Abstract
The purpose of this study was to examine the relationship between nutrient intake and bone mineral density (BMD) of elderly women in Daegu, Korea. In this study, the bone mineral densities of 101 elderly women in Daegu were measured, and their nutrient intake, dietary habits, and maternal factors were determined through a survey. The subjects were divided into the normal group, the osteopenia group, and osteoporosis group to find out if there is a correlation between bone mineral density and maternal factors, dietary habits, and nutrient intake through their T-scores, analyzed according to the standards of WHO. Classification by T-scores of the participants were the normal group 25.7%, the osteopenia group 39.6%, the osteoporosis group 34.7%. Menopause age of the osteoporosis group was lower, postmenopausal period was longer, and last delivery age was significantly higher than the normal group (p<0.05). Osteoporosis group had a lower percentage of 'everyday' fruit and vegetable intakes and higher percentage of 'never' dairy intake than of the normal group. Vitamin A, vitamin B1, and vitamin B2 intakes of participants in the osteoporosis group were lower than those in the normal group (p<0.05). In conclusion, nutritional education is necessary to encourage high intake of milk and vegetables and fruits along with calcium, vitamin A, B1, and B1 intakes and low intake of sodium for the prevention of elderly women's osteoporosis.
The rates of increase in the number of elderly people in Korea, or those aged 65 or above, against the total Korean population over the past years were very high: 5.7% in 1994, 7.2% in 2000, 8.3% in 2003, and 8.7% in 2004. People who are 65 years old or above now represent more than 7% of the country's total population, which signals the advent of an aging society, and the projection that people in this age bracket will comprise 14% of the country's population in 2022 indicates that Korea will already have an aged society in that year (Ministry of Health and Welfare, 2005). The truth of this matter would be readily seen if it would be considered that the average life expectancy of the women in Korea is 80.1 years, and that their postmenopausal life is almost over 30 years long (Ministry of Health and Welfare, 2005). After menopause, the secretion of the female hormone estrogen decreases, resulting in the risk of developing osteoporosis due to the loss of bone mass (Kim, 2001). No less than 1.3 million osteoporosis-related fracture cases occur in the U.S. every year, including 530,000 spine fractures, with the possibility of spine fractures for 1/3 of the women who are 65 years old or above (Gordon, 1988). The possibility of incurring an osteoporosis-related fracture in a whole lifetime was estimated to be about 40% (Preisinger et al., 1995), and the death rate due to osteoporosis-related fracture is higher than the death rate due to breast cancer or uterine cancer (Tenenhouse et al., 2000). This explains why osteoporosis and osteoporosis-related fractures are drawing a lot of attention as a health problem in the U.S. According to the report of NOF (National Osteoporosis Foundation, 2002), 44 million men and women aged 50 years and above were threatened by osteoporosis in 2002, 80% of which were females, and these numbers are expected to increase to 52 million in 2010 and to 61 million in 2020. Fracture incidence reportedly has race-based differences, and age-adjusted hip fracture incidence was lower for all three Asian-American groups than for whites. For females, the standardized fracture ratio relative to whites was 30.1 for Chinese, 73.2 for Japanese, and 52.8 for Koreans (Lauderdale et al., 1997).
According to a 2001 study on 50 to 79-year-old Japanese women, the prevalence rate of osteoporosis in that year for such women was 38% for the spine and 11.6% for the femoral neck (Iki et al., 2001). A study on Chinese women living in Hong Kong showed a significantly higher osteoporosis prevalence rate for older women: 10% for women in their fifties and 45% for those in their sixties (Ho et al., 2001).
