosphatase; WBC, white blood cell; ESR, erythrocyte sedimentation rate; ASO, anti-streptolysin O; IgE, immunoglobulin E
References
1. Addor FA, Takaoka R, Rivitti EA, Aoki V. Atopic dermatitis: correlation between non-damaged skin barrier function and disease activity. Int J Dermatol. 2012; 51:672–676.

2. Darlenski R, Kazandjieva J, Hristakieva E, Fluhr JW. Atopic dermatitis as a systemic disease. Clin Dermatol. 2014; 32:409–413.

3. Elias PM. Epidermal lipids, barrier function, and desquamation. J Invest Dermatol. 1983; 80:Suppl. 44s–49s.

4. Weerheim A, Ponec M. Determination of stratum corneum lipid profile by tape stripping in combination with high-performance thin-layer chromatography. Arch Dermatol Res. 2001; 293:191–199.

5. Di Nardo A, Wertz P, Giannetti A, Seidenari S. Ceramide and cholesterol composition of the skin of patients with atopic dermatitis. Acta Derm Venereol. 1998; 78:27–30.

6. Imokawa G, Abe A, Jin K, Higaki Y, Kawashima M, Hidano A. Decreased level of ceramides in stratum corneum of atopic dermatitis: an etiologic factor in atopic dry skin? J Invest Dermatol. 1991; 96:523–526.

7. Matsumoto M, Umemoto N, Sugiura H, Uehara M. Difference in ceramide composition between "dry" and "normal" skin in patients with atopic dermatitis. Acta Derm Venereol. 1999; 79:246–247.

8. Merrill AH Jr. De novo sphingolipid biosynthesis: a necessary, but dangerous, pathway. J Biol Chem. 2002; 277:25843–25846.

9. Garner WL, Oyatsu Y, Zuccaro C, Rodriquez JL, Smith DJ, Marcelo CL. The effect of essential fatty acid supplementation on keratinocyte replication. Prostaglandins Leukot Essent Fatty Acids. 1995; 52:349–355.

10. Zineb R, Zhor B, Odile W, Marthe RR. Distinct, tissue-specific regulation of vitamin D receptor in the intestine, kidney, and skin by dietary calcium and vitamin D. Endocrinology. 1998; 139:1844–1852.

11. Hennings H, Michael D, Cheng C, Steinert P, Holbrook K, Yuspa SH. Calcium regulation of growth and differentiation of mouse epidermal cells in culture. Cell. 1980; 19:245–254.

12. Uchida Y, Behne M, Quiec D, Elias PM, Holleran WM. Vitamin C stimulates sphingolipid production and markers of barrier formation in submerged human keratinocyte cultures. J Invest Dermatol. 2001; 117:1307–1313.

13. Ponec M, Weerheim A, Kempenaar J, Mulder A, Gooris GS, Bouwstra J, Mommaas AM. The formation of competent barrier lipids in reconstructed human epidermis requires the presence of vitamin C. J Invest Dermatol. 1997; 109:348–355.

14. Sivaranjani N, Rao SV, Rajeev G. Role of reactive oxygen species and antioxidants in atopic dermatitis. J Clin Diagn Res. 2013; 7:2683–2685.

15. Leveque N, Robin S, Muret P, Mac-Mary S, Makki S, Humbert P. High iron and low ascorbic acid concentrations in the dermis of atopic dermatitis patients. Dermatology. 2003; 207:261–264.

16. Macheleidt O, Kaiser HW, Sandhoff K. Deficiency of epidermal protein-bound omega-hydroxyceramides in atopic dermatitis. J Invest Dermatol. 2002; 119:166–173.

17. Shindo Y, Witt E, Han D, Epstein W, Packer L. Enzymic and nonenzymic antioxidants in epidermis and dermis of human skin. J Invest Dermatol. 1994; 102:122–124.

18. Kunz B, Oranje AP, Labrèze L, Stalder JF, Ring J, Taïeb A. Clinical validation and guidelines for the SCORAD index: consensus report of the European Task Force on Atopic Dermatitis. Dermatology. 1997; 195:10–19.

19. Wollenberg A, Zoch C, Wetzel S, Plewig G, Przybilla B. Predisposing factors and clinical features of eczema herpeticum: a retrospective analysis of 100 cases. J Am Acad Dermatol. 2003; 49:198–205.

20. Benzie I, Strain JJ. Effect of vitamin C supplementation on concentrations of vitamins C and E in fasting plasma. Asia Pac J Clin Nutr. 1999; 8:207–210.

21. Dhariwal KR, Hartzell WO, Levine M. Ascorbic acid and dehydroascorbic acid measurements in human plasma and serum. Am J Clin Nutr. 1991; 54:712–716.

22. Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951; 193:265–275.

23. Folch J, Lees M, Sloane Stanley GH. A simple method for the isolation and purification of total lipides from animal tissues. J Biol Chem. 1957; 226:497–509.

24. Uchida Y, Hara M, Nishio H, Sidransky E, Inoue S, Otsuka F, Suzuki A, Elias PM, Holleran WM, Hamanaka S. Epidermal sphingomyelins are precursors for selected stratum corneum ceramides. J Lipid Res. 2000; 41:2071–2082.

25. Kim H, Lee J, Cho Y. Dietary sericin enhances epidermal levels of glucosylceramides and ceramides with up-regulating protein expressions of glucosylceramide synthase, beta-glucocerebrosidase and acidic sphingomyelinase in NC/Nga mice. Nutr Res. 2012; 32:956–964.

26. Chen H, Mendelsohn R, Rerek ME, Moore DJ. Fourier transform infrared spectroscopy and differential scanning calorimetry studies of fatty acid homogeneous ceramide 2. Biochim Biophys Acta. 2000; 1468:293–303.

27. Benzie IF. Vitamin C: prospective functional markers for defining optimal nutritional status. Proc Nutr Soc. 1999; 58:469–476.

28. Angelova-Fischer I, Mannheimer AC, Hinder A, Ruether A, Franke A, Neubert RH, Fischer TW, Zillikens D. Distinct barrier integrity phenotypes in filaggrin-related atopic eczema following sequential tape stripping and lipid profiling. Exp Dermatol. 2011; 20:351–356.

29. Hara J, Higuchi K, Okamoto R, Kawashima M, Imokawa G. High-expression of sphingomyelin deacylase is an important determinant of ceramide deficiency leading to barrier disruption in atopic dermatitis. J Invest Dermatol. 2000; 115:406–413.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download