Abstract
Mixed squamous cell and glandular papilloma is a rare pulmonary neoplasm typically occurring in the central lung area. Herein, we report a case of peripherally located mixed papilloma in a 54-year-old man with a complaint of dyspnea. Chest computed tomography demonstrated an infiltrative peripheral lung mass in the right middle lobe, measuring 1.5 cm in diameter. The resected lung tumor had papillary configuration lined by both squamous cell epithelium and mucin-containing glandular epithelium. The papillary stroma showed a fibrovascular core with inflammatory infiltrates. p63 immunostaining was positive in basal and parabasal tumor cells in papillary fronds.
Solitary respiratory papilloma is an unusual benign neoplasm occupying 0.4% of all lung tumors (1). This tumor displays three histologic categories including squamous cell, glandular and mixed squamous cell and glandular papilloma (2). Among these subclasses, the mixed type of papilloma is an extremely rare pathologic condition that has been reported in only few cases in the English literature. Mixed papilloma is typically presented with a central mass (endobronchial type) rather than a peripheral mass (endobronchiolar type) (1). Herein, we present a case of the peripheral type of mixed papilloma in a 54-year-old man.
A 54-year-old man was referred to our hospital with a chief complaint of dyspnea for 10 days. The patient was a smoker and he had a past history of gastric cancer and pulmonary tuberculosis 7 and 20 years ago, respectively. Other medical history and laboratory studies were unremarkable. Thoracic computed tomography revealed a 1.5 cm sized pulmonary nodule with spiculated margin in the right middle lobe (Fig. 1A). Under the clinical impression of lung cancer, right middle lobectomy via video-assisted thoracoscopic surgery was performed for definitive diagnosis and treatment.
The resected lung showed an ill demarcated dark brown solid mass, measuring 1.7×1.5 cm confined to the lung parenchyma lacking pleural adhesion. On microscopic examination, the tumor exhibited papillary configurations filled with bronchiolar and alveolar spaces (Fig. 1B, C). The papillary fronds consisted of heterogeneous components of squamous and glandular epithelial cells and the papillary stalk contained central fibrovascular cores infiltrated with acute and chronic inflammatory cells (Fig. 1D, E). Leaked mucin materials were also noted in some alveolar spaces. The glandular lining cells were mucin-contained columnar or cuboidal epithelial cells, some of which had cytologic atypia. Immunohistochemically, the basal and parabasal cells with a squamoid configuration of papillary fronds showed nuclear staining for p63 (1 : 200, Biocare Medical, Concord, CA, USA) staining (Fig. 1F).
Solitary respiratory papilloma is a benign neoplasm of the lung, which was first classified by Jackson and Jackson in 1932 (3). The current World Health Organization (WHO) classification of lung tumor categorized solitary respiratory papilloma into squamous cell, glandular, and mixed papillomas by histologic characteristics (4). Although human papillomavirus infection or tobacco smoking can be associated with the development of this type of tumor, etiologic and pathologic factors have not been clearly established (1). Solitary respiratory papilloma can lead to some clinical manifestations, such as cough, hemoptysis, fever and less commonly, dyspnea (2). Mixed squamous cell and glandular papilloma is an extremely rare subtype which is usually presented with a central endobronchial mass (4). However, our case was unusual in that the tumor was located in the peripheral endobronchiolar area and caused difficulty in breathing.
The main differential diagnosis of mixed squamous cell and glandular papilloma include well-differentiated squamous cell carcinoma, papillary adenocarcinoma, and other benign neoplasms such as mucus gland adenoma and papillary adenoma (5). Distinguishing between mixed papilloma and carcinomas is very important in determining the surgical extent and postoperative care. In particular, small biopsy specimens can create confusion for pathologists in destinguishing this benign tumor from malignancy. Considering that squamous components are more likely to be neglected in the evaluation of this tumor, immunostaining for p63 and morphologic evaluation can be helpful for differentiating this tumor from adenocarcinoma or squamous cell carcinoma.
Herein, we report an unusual case of mixed squamous cell and glandular papilloma arising from the peripheral lung field and provoking dyspnea. Interestingly, we have previously reported another case which presented with a peripheral mass. Definite pathophysiology or clinical implications including causal factor, recurrence rate and cancer progression risk has not yet been assessed for this peripherally located papilloma due to its extremely rare occurrence rate (4). Therefore, further evaluation should be performed through collection of additional cases. Moreover, although mixed papilloma occurring in the peripheral area is extremely rare, its possibility should not be overlooked in the differential diagnosis of a peripheral lung mass with squamous and glandular epithelial cells.
Figures and Tables
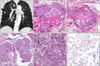 | Fig. 1(A) Chest computed tomography shows a peripheral lung mass with spiculated margin (arrows). (B, C) Low magnification view exhibits a papillary pattern filled with bronchiolar and alveolar spaces (H&E, ×10). (D, E) On high power view, the papillary structures are lined by both components of squamous and glandular epithelial cells. The papillary stalk has central fibrovascular cores with inflammatory infiltration (H&E, ×100). (F) Staining for p63 shows immunoreactivity in basal and parabasal cells in papillary fronds (ABC, ×200). |
References
1. Inamura K, Kumasaka T, Furuta R, et al. Mixed squamous cell and glandular papilloma of the lung: a case study and literature review. Pathol Int. 2011. 61:252–258.

2. Tryfon S, Dramba V, Zoglopitis F, et al. Solitary papillomas of the lower airways: epidemiological, clinical, and therapeutic data during a 22-year period and review of the literature. J Thorac Oncol. 2012. 7:643–648.

3. Jackson C, Jackson CL. Benign tumors of the trachea and bronchi with especial reference to tumor-like formations of inflammatory origin. JAMA. 1932. 99:1747–1754.
4. Sung CO, Kim J, Do IG, Han J. Solitary pulmonary mixed squamous cell and glandular papilloma: a brief case report. Korean J Pathol. 2008. 42:393–395.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download