Abstract
This study assessed folate intakes, folate concentrations in plasma and erythrocytes, plasma total homocysteine (tHcy) concentration, and urinary excretion of folate metabolites in Korean women with childbearing potential. A total of 23 women voluntarily participated in this study. Precise dietary intakes for 3 consecutive days were determined by weighing all foods consumed and folate intake was calculated using a computer-aided dietary analysis system. Folate concentration of plasma and erythrocytes was determined by a microbiological method. Plasma tHcy concentration was assayed using an HPLC analysis method. Urine excreted over the same period of time was collected and folate catabolites, para-aminobenzoylglutamate (pABG) and para-acetamidobenzoylglutamate (ApABG), were evaluated using a reverse-phase HPLC method after affinity chromatography. Young women of 20 and under were likely to consume less folate with low energy intake, had lower folate concentration in plasma and erythrocytes, and excreted a lesser amount of ApABG and total folate catabolites than women of 25 years and over. The results of this study confirmed that young Korean women with childbearing potential, especially those under 21 years of age, might be at risk for compromised folate status due to insufficient folate intakes from inadequate energy consumption.
Maternal folate deficiency may cause congenital malformations (Bonin et al., 1998; Moyers & Bailey, 2001), including neural tube defects (NTDs) (Scholl & Johnson, 2000), and adverse outcomes of pregnancy such as low birth weight (Vollset et al., 2000). The fact that neural tubes close during the fourth week of gestation (McNulty et al., 2000) implies that folate nutritional status at peri-conception is essential to prevent NTDs. However, an estimated 50% of pregnancies in the United Kingdom (Department of Health, 1992) and the United States (Grimes, 1986) are unplanned as are over 40% in developing countries (Chinebuah & Perez-Escamilla, 2001). It is, therefore, important to ensure adequate folate status in all women of reproductive age.
Previous studies on the folate status of Korean women with childbearing potential have indicated that dietary intakes of folate are insufficient to maintain adequate folate status (Ahn et al., 2002; Hyun & Han, 2001; Hyun et al., 1999; Kim et al., 1999; Lim et al., 2000), and a considerable proportion of women are marginally folate deficient (Ahn et al., 2002; Hyun et al., 1999; Lim et al., 2000). However, those studies determined only folate intakes (Hyun & Han, 2001; Kim et al., 1999), folate concentrations of serum or erythrocytes (Hyun et al., 1999; Lim et al., 2000), and/or plasma total homocysteine (tHcy) concentration (Ahn et al., 2002).
Serum folate concentration is used as a sensitive indicator of recent folate balance, erythrocyte folate concentration is considered an index of a prolonged folate status (Herbert, 1990), and the elevation of plasma tHcy concentration is agreed to be a metabolic result of folate deficiency (Bakker & Brandjes, 1997). Those are the common indexes for evaluation of folate nutritional status. In addition, urinary folate catabolite excretion is considered another long-term indicator of the body folate pool size that parallels the functional measures of folate status (Wolfe et al., 2003). It responds to the changes in dietary folate intakes slowly within the controlled research conditions of a metabolic protocol (Caudill et al., 1998; Gregory et al., 2000). Folate catabolism represents the major route of folate turnover in humans under conditions of normal folate intake and involves cleavage of the C9-N10 bond producing a pterin and paraaminobenzoylglutamate (pABG) (Geoghegan et al., 1995). The majority of pABG is N-acetylated in the cytosol by arylamine N-acetyltransferase to produce para-acetamidobenzoylgultamate (ApABG) (Estrada-Rogers et al., 1998; Minchin, 1995). Previous studies performed in western countries reported that mean urinary ApABG and pABG concentrations of nonpregnant women were ~110 and 27 nmol/d (Caudill et al., 1998) and ~104 and 49 nmol/d (McPartlin et al., 1993), respectively and ~150 nmol/d (pABG plus ApABG) (Kownacki-Brown et al., 1993).
However, there is little data available on urinary folate catabolite excretion of reproductive-aged women in Korea. We previously confirmed that folate intake was related to energy consumption and found that energy intake was associated with age in women of childbearing potential (Lim et al., 2000): The young women, aged 15 to 24 years, consumed less energy and folate with lower folate-density meals than older women over 25 years of age. However, folate status of the young women, as estimated by the folate concentrations of plasma and erythrocytes, was not significantly different from that of the older women, contrary to our assumption.
Therefore, this study was designed to evaluate the folate status of women with childbearing potential according to age, by determining plasma concentrations of folate and tHcy as short-term indexes and erythrocyte folate concentration and urinary excretion of folate catabolites as long-term indexes.
Subjects for this study were recruited from women aged 15 to 45 years living in Gwangju, a large city, and Sunchon, a small city, in Korea. Smokers and users of oral contraceptive agents were excluded. A total of twenty-three healthy women participated voluntarily in this study. The purposes and procedures of the study were explained to each subject and all subjects provided written informed consent.
