Abstract
The present study was conducted to document the association between plasma homocysteine levels and the presence of macrovascular angiopathy with food and nutrient intake patterns among patients with Type II diabetes mellitus in Korea. Plasma total homocysteine concentration was analyzed by HPLC-fluorescence detector method in 127 patients with non-insulin dependent diabetes mellitus. Logistic regression analyses were performed respectively to study the association of plasma homocysteine levels with clinical and dietary characteristics and macroangiopathy (MA). The average plasma homocysteine level of patients with MA was 14.2 µmol/l, which was significantly higher than that of patients without MA (11.4 µmol/l). The proportions of patients with MA showed a significant difference, being 32.3% in hyperhomocysteinemic (>14.0 µmol/l) patients and 13.5% in others with homocysteine levels lower than 14.0 µmol/l. Odds ratios for macroangiopathy by tertile increase of plasma homocysteine concentration were 1.633 (Q2) and 4.831 (Q3), when adjusted for age, sex, and cigarette smoking. Patients with MA consumed reduced amounts of vitamin B1, B2, and folate. The results indicate that the plasma homocysteine levels are significantly increased in NIDDM patients who have macroangiopathy. Dietary management such as increased fruits and vegetables and decreased potatoes and starches might be beneficial for the prevention of macroangiopathy in diabetic patients.
Non-insulin dependent diabetes mellitus (NIDDM) and its vascular complications are markedly increasing in Korea (Park et al., 1997) due to rapid industrialization process and economic growth, which entail changes in lifestyle and food habits. The management of vascular complications associated with the NIDDM, therefore, is becoming one of the critical public health concerns and issues in Korea.
Hyperhomocysteinemia has been recently identified as an important risk factor for cardiovascular (Hoogeveen et al., 1998), cerebrovascular, and peripheral vascular diseases. Hyperhomocysteinemia is found in up to 30-50% of patients with coronary artery disease and/or cerebrovascular disease (Robinson et al., 1995). With regard to the attribution of plasma homocysteine levels to the coronary artery disease risk, it has been estimated that a 5 µmol/l increase in the plasma homocysteine level is equivalent to an approximately 0.52 nmol/l (20 mg/dl) increase in the total cholesterol level, and this will result in a 20% increase in the coronary artery disease risk (Rees & Rodgers, 1993). Controlling the plasma levels of homocysteine thus becomes a critical step in the management of patients with NIDDM.
Numerous investigators have reported on homocysteine concentrations among patients with atherosclerotic vascular diseases and diabetic patients. It has been reported that type II diabetic patients who had proteinuria and macrovascular disease (Araki & Sako., 1993; Hoffman et al., 1998; Hultberg et al., 1991; Munshi et al., 1996; Vaccaro et al., 1997) had higher fasting homocysteine levels than nondiabetic control subjects. Most of the studies however, were conducted on western population and such studies on the Asians such as Koreans who show an increasing trend in the prevalence of NIDDM are limited.
Fruits and vegetables contain various micronutrients such as folic acid and other anti-oxidant vitamins which are beneficial for the maintenance of plasma homocysteine levels within the optimum range. Several studies reported inverse relationships between plasma homocysteine with intakes of B vitamins such as folate (Hatzis et al., 2006) and of fruits and vegetables (Paterson et al., 2006).
The purpose of this paper is to report the prevalence of hyperhomocysteinemia in NIDDM patients according to their respective vascular health status, and to document an association between food and nutrient intake and plasma homocysteine levels in these patients.
The study subjects were 127 NIDDM patients. We divided diabetic patients into two groups: (1) Those who have coronary artery disease, cerebrovascular disease, and peripheral vascular disease, were classified as patients with macroangiopathy(MA) complications, and (2) the rest, as patients with no macroangiopathy. The 24-hour recall dietary data were collected by a well-trained interviewer and analyzed using a Can-Pro (Korean Nutrition Society 2006) for nutrient and food group intake. This study was approved by the CHA University College of Medicine Human Investigation Review Committee. We included age, gender and BMI matched control subjects in the study. Any patient or control subjects who had known renal or other metabolic diseases or on any medications that might influence plasma homocysteine levels were excluded.