There are no statistical data available on the prevalence rate of osteoporosis in Korea, but it is known that the bone mineral density of Korean women is about 10% lower than that of Western women (Kang, 1998), and that the rate of diminution of the Korean women's bone mineral density after menopause is higher than that of the women in other countries (Koh et al., 1992). In a study on 1,448 Korean women aged 40 years and above, the prevalence rates of osteoporosis were found to be 19.4%, 10.8%, and 6.7% for the spine, femoral neck, and total femur bone mineral density, respectively. In the case of the women who were 50 years old or above, the prevalence rates were 23.1%, 13.0%, and 7.6%, respectively (Lee et al., 2002). In addition, in a study on 1,020 Korean women who were in their premenopausal period, the prevalence of osteoporosis was found to be 9.8% for the spine and 1.4% for the femoral neck (Kim et al., 2002). The osteopenia was 30.7% for the spine and 24.4% for the femoral neck. The subjects had relatively low prevalence of osteoporosis. Since the total subjects had not experienced menopause or were in the early menopausal period, and the ages of the subjects ranged from 49 to 54 years. Among them, 507 subjects were premenopausal women.
However, the study for rural females reported high prevalence of osteopenia or osteoporosis (Kim et al., 2000). It is reported that 86.4% of the rural female subjects aged 50 years or above in their study had osteopenia or osteoporosis. The percentages of old women over aged 60 years in their study who had osteopenia or osteoporosis were 91.7%.
A study on the relationship between nutrition and bone mineral density showed that the bone mineral density of elderly people is related to their overall nutrition (Kim, 2001), and a study on menopausal women showed that almost all the nutrition intakes of these women have a positive correlation with their bone mineral density (Lee et al., 1992). Calcium intake, in particular, was found to have a significant effect on bone mineral density. The minimum calcium intake needed for minimizing the decrease of bone mineral density is estimated to be about 600 mg (Lee et al., 2005). According to the results of the Korea National Health and Nutrition Survey (Ministry of Health and Welfare, 2001), the average calcium intake of 65-year-olds or above in Korea in 2001 was 515.5 mg, which was far less than the EAR (estimated average requirement) of 580 mg and the RI (recommended intake) of 800 mg, and the actual absorption was estimated to be far less than the intake because the calcium intake was mainly through vegetables, which have a low calcium absorption rate (Korea Health Industry Development Institute, 2002). The environmental factors associated with poor skeleton metabolism include smoking (Jeng et al., 2000; Slemenda et al., 1992), alcohol, coffee, sodium, and the regularity of meals (Lee & Son, 2004), in addition to improper nutrition.
In this study, the nutrient intakes and dietary habits of elderly women in Daegu were investigated, and the data that were obtained were analyzed to determine if there is a relationship between such factors and these women's bone mineral density. This is expected that results can be used as the basic data to nutritional intervention for prevention of osteoporosis.
The survey was performed at a clinic center from May 2005 to August 2005 in Daegu. The subject of this research was 110 respondents of a survey carried out on the elderly women from 65 to 80-years-old who visited to check bone mineral density voluntarily. The analysis was conducted using verified 101 cases among the total samples.
The height (cm) and weight (kg) of the subjects were measured using a height and weight-measuring instrument (FANICS MEASURING SYSTEM, HM-170, 1999), and their BMI [body mass index = weight (kg) / height (m2)], which reflects the body fat more accurately than the standard weight does, was calculated from the height and weight values. The body fat rate (fat%) was also measured using an automatic fat-measuring instrument's, a body fat monitor HBF-302 (Hongil Medical, 2004).
The bone mineral densities of the subjects were measured using Lunar's dual-energy X-ray absorptiometry (DEXA), and the diagnoses were conducted according to WHO standards: the bone mineral density was classified as normal if the T-score (calculated by dividing the difference between the individual bone mineral density and the maximum bone mineral density of a young adult by the standard deviation of the normal bone mineral density) was above -1.0; osteopenia was adjudged to exist if the T-score was between -1.0 and -2.5; and osteoporosis was adjudged to exist if the T-score was -2.5 or below.
The survey carried out on trained researcher through individually interviews. Subjects were asked to provide information on maternal factors such as age, menarche, menopause, and children, and dietary habits such as the regularity of the eating time, the frequency of the intake of vegetables and fruits, and the frequency of the intake of dairy foods.
