Abstract
Extra-adrenal myelolipoma is a rare benign tumor which can occur in the abdomen, thorax, or even in the face. We present a case of 58-year-old woman patient with thoracic myelolipoma, which has manifested as three paravertebral masses at the level of T9 and T10. The computed tomography scan showed heterogenous enhancing masses, which contained fat component. She underwent video-assisted thoracoscopic surgery, and the pathologic examination revealed adipose tissue with many hematopoietic cells, consistent with myelolipoma.
Myelolipomas are usually found in the adrenal glands, composed of adipose tissue and normal hematopoietic elements. Extra-adrenal myelolipomas are very rare condition, and their incidence is reported in the order of retroperotineum (mainly in perirenal space), presacral area, thorax, mesentery, stomach, liver, nasal cavity, leptomeninges, and lymph node (1). In the thorax, myelolipoma could be occurred as pleural or mediastinal mass (2), or even paravertebral mass. We report a case of extraadrenal myelolipoma, which is presented as paravertebral masses mimicking neurogenic tumor in the thorax.
A 58-year-old woman complained of intermittent dizziness with history of hypertension and underwent a general health examination. On her laboratory tests were shown the following: anemia, hyperbililubinemia, increased mean corpuscular volume and mean cell hemoglobin, increased osmotic fragility, and poikilocytosis with spherocytes on peripheral blood smear, which were consistent with hereditary spherocytosis. On the low dose chest computed tomography (CT) for general work-up, paravertebral masses were noted and contrast-enhanced helical CT scan was obtained. At the level of T9 and T10, two nodules on the right and one nodule on the left paravertebral area were noted in the posterior mediastinum. The nodules weres 24 mm, 18 mm, and 16 mm in size. They were well-defined, localized in the paravertebral space, and extensions to the neural foramen or spinal canal were not demonstrated. Adjacent vertebral structures were also patent. All nodules contained fat components, and soft tissue in the medial side showed about 40~50 HU of net enhancement (Fig. 1A, B). Two months after splenectomy as the treatment for hereditary spherocytosis, anemia and hyperbililubinemia were corrected. Video-assisted thoracoscopic excision was performed for three nodules in the bilateral paravertebral space for the exclusion of malignancy. During the operation, soft and pink tan colored, lobular shape nodules were noted, covered with pleura (Fig. 1C, D). On pathologic examination, the resected tumors were relatively well-circumscribed and ovoid soft mass, measuring 2 cm in the largest diameter. The cut surface was pale yellow to deep red or brown in color, depending on the proportion of fat and hematopoeitic elements. The mass was consisted of a mixture of mature adipose tissue and hematopoietic elements resembling bone marrow. There were full trineage maturation of the hematopoietic component including myeloid, erythroid, and megakaryotic lines (Fig. 1E~G). Immunohistochemical stain for myeloperoxidase polyclonal antibody (MPO, a biotinavidin peroxidase complex method; 1:20,000, Daco, Glostrup, Denmark) highlighted myeloid cell (Fig. 1H), which was consistent with myelolipoma. So far, she has no symptoms and no evidence of recurrence in the thorax.
Extra-adrenal myelolipomas in the thorax are rare; and paravertebral thoracic myelolipoma is extremely rare. Pathogenesis of myelolipoma is unclear. Some have reported associations between myelolipoma and obesity, hypertension, chronic inflammation, carcinoma, previous trauma, and treatment with exogenous steroids. Myelolipoma is originated from embryonal rests of osteogenic tissue and embolism of bone marrow cells via the blood stream or metaplastic change. Majority of cases are related to anemic condition such as hereditary spherocytosis and thalassemia. Schön et al. (3) have suggested that anemic clinical condition is related to the occurrence of myelolipoma, as a kind of extramedullary hematopoiesis, with a composition of heterotopic bone marrow and adipose tissue. Another suggestion for development of myelolipoma is the origin from metaplasia of adrenocortical cells, as ectopic adrenal tissue. Exo- or endogenous corticosteroid may have some effects on the pathogenesis.
As in the reported cases, the patient's manifestation of myelolipoma was bilateral paravertebral nodular lesions. Suggested differential diagnosis was neurogenic tumor, considering the well-defined paravertebral mass containing fat components. For fat-containing paravertebral mass, other radiologic differential diagnoses include angiolipoma, teratoma, and epidural lipomatosis. But multiplicity and bilaterality, without adjacent bony disruption, favor the possibility of conditions due to hematogenous problems, including chloroma and extramedullary hematopoiesis. Magnetic resonance imaging is helpful for the differentiation in terms of the detection of interspersed fat within hematopoietic tissue component. The imaging, reveals a high signal intensity of fat component on T1- and T2-weighted spin echo images and chemical shifting on in- and opposed-phases; and shows low signal intensity on T1-weighted images and intermediate signal intensity on T2-weighted images in case of hematopoietic elements (4). Hemorrhage in the lesion can show different signal intensity following its bleeding age. Actually, myelolipoma and extramedullary hematopoiesis may have similar imaging and histopathologic findings, but extramedullary hematopoiesis usually does not contain macroscopic fat component, and this point may help the differential diagnosis.
Bone marrow scintigraphy can detect the myeloid elements. The object of murine monoclonal antibody Mab BW 250/183 is the cellular components of granulocytes and their progenitors. The hematopoietic components in the myelolipoma can be demonstrated on the scintigraphy; and this may help other kinds of fat containing tumor (5).
Pathologically, myelolipomas contain mature fat and full trineage maturation of the hematopoietic component. The aggregation of lymphocytes, plasma cells, and hemosiderin-laden macrophages can be associated. Also hemorrhagic foci can be seen, but primitive adipose tissue, other mesenchymal tissues, or bones are not present. The detection of myelocytic component can be achieved MPO polyclonal antibody, chloroacetate esterase stain, or CD15 immunohistochemical stain.
If myelolipomas is nonhemorrhagic and asymptomatic, a conservative management is enough after the pathologic confirmation such as percutaneous biopsy. Surgical excision can be required in the case of uncertain diagnosis or if the lesion results some symptoms.
Although thoracic myelolipoma is very rare, it can be considered as differential diagnosis for bilateral and multiple fat-containing paravertebral tumors. Pathologic tissue confirmation is often required for its diagnosis, but preoperative suggestion of myelolipoma can prevent unnecessary surgery.
Figures and Tables
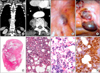 | Fig. 1(A, B) On computed tomography images, three paravertebral nodules were noted. They were well-defined and lobular shape, containing fat components. After contrast administration, they showed enhancement. No invasion to adjacent structures was seen. (C, D) During the operation, the lesions were presented as pink tan colored, lobular shape nodules, covered with pleura. (E~G) The lesions were consisted of mature adipose tissue and hematopoietic elements resembling bone marrow. Full trineage maturation of the hematopoietic component includes myeloid, erythroid, and megakaryotic lines (E, H&E, ×1; F, H&E, ×100; G, H&E, ×200). (H) Immunohistochemical stain for myeloperoxidase polyclonal antibody showed myeloid cell (×200). |
References
1. Franiel T, Fleischer B, Raab BW, Füzesi L. Bilateral thoracic extraadrenal myelolipoma. Eur J Cardiothorac Surg. 2004. 26:1220–1222.

3. Schön HR, Emmerich B, Arnold H, Maubach PA, Becker K, Rastetter J. Hemolytic anemia with pyruvate kinase deficiency presenting as paravertebral myelolipoma. Klin Wochenschr. 1984. 62:133–137.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download