Blood samples were drawn from subjects after an overnight fast and were immediately centrifuged at 2,800rpm for 15 minutes at 4℃. The plasma was stored frozen at -70℃, and was analyzed for total homocysteine level. Plasma homocysteine was analyzed by the HPLC (Hitachi L-7100)-fluorescence detection method developed by Araki and Sako (1987). The plasma was thawed and treated with tri-n-butyl phosphine in dimethylformamide (DMFA) to release protein-bound homocysteine and to accomplish the reduction of mixed disulfides. Protein was precipitated with trichloroacetic acid and EDTA. After centrifugation at 3,000 × g for 5 minutes to remove protein, the supernatant was treated with ammonium 7-flurobenzo-2-oxa-1,3 diazole-4-sulfonate (SBD-F, Sigma, USA) to derivatize homocysteine and plasma thiols. Derivatized thiols were separated on a Phenomenex Luna C18 column (250 × 4.6 mm I.D., 5 µm particle size) and measured using a Waters 474 scanning fluorescence detector. The mobile phase was 0.1 M sodium phosphate buffer, pH 6.0 containing 5% methanol v/v). The plasma glucose and cholesterol concentrations were analyzed by an Autoanalyzer at the clinical laboratory.
All the results were statistically processed using a SAS program (SAS Institute, Inc., Cary, NC, USA). Patients were divided into (1) those having macrovascular disease and (2) those not, and were compared for their differences. One-way analysis of variance followed by Duncan's multiple range tests was performed and probability values less than 0.05 were considered statistically significant. Logistic regression analyses were performed to study the association of hyperhomocysteinemia with the risk of macroangiopathy. We calculated odds ratios (ORs) and 95% confidence intervals (CIs) by tertiles of plasma homocysteine levels with the lowest tertile as a reference category. Age, sex and cigarette smoking were all considered as potential covariates.
Diabetes mellitus patients were divided into two groups: (1) those having macrovascular complications were designated MA group and (2) those not having macrovascular complications, nMA group.
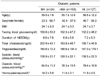
In the diabetic patients without macroangiopathy, the plasma homocysteine level was 11.4 ± 3.1 µmol/l. In the diabetic patients with macroangiopathy, however, the plasma homocysteine level was 14.2 ± 5.8 µmol/l, which was significantly higher than the values of the patients with MA and the control by 23% and 25%, respectively (Table 1). Both systolic and diastolic blood pressures were increased in patients with MA compared to those without MA complications. There were no significant differences in the mean age, gender, BMI, fasting blood glucose, and the years of NIDDM between the two groups of diabetic patients
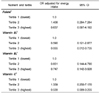
The result of the logistic regression analysis on the association between plasma homocysteine levels with the risk of macroangiopathy is shown in Table 2. We calculated odds ratios by tertiles of plasma homocysteine with the lowest tertile as a reference. When adjusted for age, gender, and cigarette smoking, the odds ratios for MA were 1.633 (95% CIs = 0.606-4.398) and 4.831 (95% CIs = 1.676-7.933) for Q2 and Q3, respectively.
There was no difference in intakes of macronutrients such as energy and protein, but intakes of micronutrients such as thiamine, riboflavin, and folate were reduced in patients with macroangiopathy compared to those without MA. The difference in folate intake was still present when folate intake was adjusted for energy intake.
In order to investigate the association between vitamin B intakes and macroangiopathy in diabetic patients, a logistic regression analysis was conducted. After adjustment for energy intake, dietary folate and vitamin B1 intakes were inversely associated with the risk of hyperhomocysteinemia as shown in the Table 3. Compared with subjects in the lowest tertile of intake, those in the highest tertile had a calorie-adjusted OR of 0.637 (95% CI = 0.097-4.192) and 0.055 (95% CI = 0.012-0.735), respectively. Also, dietary vitamin B2 and vitamin C intakes were inversely associated with the risk of hyperhomocysteinemia. Compared with subjects in the lowest tertile of intake, those in the highest tertile had a calorie-adjusted OR of 0.747 (95% CI = 0.142-3.928) and 0.539 (95% CI = 0.089-3.255), respectively. However, none of the logistic analysis data on the vitamin intake was statistically significant.
The result of the logistic analysis on the food group intake showed that the odds ratios for potatoes and starches and fruits were 2.804 (95% CI = 1.144-6.870) and 0.155 (95% CI = 0.057-0.422) when the data were adjusted for age, gender, energy intake, and cigarette smoking in patients with hyperhomocysteinemia.