To determine the subjects' nutrient intake levels, they were interviewed individually using the 24-hour (one-day) recall method. Their daily energy and nutritional intakes were calculated by inputting the collected nutritional intake data into the professional-use CAN-pro (Computer-aided Nutrition Analysis, version 3.0) developed by Korea Nutrition Society, and were compared with the EAR (estimated average requirement), RI (recommended intake), and AI (adequate intake) values provided by KDRIs (Dietary Reference Intake for Koreans).
Statistical analysis was conducted using the SAS program. The frequency count, percentage, mean and standard deviation were calculated for all the variables, and when the results of ANOVA test were found to be significant, they were verified through Duncan's multiple-range test (α=0.05).
Based on the WHO standards, bone mineral density was classified in this study as normal, osteopenia and osteoporosis. The subjects of this study were the elderly women from 65 to 80-years-old in the city. The bone mineral density of the subjects is as follows. The group that was found to have normal bone mineral densities represented 25.7% of the subjects, the osteopenia group 39.6%, and the osteoporosis group 34.7% (Table 1).
Table 2 shows the results of the comparison of the anthropometric measurements according to bone mineral density. The average age of the normal group was 71.1, 72.3 for the osteopenia group and 73.6 for the osteoporosis group. The average heights of the normal group, the osteopenia group, and the osteoporosis group were 151.3 cm, 149.7 cm, and 149.7 cm, respectively, and their average weights were 56.2 kg, 55.0 kg, and 54.1 kg, respectively, with no significant difference among the groups. The average BMIs (body mass indexes) in the normal group, the osteopenia group, and the osteoporosis group were 24.5 kg/m2, 24.5 kg/m2, and 24.4 kg/m2, respectively, and the average body fat rates were 33.0%, 32.5%, and 33.3%, respectively, with no significant difference among the groups.
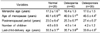
Table 3 shows the results of the comparison of the maternal factors according to bone mineral density. The average menarche ages of the normal group, the osteopenia group, and the osteoporosis group were 17.3, 16.4, and 17.0, respectively. There is no significant difference among the groups on average menarche ages. The average menopause ages of the normal group, the osteopenia group, and the osteoporosis group were 48.1, 46.9, and 45.5, respectively, and the normal group had a somewhat high value although this had no statistical significance. The postmenopausal periods were 23.0 years long for the normal group, 25.3 years long for the osteopenia group, and 27.4 years long for the osteoporosis group, which showed a significant difference between the normal group and the osteoporosis group (p<0.05) but no significant difference between the normal group and the osteopenia group. The average numbers of children were 4.6 for the normal group, 4.5 for the osteopenia group, and 4.2 for the osteoporosis group, with no significant difference among the groups. The last-child-delivery ages of the normal group, the osteopenia group, and the osteoporosis group were 33.27, 35.7, and 33.9, respectively, with no significant difference among the groups.
Based on the results of the comparison of the subjects' bone mineral density levels (Table 4), the rates of their regular diets were determined to be 53.9% for the normal group, 52.5% for the osteopenia group, and 54.1% for the osteoporosis group. The rates of their daily intake of 200 ml milk or above were 7.7% for the normal group, 5.0% for the osteopenia group, and 8.5% for the osteoporosis group; and the rates of the intake of 4-5 200 ml glasses of milk/week were 23.1% for the normal group, 10.0% for the osteopenia group, and 11.4% for the osteoporosis group. The rates of the non-intake of milk were 7.7% for the normal group, 25.0% for the osteopenia group, and 20.0% for the osteoporosis group, with no statistical significance. As for the intake of fruits and vegetables, one intake was recognized to be 70 g or more of fruits and 60-70 g or more of vegetables. The daily intakes (%) were 7.7% for the normal group and none for the osteopenia and osteoporosis groups. The percentage of the non-intake of fruits and vegetables were 7.7% for the normal group and 10.8% for the osteoporosis group.