Daily dietary intakes were determined for 3 consecutive days by a weighed food record method: The subjects were instructed how to weigh and record their meals using the dietary scale (± 1 g) distributed to them. Intakes of energy and folate were calculated using a computer-aided dietary analysis system (CAN-Pro version 2.0, The Korean Nutrition Society).
Venous blood samples from the fasting subjects were collected once on the day after the 3-day dietary survey. The blood samples were used for a variety of laboratory measurements. Hemoglobin concentration and hematocrit values were determined by a hematology analyzer (Coulter STKS; Beckman Coulter, Fullerton, CA). Folate concentrations of plasma and erythrocytes were determined by a microbiological assay (Tamura, 1990) using Lactobacillus casei (ATCC 7469; ATCC, Manassas, VA) with a microplate reader (ELX 808; Bio-Tec Instruments Inc, Winooski, VT). Plasma tHcy concentration was measured by HPLC (model 501; Waters Corporation, Milford, MA) using the method of Araki and Sako (1987).
Daily 24-h urine was collected in a PET bottle containing 3 g of sodium ascorbate during the same 3 consecutive days as the dietary survey. Subjects were instructed to keep the urine refrigerated at all times during the collection period to protect against bacterial growth. After total urine volume was recorded, the urine was mixed thoroughly, dispensed into 300 ml portions, and stored in a frozen state at -20℃.
Urinary folate catabolite concentrations, pABG and ApABG, were determined by a reverse-phase HPLC analysis method (McPartlin et al., 1992) after affinity chromatography (Selhub et al., 1980). Urine samples were adjusted to pH 7.0 and filtered through Whatman number 1 filter paper. Filtered urine samples were applied to 2 ml FBP-Affigel columns containing immobilized folate-binding protein to remove intact folate. After affinity chromatography, the 20 ml urine samples were adjusted to a final concentration of 0.1 mol/l HCl and applied to glass columns (200 × 15 mm) filled to a height of 5 cm with a slurry of Dowex 50W (50 × 8 - 400, Sigma Chemical, St Louis, MO) cation exchange resin equilibrated with 0.1 mol/l HCl. Acetamidobenzoylglutamate was eluted in the sample volume and the following 50 ml 0.1 mol/l HCl effluent, which were pooled and retained. A second 50 ml 0.1 mol/l HCl was applied to wash the column and 100 ml 0.6 mol/l HCl was applied to collect the pABG fraction. The fraction containing ApABG was acidified to 0.2 mol/l HCl and heated at 100℃ for 60 min to deacetylate it. After deacetylation, the fraction was adjusted to 0.1 mol/l HCl and reapplied to the re-equilibrated ion exchange columns. After a 100 ml wash with 0.1 mol/l HCl, pABG representing the ApABG fraction was eluted and collected in 100 ml 0.6 mol/l HCl. The two pABG fractions were kept separate throughout the process and derivatized. One milliliter of sodium nitrite solution (1%) and 1 ml 5.0 mol/l HCl was added to each pABG fraction and reacted at room temperature. After 5 min, 1 ml ammonium sulfamate solution (50 g/l) was added. Then, after 5 min, 1 ml N-(1-naphthyl)-ethylenediamine solution (10 g/l) was added to couple pABG.. Both fractions sat overnight at room temperature to complete formation of the purple-colored azo-N-(1-naphthyl)-ethylenediamine derivative of pABG (azo-pABG). Each fraction was applied to a preactivated (5 ml methanol wash followed by 5 ml H2O) C18 Sep Pak cartridge (Waters, Milford, MA). After a 10 ml 0.05 mol/l HCl wash, azo-pABG was eluted in 4 ml 100% methanol. The solution was evaporated until dry at 40℃ under a stream of nitrogen. The residue was reconstituted in 250 µl H2O and added to a 25 µl 5 mol/l HCl and 25 µl zinc powder suspension (1 g/3 ml H2O). After 15 min mixing, the mixture was transferred to a 1-ml Eppendorf tube and centrifuged for 10 min. The supernatant from the centrifuged mixture was removed, filtered, and stored at -20℃ until HPLC analysis. The amount of pABG was determined by reverse-phase HPLC with an octadecylsilica column (Ultramex C18, 5-µm particle size, 4.6 mm ID × 250 mm; Phenomenex, Torrance, CA). The HPLC injection volume was 100 µl, and flow rate was 1.0 ml/min. The isocratic mobile phase (pH 4.0) was composed of acetonitrile (2%) and 0.1 mol formic acid (98%). A UV absorption detector (Diones AD 20) monitored at 280 nm. Quantification of pABG (representing excreted pABG and ApABG) was estimated from a standard curve derived using commercial pABG (Sigma Chemical, St Louis, MO).
All statistical analyses were performed with the use of SPSS version 10.0 (SPSS Inc, Chicago, IL). The subjects were divided into two groups; Lower (20 y and under, n = 13) or Upper (25 y and over, n = 10) groups. Data were presented as means ± SDs for 10 to 13 subjects. Mean differences between the two groups were compared with t-test. Regression equations were derived to explain the associations between age and folate status indexes. Pearson's correlation coefficients were used to describe the relationships among the folate status indexes. A p-value<0.05 was considered significant. Since the data of weight, folate intake, dietary folate density, plasma tHcy concentration, folate concentrations of plasma and erythrocytes, and urinary excretion of pABG and ApABG did not show standard distribution, those were transposed into natural log before statistical analysis.