We found that the plasma homocysteine levels in the diabetic patients with macroangiopathy were significantly higher compared to those in the patients with no macrovascular complications or the non-diabetic normal control subjects. Diabetic patients with vascular complications consumed less amounts of B vitamins such as vitamin B1, B2, and folate. When vitamin intakes were adjusted for energy intake, the difference in folate intake was found to be still significant. After adjustment for energy intake, dietary intakes of folate, thiamin, riboflavin and vitamin C were inversely associated with the risk of hyperhomocysteinemia.
In our study, the homocysteine level among the diabetic patients having the macrovascular disease was found notably high. In the study of 136 Japanese male and female non-insulin-dependent diabetes mellitus patients, Araki et al. (1993) reported that the concentration level of plasma homocysteine among the patients having macrovascular complications was higher than that among those having no macrovascular complications nor control. A study by Munshi et al. (1996) on the non-insulin dependent male patients under age 60, also, reported similar trends.
We showed that the intakes of vitamin B1, B2 and folate were significantly low among the diabetic patients with macrovascular complications. Among several nutrients that are known to affect the plasma homocysteine level, the intakes of riboflavin and folate were investigated with particular attention. As was found out, the mean riboflavin intake in the MA group was lower than the recommended intake level for riboflavin. The metabolism of riboflavin is closely linked to the metabolism of other B vitamins such as folate, pyridoxine, and niacin. The deficiency of riboflavin, therefore, could cause a secondary deficiency in folate (Tan et al., 1984), leading to an increase of plasma homocysteine level (Selhub et al., 1993a).
Our results also showed that the folate intake in all three groups was far from the 400 µg, the recommended amount of folate intake for Koreans (Korean Nutrition Society, 2005), and was in fact the lowest in the MA group. Folate plays an important role in the process of transmethylation and transsulfuration, and is required in the metabolic pathway of removing homocysteine (Ubbink, 1994). It has been reported that the poor folate state can cause an increase in the total homocysteine concentration in the plasma, thereby increasing the danger of developing vascular complications (Berwanger et al., 1995; Masser et al., 1994; Stampfer & Malinow, 1995). A sufficient supply of folate, on the other hand, can lower the homocysteine concentration, thereby decreasing the danger of developing vascular diseases (de Bree et al., 2001; Stampfer & Malinow, 1995). Insufficient intake of B vitamins like riboflavin, folate, vitamin B6, and vitamin B12 was shown to increase plasma homocysteine levels (Jacques et al., 2001; Selhub et al., 1993a; Selhub et al., 1993b).
The reasons for a higher mean homocysteine level observed in our diabetic subjects with MA might be attributed to their reduced intakes of riboflavin and folate, both of which can influence the plasma homocysteine levels. These findings strongly indicate that the intake of B vitamins that are known to influence homocysteine levels should be sufficiently increased for the diabetic patients to prevent vascular complications. From these results, we have come to a conclusion that a decreased level of folate intake causes an increase of homocysteine level in the blood, thereby leading to the complications of macrovascular disease.
In our study, the odds ratios for the presence of hyperhomocysteinemia was significantly decreased in patients whose consumption of fruits was in the highest quartile, confirming results of other investigators (Bogers et al., 2007; Hatzis et al., 2006). Fruits and vegetables contain numerous micronutrients and functional ingredients with anti-oxidant properties which are helpful in keeping the homocysteine levels low thereby enhancing vascular health status. Increased fruits and vegetable intake has been effective in the improvement of plasma folate and homocysteine levels (Bermejo et al., 2007). In the other study, however, 4-week of increased fruits and vegetable consumption by 200 g/d (133 g/d for fruits and juice and 64 g/d for vegetables) was not sufficient to change plasma folate and homocysteine concentrations (Bogers et al., 2007).
Studies on the effect of folate and homocysteine on vascular health of the diabetic patients need to receive more attention to identify dietary factors that are associated with vascular complications in these patients. We are pursing our investigations further on these matters and more results will be discussed in future reports.
Figures and Tables
Table 2
Odds ratios for macroangiopathy by tertile increase of plasma homocysteine concentration in diabetic patients