The nutrient intakes (determined through the 24-hour recall method) according to the bone mineral density are shown in Table 5. The nutrient intakes of the subjects were 1505.0 kcal for the normal group, 1481.9 kcal for the osteopenia group, and 1484.3 kcal for the osteoporosis group, with no significant difference among them. There was no significant difference between the three groups' intakes of protein, lipid, carbohydrate, calcium, phosphorous, and potassium, and the vitamin A, B1, and B2 intakes were significantly higher in the normal group than in the osteopenia and osteoporosis groups. The intake of cholesterol was lower, though, in the normal group than in the osteopenia or osteoporosis group.
Table 6 shows the intakes of nutrients as rates against the recommended intake (RI) or the adequate intake (AI). All the groups had less calcium, vitamin B1, vitamin B6, and folate than the RI, and the intakes of fibrin and potassium were far lower than the AI, while the intake of sodium was very high.
The calcium intakes compared to the RI were 86.1% for the normal group, 79.4% for the osteopenia group, and 79.8% for the osteoporosis group, with all the groups recording less than the recommended intakes, having no significant difference due to the bone mineral density. The vitamin A intake levels against the RI were 141.2% for the normal group, 107.5% for the osteopenia group, and 111.7% for the osteoporosis group, with all the groups satisfying the RI. The vitamin A intake of the normal group was significantly higher, though, than those of the osteopenia group and of the osteoporosis group (p<0.05). The vitamin B1 intakes of the normal group, the osteopenia group, and the osteoporosis group were 1.0 mg, 0.9 mg, and 0.9 mg, respectively, which represented 92.2%, 78.6%, and 80.6% of the RI. As such, the vitamin B1 intakes of all the groups were lower than the RI. The normal group had a significantly higher vitamin B1 intake level, though, than the osteopenia group and the osteoporosis group (p<0.05). The vitamin B2 intakes of the normal group, the osteopenia group, and the osteoporosis group were 1.0 mg, 0.8 mg, and 0.9 mg, respectively, which were somewhat higher than the RI. The normal group had a significantly higher vitamin B1 intake level, though, than the osteopenia and osteoporosis groups (p<0.05). The folate intakes were 242.5 µg for the normal group, 243.7 µg for the osteopenia group, and 244.5 µg for the osteoporosis group, which represented 60.6%, 60.9%, and 61.1% of the RI, respectively, with no significant difference among the groups but showing a somewhat low intake level in all of them. All the groups had more than four times as much sodium (Na) as the AI, while the potassium (K) intakes were 56.5% for the normal group, 56.8% for the osteopenia group, and 56.4% for the osteoporosis group, all very low values. The cholesterol intakes of the normal group, the osteopenia group, and the osteoporosis group were 358.5 mg, 233.0 mg, and 311.1 mg, respectively, with a significant difference between the normal group and the osteopenia group.
Table 7 shows the rate of nutrient intake of the old women in Daegu against the EAR. The protein, Ca, P, Fe, zinc, vitamin A, vitamin B6, and niacin intakes of all the groups were more than 100% of the EAR. The vitamin A intakes of the osteopenia and osteoporosis groups were significantly low, however, in terms of%EAR (p<0.05). Energy was somewhat insufficient in all the groups compared to the EAR, and folate was low, within the range of 75.8-76.4% of the EAR. In the case of vitamin B1, the normal group had more than the EAR, but the osteopenia group had only 96.1% while the osteoporosis group had only 97.1%, which represented a significantly lower%EAR than that of the normal group. For vitamin B2, the normal group had 99.3%, while the osteopenia group had 83.6% and the osteoporosis group 87.2%, less than the EAR, representing a significantly lower%EAR compared to that of the normal group (p<0.05). Vitamin C intake showed no significant difference among the groups, but the intake of the osteopenia group was lower than the EAR.
In the study conducted by Kim et al. (2000), it was reported that 10% of the subjects who were 60 years old or above maintained a normal bone mineral density, and that 85.5% of the old male subjects and 91.7% of the old female subjects had osteopenia or osteoporosis. Contrary to the results of the previous study, 74.3% of the old female subjects in this study were found to have osteopenia or osteoporosis, with the average age of the subjects being 72, showing a relatively low osteoporosis rate.