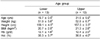
Age, anthropometrical measurements, and hematological indexes of the subjects are shown in Table 1. The average ages of Lower and Upper groups were 20.9 ± 0.5 and 31.5 ± 5.9 y. No significant differences were detected in weight, height, and BMI between the two groups and hemoglobin and hematocrit values were not significantly different either.
Dietary intakes of energy and folate of the subjects are presented in Fig. 1. Energy intake of Lower group was significantly lower than that of Upper group (1457 ± 421 vs 1977 ± 527 kcal, p<0.05). Lower group consumed significantly less folate than Upper group (158.8 ± 47.7 vs 280.9 ± 121.0 µg DFE, p<0.05). However, dietary folate density was not significantly different between the two groups (113.5 ± 35.0 vs 141.4 ± 34.3 µg DFE /1000 kcal, p<0.05).
Plasma and erythrocyte folate concentrations and plasma tHcy concentration of the subjects are shown in Fig. 2. Plasma folate concentration of Lower group (ng/ml) was significantly lower than that of Upper group (9.1 ± 2.2 vs 12.7 ± 5.1 ng/ml, p<0.05). Erythrocyte folate concentration of Lower group was also significantly lesser compared to that of Upper group (178.9 ± 72.0 vs 289.7 ± 99.0 ng/ml, p<0.01). However, no significant difference in plasma tHcy concentrations was found between the two groups (13.1 ± 4.6 vs 11.7 ± 3.5 ng/ml).
The measurement of urinary folate catabolites yielded the results shown in Fig. 3. Although the excretion of pABG (9.5 ± 2.1 vs 11.4 ± 3.2 nmol/d) was not different between the two groups, Lower group excreted significantly less ApABG (81.3 ± 23.7 vs 100.6 ± 16.6 nmol/d, p<0.05) and total folate catabolites (90.8 ± 24.0 vs 112.0 ± 16.7 nmol/d, p<0.05) than Upper group, respectively. The ratio of ApABG/total folate catabolites of all subjects was 0.89 ± 0.03 and the molar ratio of total folate catabolites/ folate intake was 0.24 ± 0.08. No significant differences were observed in those two ratios between the two groups.
As presented in Fig. 4, positive linear relationships were observed between age and dietary folate intake (r = 0.4293, p<0.05), erythrocyte folate concentration (r = 0.6160, p<0.01), urinary excretion of ApABG (r = 0.4185, p<0.05), and total folate catabolites (r = 0.4465, p<0.05).
As indicated in Table 2, dietary folate intakes correlated positively with plasma folate concentration (r = 0.5078, p<0.05) but not with erythrocyte folate concentration. In addition, erythrocyte folate concentration related positively to urinary excretion of ApABG (r = 0.6278, p<0.01) and total folate catabolites (r = 0.6171, p<0.01). There was a considerable relationship between urinary excretion of ApABG and total folate catabolites (r = 0.9933, p<0.001). Although it was not significant, folate intakes related positively to urinary excretion of total folate catabolites (r = 0.3840, p<0.07).
The present study showed that among Korean women of childbearing potential, young women of 20 y and under (Lower group) consumed less folate due to insufficient energy consumption than the women of 25 y and over (Upper group). This result was consistent with a previous report (Lim et al., 2000) revealing that younger women in Korea consumed less folate than older women, although the mean ages of the groups were not exactly same in the two studies.
The women of Lower group who consumed less folate showed, consequently, inadequate folate status; they had significantly lower folate concentration in both plasma and erythrocytes compared to the women of Upper group. These results indicate that dietary folate intakes of the women in Lower group are insufficient to maintain adequate folate concentration in both plasma and erythrocytes. In this study, contrary to an expectation, plasma tHcy concentration, a valid functional index of long-term folate status (Jacob et al., 1994; O'keefe et al., 1995), was not significantly different between the two groups. Plasma tHcy concentration had an inverse relationship to erythrocyte folate concentration but not significant (r = -0.3843, p<0.07). As estimated by plasma folate concentration, no women in this study were found to be folate-deficient (<3 ng/ml) but one subject (10.0%) in Upper group was in marginal folate-deficiency (3-5.9 ng/ml). As determined by erythrocyte folate concentration, however, 5 subjects (38.5%) in Lower group were in folatedeficient (<140 ng/ml) and 1 subject (10.0%) in Upper group was in marginally folate-deficient (14 ~ 156 ng/ml). The result that more than one third of the women in Lower group were in marginally folate-deficient confirms that their folate intakes were not enough for a long time but it was not short to raise plasma tHcy concentration. Several studies performed in Korea have already reported that a considerable proportion of women of childbearing age were marginally folate-deficient (Ahn et al., 2002; Hyun et al., 1999; Lim et al., 2000).