References
1. Araki A, Sako Y. Determination of free and total homocysteine in human plasma by high-performance liquid chromatography with fluorescence detection. J Chromatogr. 1987. 422:43–52.

2. Araki A, Sako Y, Ito H. Plasma homocysteine concentrations in Japanese patients with non-insulin-dependent diabetes mellitus: effect of parenteral methylcobalamine treatment. Atherosclerosis. 1993. 103:149–157.

3. Bermejo LM, Aparicio A, Andrés P, López-Sobaler AM, Ortega RM. The influence of fruit and vegetable intake on the nutritional status and plasma homocysteine levels of institutionalised elderly people. Public Health Nutr. 2007. 10:266–272.

4. Berwanger CS, Jeremy JY, Stansby G. Homocysteine and vascular disease. Br J Surg. 1995. 82:726–731.

5. Bogers RP, Dagnelie PC, Bast A, van Leeuwen M, van Klaveren JD, van den Brandt PA. Effect of increased vegetable and fruit consumption on plasma folate and homocysteine concentrations. Nutrition. 2007. 23:97–102.

6. De Bree A, Verschuren WMM, Blom HJ, Kromhout D. Association between B vitamin intake and plasma homocysteine concentration in the general Dutch population aged 20-65y. Am J Clin Nutr. 2001. 73:1027–1033.

7. Hatzis CM, Bertsias GK, Linardakis M, Scott JM, Kafatos AG. Dietary and other lifestyle correlates of serum folate concentrations in a healthy adult population in Crete, Greece: a cross-sectional study. Nutr J. 2006. 5:5.

8. Hofmann MA, Kohl B, Zumbach MS, Borcea V, Bierhaus A, Henkels M, Amiral J, Schmidt AM, Fiehn W, Ziegler R, Wahl P, Nawroth PP. Hyperhomocysteinemia and endothelial dysfunction in IDDM. Diabetes Care. 1998. 2:841–848.

9. Hoogeveen EK, Kostense PJ, Beks PJ, Mackaay AJC, Jakobs C, Bouter LM, Heine RJ, Stehouwer CDA. Hyperhomocysteinemia is associated with an increased risk of cardiovascular disease, especially in non-insulin-dependent diabetes mellitus a population-based study. Arterioscler Thromb Vasc Biol. 1998. 18:133–138.

10. Hultberg B, Agardh E, Andersson A, Brattstrom L, Isaksson A, Israelsson B, Agardh CD. Increased levels of plasma homocysteine associated with nephropathy, but not severe retinopathy in type I diabetes mellitus. Scand J Clin Lab Invest. 1991. 51:277. [Abstract].

11. Jacques PF, Bostrom AG, Wilson PWF, Rich S, Rosenberg IH, Selhub J. Determinants of plasma total homocysteine concentration in the Framingham Offspring cohort. Am J Clin Nutr. 2001. 73:613–621.

12. Korean Nutrition Society. Korean Dietary Reference Intakes. 2005. Seoul. Republic of Korea: Kookjin Publishing Co.
13. Konstantinova SV, Vollset SE, Berstad P, Ueland PM, Drevon CA, Refsum H, Tell GS. Dietary predictors of plasma total homocysteine in the Hordaland Homocysteine Study. Br J Nutr. 2007. 98:201–210.

14. Masser PA, Taylor LM, Porter JM. Importance of elevated plasma homocysteine levels as a risk factor for atherosclerosis. Ann Thorac Surg. 1994. 58:1240–1246.

15. Munshi MN, Stone A, Fink L, Fonseca V. Hyperhomocysteinemia following a methionine load in patients with non-insulin-dependent diabetes mellitus and macrovascular disease. Metabolism. 1996. 45:133–135.

16. Park JY, Lee KU, Kim CH, Kim HK, Hong SK, Park KS, Lee HK, Min HK. Past and current obesity in Koreans with non-insulin-dependent diabetes mellitus. Diabetes Res Clin Pract. 1997. 35:49–56.

17. Paterson E, Gordon MH, Niwat C, George TW, Parr L, Waroonphan S, Lovegrove JA. Supplementation with fruit and vegetable soups and beverages increases plasma carotenoid concentrations but does not alter markers of oxidative stress or cardiovascular risk factors. J Nutr. 2006. 136:2849–2855.

18. Rees MM, Rodgers GM. Homocysteinemia: association of a metabolic disorder with vascular disease and thrombosis. Thromb Res. 1993. 71:337–359.

19. Robinson K, Mayer EL, Miller DP, Green R, van Lente F, Gupta A, Kottke-Marchant K, Savon SR, Selhub J, Nissen SE, Kutner M, Topol EJ, Jacobsen DW. Hyperhomocysteinemia and low pyridoxal phosphate common and independent reversible risk factors for coronary artery disease. Circulation. 1995. 92:2825–2830.
20. Selhub J, Jacques PF, Wilson PWF, Rush D, Rosenberg IH. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. JAMA. 1993a. 270:2693–2698.

21. Selhub J, Jacques PF, Wilson PWF, Rush D, Rosenberg IH. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. J Am Med Assoc. 1993b. 272:2703–2708.

22. Stampfer MJ, Malinow MR. Can lowering homocysteine levels reduce cardiovascular risk? N Engl J Med. 1995. 332:328–329.

23. Tan PS, Wenlock RW, Buss DH. Folic acid content of the diet in various types of British household. Hum Nutr Appl Nutr. 1984. 38:17–22.
24. Ubbink JB, Vermaak WJH, Bissbort S. Rapid high performance liquid chromatographic assay for total homocysteine levels in human serum. J Chromatogr. 1991. 565:441–446.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download