The subjects of this study were female in the ages from 65 to 80 years old. By comparing the average age according to the bone mineral density by group, it was not found the influence of age on osteoporosis. There was no significant difference, though, in the other factors (height, weight, BMI, and body fat) according to bone mineral density.
According to the Korea National Health and Nutrition Survey (Ministry of Health and Welfare, 2001), the average menarche age was 16.7 years, and the average menopause age was 48 years, for women who were 65 years old or above. The menarche age then was similar to that established in the previous study, but the total average of the menopause age was 47 years, which was 1 year less than the national average. In particular, the osteoporosis group had a younger menarche age than the normal group, and its menopause age was 2.6 years less than that of the normal group, but the osteoporosis group had a 5.1-year-longer menopause period than the normal group did, which implies that menopause age or menopause period influences the health of a person's skeleton.
In this study on the dietary habits of elderly women according to the classification of their bone mineral density, no difference was found among the groups in terms of eating regularity. However, in terms of the frequency of their intake of dairy products, the people who 'never' intake had 3.2 times of osteopenia and 2.6 times of osteoporosis than those of normal group. In terms of the intake of vegetables and fruits, both osteopenia and osteoporosis group did not have 'everyday' intake people. However, the osteopenia group had 11.4% of 'never' answer. Since the sample size of this study is not enough to have a significant result, the sample size should be increased in the next study.
The previous study reported the relationship of frequency of vegetables and fruits (Bae & Sung, 2005). In addition, it also coincided with the report by Celia et al. (2006), that there was a significant positive relationship between the intake of vegetables and fruits and the bone mineral densities of the spine and femur, and with the report by Susan et al. (2000), that the bone mineral densities of those who have a high intake of vegetables and fruits were high. According to Tucker et al. (1999), vegetables and fruits help keep the bone mineral density at its normal level because they include many alimentary ingredients that produce alkaline metabolite in a body, and R. Jajoo et al. (2006) reported that alkaline metabolite decreases the total acid drainage rate in the body, thereby lowering the PTH in the blood, the bone absorption, and the calcium drainage.
In addition, Franceschi (1992) reported that vitamin C in vegetables and fruits act as coenzymes for the hydroxylation of lysine and proline, which synthesize the collagen protein composing the skeleton (Franceschi, 1992). According to Katherine et al. (2002), magnesium, potassium, vitamin C, and vitamin K, which are abundant in vegetables and fruits, have an effect on the bones. In a study on rural women in Japan who have not had menopause, the BMD was found to be higher in those who had a high intake of fish, vegetables, and fruits and a low intake of meat and processed foods (Kazutoshi et al., 2005) than in those who had the opposite.
There was no significant difference among the groups in this study in terms of their calcium intake, according to the comparison of the nutrient intakes by bone mineral density. The calcium intakes were 688.6 mg for the normal group, 635.4 mg for the osteopenia group, and 638.7 mg for the osteoporosis group, which were somewhat higher than the EAR of Korea in 2005, but all the groups had less than the 800 mg RI (normal group: 86.1%; osteopenia group: 79.4%; osteoporosis group: 79.8%). Therefore, all the older-women groups had insufficient calcium. This suggests that the calcium intake of senile women, who have a high osteoporosis onset risk, should be increased, and that nutrition education programs with the aim of increasing the calcium intake to prevent the onset of osteoporosis should be offered, especially to the elderly.