The urinary folate catabolite excretion in this study revealed that the women of Lower group who consumed less dietary folate and were in inadequate folate status excreted less ApABG and total folate catabolites than the women of Upper group. Wolfe et al. (2003) recently reported that folate catabolite excretion was significantly reduced in response to a low-folate diet, which may reflect a decrease in tissue folate catabolism or in the rate of folate turnover. Based on this evidence, it is reasonable to assume that the women of Lower group had a smaller tissue folate pool with lower rate of folate turnover than the women of Upper group. In the present study, ApABG and total folate catabolite urinary excretion were positively associated with dietary folate intakes but not significant. However, ApABG and total folate catabolite urinary excretion were positively and significantly associated with erythrocyte folate concentration. This result suggests that urinary excretion of folate catabolites might be an indicator of folate turnover. Erythrocyte folate concentration is considered to be the primary indicator of adequacy of folate status because of its correlation with liver folate and thus tissue stores (Tu et al., 1975). Urinary ApABG excretion, the primary excretory form and an index of long-term folate status, may be influenced by tissue folate concentration. In this study, ApABG constituted >85% of total folate catabolites as also reported by Gregory et al. (2000). The result in this study that plasma folate concentration was positively correlated with folate intakes confirmed that plasma folate concentration is a sensitive index of recent folate status (Herbert, 1987). As found in the above results, total folate catabolite excretion strongly related to erythrocyte folate concentration. Thus, these data do not sustain the idea that urinary excretion of folate catabolites is an unreliable index of folate status (Sauberlich et al., 1987).
In a study of young American adults (Wolfe et al., 2003), the subjects excreted 115.0 ± 12.7 nmol/d of total folate catabolites when they were consuming their usual diets but 86.1 ± 26.7 nmol/d when they consumed folate-depleted diets. The excretion of total folate catabolites of Upper group was similar to the data of the Americans consuming usual diets and that of Lower group was comparable to the data of the Americans consuming folatedeficient diets.
Based on the overall results of this study, it could be assumed that young women of 20 y and under consumed insufficient folate to maintain adequate folate status. Therefore, young women under 21 y should obtain more folate by increasing energy intakes and/or taking folate supplements. Brouwer et al. (1999) reported that a dose as low as 250 µg folic acid/d in addition to usual dietary folate intakes effectively lowered plasma tHcy concentration and increased the folate status of young, healthy women. According to the report of Sauberlich et al. (1987), when subjects consumed less than 150 µg/d of folate from food, plasma and erythrocyte folate concentration declined; however, plasma folate concentration appeared to stabilize with an intake of 200 µg/d of folate, but erythrocyte folate concentrations continued to fall. In this study, the amount of folate consumed by the women of Upper group, 289.7 ± 99.0 µg/d, might be sufficient to maintain adequate folate status for women of childbearing age.
The results of this study demonstrating that age related positively to dietary folate intakes, erythrocyte folate concentration, urinary excretion of ApABG and total folate catabolite suggest that age may be an important factor influencing the folate status of women with childbearing potential. This might be a result of poor dietary habits (Lim et al., 2002) of young women; among the Korean women with childbearing potential, 27% of the teens and 45% of those in their twenties were underweight (BMI < 20) and their dietary intakes of energy, folate, iron, and calcium did not meet the Korean RDA.
In conclusion, the results from the present study suggest that young age under 21 may be an important factor influencing folate status in Korean women of childbearing age, and also support the idea that inadequate folate intake is associated with compromised folate status and lowered urinary excretion of folate catabolites. It should be recommended that women with childbearing potential, especially young women under 21 y, increase energy intake and consume meals rich in folate.
Figures and Tables
 | Fig. 1Dietary intakes of energy and folate and folate density of the diets of the subjects by age.
Values with different lower case letters are significantly different at p<0.05 by t-test.
|
 | Fig. 2Plasma and erythrocyte folate and plasma total homocysteine (tHcy) concentrations of the subjects by age.
Values with different lower case letters are significantly different at p<0.05 and those with different upper case letters at p<0.01 by t-test.
|
 | Fig. 3Urinary excretion of folate catabolites, para-aminobenzoylglutamite (pABG) and para-acetamidobenzoylglutamite (ApABG,) of the subjects by age.
Values with different lower case letters are significantly different at p<0.05 by t-test.
|
 | Fig. 4Regression equations between age and folate intake, erythrocyte folate concentration, urinary excretion of para-acetamidobenzoylglutamite (ApABG), and the sum of para-aminobenzoylglutamite (pABG) plus ApABG. |
References
1. Ahn HS, Jeong EY, Kim SY. Studies on plasma homocysteine concentration and nutritional status of vitamin B6, B12 and folate in college women. Korean Journal of Nutrition. 2002. 35:37–44.
2. Araki A, Sako Y. Determination of free and total homocysteine in human plasma by HPLC with fluorescence detection. J Chromatogr. 1987. 422:43–52.

3. Bakker RC, Brandjes DPM. Hyperhomocysteinemia and associated disease. Pharm World Sci. 1997. 19:126–132.
4. Bonin MM, Bretzlaff JA, Therrien SA, Rowe BH. Knowledge of periconceptional folic acid for the prevention of neural tube defects; the missing links. Arch Fam Med. 1998. 7:438–442.

5. Brouwer IA, van Dusseldorp M, Thomas CMG, Duran M, Hautvast JGAJ, Eskes TKAB, Steegers-Theunissen RPM. Low-dose folic acid supplementation decreases plasma homocysteine concentrations: a randomized trial. Am J Clin Nutr. 1999. 69:99–104.

6. Caudill MA, Gregory JF III, Huston AD, Bailey LB. Folate catabolism in pregnant and nonpregnant women with controlled folate intakes. J Nutr. 1998. 128:204–208.

7. Chinebuah B, Perez-Escamilla RP. Unplanned pregnancies are associated with less likelihood of prolonged breast-feeding among primiparous women in Ghana. J Nutr. 2001. 131:1247–1249.

8. Folic acid and the prevention of neural tube defects. Department of Health Report from an Expert Advisory Group. 1992. London. UK: Department of Health.
9. Estrada-Rodgers L, Levy GN, Weber WW. Substrate selectivity of mouse N-acetyltransferase 1, 2, and 3 expressed in COS-1 cells. Drug Metab Dispos. 1998. 26:502–505.
10. Geoghegan FL, McPartlin JM, Weir DG, Scott JM. Paraacetamidobenzoylglutamate is a suitable indicator of folate catabolism in rats. J Nutr. 1995. 125:2563–2570.
11. Gregory JF, Swendseid ME, Jacob RA. Urinary excretion of folate catabolites responds to changes in folate intake more slowly than plasma folate and homocysteine concentrations and lymphocyte DNA methylation in postmenopausal women. J Nutr. 2000. 130:2949–2952.