It was recently reported that calcium helps keep a person's bone mineral density at the normal level and influences bone metabolism by helping drain the total acid in the body (Sebastian et al., 1994). Both the normal group and the osteoporosis group in this study had far less potassium than the AI presented in the nutritional standards of Korea in 2005 (4700 mg/day): the normal group had 56.4%, and the osteoporosis group 56.9%. Meanwhile, their sodium intakes were 423% and 406% of the AI, respectively, which were very high. If a high-sodium diet is considered disadvantageous to bone mineral density (Goulding & Campbell, 1983), education on increased potassium intake is necessary to improve the drainage of sodium. Since the risk of hypertension increases as a person becomes older, sufficient potassium intake is important. The dietary fiber AI for old people in the country's nutritional standards is 22 g/d, but the intakes of the subjects in this study were 6.3 g for the normal group, 6.4±2.2 g for the osteopenia group, and 6.4±1.8 g for the osteoporosis group, which were very insufficient (normal group: 30.9% of the AI; osteopenia group: 29.3%; and osteoporosis group: 28.8%).
The vitamin A intake of the normal group was higher than those of the osteopenia and osteoporosis groups. All the groups had insufficient vitamin B2 and folate intakes, which must be addressed through related education.
In summary, the osteoporosis group had a higher average age, a lower menopause age, and a longer postmenopausal period than the normal group, with a significant difference. The osteopenia and osteoporosis groups had lower intake percentage of milk, vegetables and fruits than the normal group. And, the vitamin A, B1, and B2 intakes were significantly higher in the normal group than in the osteopenia and osteoporosis groups. Furthermore, all the groups had less calcium, vitamin B1, vitamin B6, and folic acid than the RI; their fiber and potassium intakes were far lower than the AI; and their sodium intake was very high.
In conclusion, nutritional education is necessary to encourage the high intake of milk and vegetables and fruits along with calcium, vitamin A, B1, and B2 intakes and the low intake of sodium for the prevention of osteoporosis in elderly women's osteoporosis.
Figures and Tables
Table 3
Menarche, menopausal state, and maternal factors according to the bone mineral density of the subjects
References
1. Bae YJ, Sung CJ. A Comparison between postmenopausal osteoporotic women and normal women of their nutrient intakes and the evaluation of diet quality. Korean Journal Community Nutrition. 2005. 10:205–215.
2. Franceschi RT. The role of ascorbic acid in mesenchymal differentiation. Nutr Rev. 1992. 50:65–70.

3. Gordon W. The effects of diet and Life style on bone mass in women. J Am Diet Assoc. 1988. 88:17–25.
4. Goulding A, Campbell D. Dietary Nacl loads promote calciuria and done loss in adult oophorectomized rats consuming a low calcium diet. J Nutr. 1983. 113:1409–1414.

5. Ho SC, Chan SG, Yi Q, Wong E, Leung PC. Soy intake and the maintenance of peak bone mass in Hong Kong Chinese women. J Bone Miner Res. 2001. 16:1363–1369.

6. Iki M, Kagamimori S, Kagawa Y, Matsuzaki T, Yoneshima H, Marumo F. Bone mineral density of the spine, hip and distal forearm in representative samples of Japanese female population: Japanese Population-Based Osteoporosis (JPOS) study. Osteoporos Int. 2001. 12:529–537.

7. Jajoo R, Song L, Rasmussen H, Harris SS, Dawson-Hughes B. Dietary acid-base balance, bone resorption, and calcium excretion. J Am Coll Nutr. 2006. 25:224–230.

8. Jeng SY, Han SY, Kim GM, Lee SY, Kim YJ. The relationship between nutrient intakes and bone mineral density by use of a semiquantitative food-frequency questionnaire. Journal of the Korean Academy of Family Medicine. 2000. 21:523–532.
9. Kang HS. Diagnosis of Osteoporosis. 1998. Seoul. Republic of Korea: Seoul National University Publishing Commit;24–32.
10. Kim KR, Kim KH, Lee EK, Lee SS. A study on the factors affecting bone mineral density in adult women-based on the mothers of elementary school students. Korean Journal of Nutrition. 2000. 33:241–249.
11. Kim SJ. Study on the osteoporosis in Korean middle-aged and elderly women in rural area. 2002. Ewha Womans University;Master's theses.
12. Kim YL, Park JH, Lee JS, Kim JY, Yang SO, Jun DJ, Kim MC, Jung DH, Lee YG, Lee BD. Prevalence and risk factors of the osteoporosis of perimenopausal women in the community population. The Korean Journal of Medicine. 2002. 62:11–24.
13. Koh SK, Cho SH, Hwang YY, Moon H, Kim DS, Cho JL. Spinal bone mineral density of normal and osteoporotic women in Korea. Journal of Korean Medical Science. 1992. 7:136–140.

14. Korea Health Industry Development Institute. Report on 2001 National Health and Nutrition Survey -Nutrition Survey(1). 2001. Seoul. Republic of Korea:
15. Lauderdale DS, Jacobsen SJ, Furner SE, Levy PS, Brody JA, Goldberg J. Hip fracture incidence among elderly Asia-American populations. Am J Epidemiol. 1997. 146:502–509.
16. Lee BK, Chang YK, Choi KS. Effect of nutrient intake on bone mineral density in postmenopausal women. Korean Journal Nutrition. 1992. 25:642–655.
17. Lee EJ, Son SM. Dietary risk factors related to bone mineral density in the postmenopausal women with low bone mineral density. Korean Journal of Community Nutrition. 2004. 9:644–653.
18. Lee YS, Park HM, Bae DH. Prevalence of Osteoporosis in Korean Women. Journal of the Korean Society of Menopause. 2002. 62:78–85.
19. Lee YS, Leem HS, Aha HS, Jang NS. Nutrition throughout the life cycle. 2005. Seoul. Republic of Korea: Kyomunsa Co.;262–263.
20. Ministry of Health and Welfare. Chapter 2 Health status: Daily nutrient supply per capita. The Yearbook on Health and Welfare Statistics. 2001. (The publication of the 49rd issue):Seoul. Republic of Korea: 66–67.
21. Ministry of Health and Welfare. Chapter 1 Population. The Yearbook on Health and Welfare Statistics. 2005. (The publication of the 53rd issue):Seoul. Republic of Korea: 41–47.
22. Nakamura K, Ueno K, Nishiwaki T, Okuda Y, Saito T, Tsuchiya Y, Yamamoto M. Nutrition, mild hyperparathyroidism, and bone mineral density in young Japanese women. Am J Clin Nutr. 2005. 82:1127–1133.

23. New SA, Robins SP, Campbell MK, Martin JC, Garton MJ, Bolton-Smith C, Grubb DA, Lee SJ, Reid DM. Dietary influences on bone mass and bone metabolism: further evidence of a positive link between fruit and vegetable consumption and bone health? Am J Clin Nutr. 2000. 71:142–145.

24. NOF. America's Bone Health: The state of osteoporosis and low bone mass. 2002. Washington DC. USA: National osteoporosis foundation.
25. Preisinger E, Leitner G, Uher E, Alacamlioglu Y, Seidl G, Marktl W, Resch KL. Nutrition and osteoporosis: a nutritional analysis of women in postmenopause. Wien Klin Wochenschr. 1995. 107:418–422.
26. Prynne CJ, Mishra GD, O'Connell MA, Muniz G, Laskey MA, Yan L, Prentice A, Ginty F. Fruit and vegetable intakes and bone mineral status: a cross-sectional study in 5 age and sex cohorts. Am J Clin Nutr. 2006. 83:1420–1428.

27. Sebastian A, Harris ST, Ottaway JH, Todd KM, Morris RC. Improved mineral balance and skeletal metabolism in postmenopausal women treated with potassium bicarbonate. N Engl J Med. 1994. 330:1776–1781.

28. Slemenda CW, Christian JC, Reed T, Reister TK, Williams CJ, Johnston CC Jr. Long-term bone loss in men: effects of genetic and environmental factors. Ann Intern Med. 1992. 117:286–291.

29. Tenenhouse A, Joseph L, Kreiger N, Poliguin S, Murray TM, Biondeau L. Estimation of the prevalence of low bone density in Canadian women and men using population-specific DXA reference standard; the Canadian Multicentre Osteoporosis study. Osteoporos Int. 2000. 11:897–904.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download