12. Grimes DA. Unplanned pregnancies in the US. Obstet Gynecol. 1986. 67:438–442.
13. Herbert V. Making sense of laboratory tests of folate status: folate requirements to sustain normality. Am J Hematol. 1987. 26:199–207.

14. Herbert V. Picciano MF, Stokstad ELR, Gregory JP, editors. Development of human folate deficiency. Evaluation of Folic Acid Metabolism in Nutrition and Disease. 1990. New York. USA: Alan R. Liss;195–210.
15. Hyun TS, Han YH. Comparison of folate intake and food sources in college students using the 6th vs. 7th nutrient database. Korean Journal of Nutrition. 2001. 34:797–808.
16. Hyun TS, Han YH, Lim EY. Blood folate level determined by a microplate reader and folate intake measured by a weighed food record. Korean Journal of Community Nutrition. 1999. 4:512–520.
17. Jacob RA, Wu MM, Henning SM, Swenseid ME. Homocysteine increases as folate decreases in plasma of healthy men during short-term dietary folate and methyl group restriction. J Nutr. 1994. 124:1072–1080.

18. Kim Y, Kim K, Chang N. Dietary folate intake of Korean women of childbearing age. Korean Journal of Nutrition. 1999. 32:585–591.
19. Kownacki-Brown PA, Wang C, Bailey LB, Toth JP, Gregory JF III. Urinary excretion of deuterium-labeled folate and the metabolite p-aminobenzoylglutamate in humans. J Nutr. 1993. 123:1101–1108.
20. Lim HS, Jin HO, Lee JA. Dietary intakes and status of folate in Korean women of childbearing potential. Korean Journal of Nutrition. 2000. 33:296–303.
21. Lim HS, Kang SA, Lee JI, Jin HO. Low intakes of energy, folate, iron, and calcium of childbearing Korean women. Ecol Food Nutr. 2002. 41:401–403.

22. McNulty H, Cuskelly GS, Ward M. Response of red blood cell folate to intervention; implications for folate recommendations for the prevention of neural tube defects. Am J Clin Nutr. 2000. 71:1308S–1311S.

23. McPartlin J, Halligan A, Scott JM, Darling M, Weir DG. Accelerated folate breakdown in pregnancy. Lancet. 1993. 341:148–149.

24. McPartlin JM, Courtney G, McNulty H, Weir DG, Scott JM. The quantitative analysis of endogenous folate catabolites in human urine. Anal Biochem. 1992. 206:256–261.

25. Minchin RF. Acetylation of p-aminobenzoylglutamate, a folic acid catabolite, by recombinant human arylamine N-acetyltransferase and U937 cells. Biochem J. 1995. 307:1–3.

26. Moyers S, Bailey LB. Fetal malformations and folate metabolism; review of recent evidence. Nutr Rev. 2001. 59:215–235.

27. O'Keefe CA, Bailey LB, Thomas EA, Hofler SA, Davis BA, Cerda JJ, Gregory JF. Controlled dietary folate affects folate status in nonpregnant women. J Nutr. 1995. 125:2717–2725.
28. Sauberlich HE, Kretsch MJ, Skala JH, Johnson HL, Taylor PC. Folate requirement and metabolism in nonpregnant women. Am J Clin Nutr. 1987. 46:1016–1028.

29. Scholl TO, Johnson WG. Folic acid; influence on the outcome of pregnancy. Am J Clin Nutr. 2000. 71:1295S–1303S.

30. Selhub J, Ahmad O, Rosenberg IH. Preparation and use of affinity columns with bovine milk-folate binding protein covalently linked to Sepaharose 4B. Methods Enzymol. 1980. 66:686–690.
31. Tamura T. Picciano MF, Stokstad ELR, Gregory JF, editors. Microbiological assay of folates. Folic Acid Metabolism in Health and Disease. 1990. New York. USA: John Wiley & Sons;121–137.
32. Tu A, Chanarin I, Slavin G, Levi AJ. Folate deficiency in the alcoholic; its relationship to clinical and hematological abnormalities, liver disease, and folate stores. Br J Haematol. 1975. 29:269–278.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download