Abstract
Bupropion is widely used for the treatment of depressive disorder and smoking cessation. Hyponatremia, including a syndrome of inappropriate secretion of antidiuretic hormone (SIADH), is not rare complication of treatment with antipsychotic drugs. We report a 60-year-old man who experienced severe hyponatremia after a treatment with bupropion for depressive disorder for the first time in the Korea.
Go to : 
Antidepressants, including the selective serotonin reuptake inhibitor (SSRI) and the tricyclic antidepressants (TCA) often cause hyponatremia1-5). Bupropion is an atypical antidepressant and smoking cessation aid. The drug is a non-tricyclic antidepressant and its primary pharmacological action is to inhibit norepinephrine-dopamine reuptake. Although bupropion does not act as TCA and SSRI, there are few case reports describing how bupropion is associated with hyponatremia1,2). We present a case of bupropion induced hyponatremia for the first time in the Korea.
Go to : 
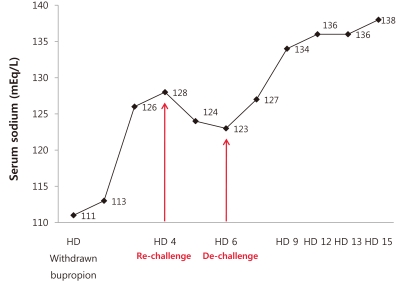
A 60-year-old man came to a hospital complaining that he was experiencing fatigue and general weakness of body for 3 days. He had a history of hypertension and old myocardial infarction that stents were placed on May 2009. He was also diagnosed with depressive disorder in psychiatry on December 2009. He had been treated with antidepressant agents, including escitalopram (SSRI) 10 mg, mirtazapine (TCA) 15 mg, clonazepam 0.5 mg and alprazolam 0.25 mg twice per day. In addition, he was prescribed aspirin, clopidogrel, simvastatin and telmisartan for hypertension and old myocardial infarction. Mirtazapine was substituted with bupropion due to the patient gaining weight in late December 2010. About a week later, the patient began complaining of the symptoms stated above. He had no generalized edema and postural hypotension. His neurological signs were normal. Chest X-ray did not show any pathologic abnormality in both lungs, and his left ventricular ejection fraction was 56.2% on echocardiography. His sodium level was markedly decreased to 111 mgEq/L from 137 mgEq/L during 2 months. The level of another electrolytes were potassium 3.8 mEq/L, chloride 80 mgEq/L, uric acid 5.9 mg/dL, BUN 24.5 mg/dL and creatinine 1.3 mg/dL. His serum osmolality and urine osmolality were 240 and 598 mOsm/kg, respectively. The level of urine sodium and urine potassium were 41 and 82.0 mEq/L. Arterial blood gas analysis revealed a pH 7.413, pCO2 35.9 mmHg, pO2 77.2 mmHg, HCO3- 22.5 mEq/L and 95.3% O2 Saturation. His thyroid function test was within normal range, T3 0.62 ng/mL, free T4 2.00 ng/dL and TSH 0.59 ulU/mL. The level of plasma adrenocorticotropic hormone (ACTH) was 29.6 pg/mL (reference range: 0-60 pg/mL). We performed rapid ACTH test and it showed the level of serum cortisol after injection of ACTH, did not increase sufficiently(from 9.1 µg/dL to 13.0 µg/dL). However, aldosterone was raised up to 219 pg/mL from 45 pg/mL at basal, such as a pattern consistent with secondary adrenal insufficiency. (The psychiatric drugs were thought to be the offending agents and were withdrawn from the treatment. We also added low dose of prednisolone because of secondary adrenal insufficiency.) Three days later, his symptoms were improved and sodium level slowly increased to 128 mEq/L. At that time, the patient again complained of severe anxiety and insomnia. His medications were restarted, including bupropion, escitalopram, mirtazapine and alprazolam. Two days later, his serum sodium was decreased again from 128 mEq/L to 123 mEq/L. He was stopped bupropion immediately (which was thought to cause the hyponatremia) but, had not been restricted water intake. Two weeks after withdrawn bupropion, his serum sodium had returned to the normal range, which was 138 mEq/L. It did not decrease thereafter and his symptoms began improving. There was no evidence of internal malignancy suggesting a syndrome of inappropriate secretion of antidiuretic hormone (SIADH) in a brain, chest and abdominal computed tomography as well as tumor markers including alpha fetoprotein and prostate specific antigen. Although the level of carcinoembryonic antigen (CEA) was slightly elevated to 6.51 ng/mL (0-4.7), we could not find any cancerous lesions in colonoscopy.
Go to : 
Hyponatremia is defined as a serum level of less than 135 mEq/L and the most common electrolyte disorder6). However, hyponatremia is not rare condition following a treatment with SSRI and antipsychotic drugs1-5). Case reports of hyponatremia associated with SSRI began appearing in 1989. Currently, about 50 case reports have appeared in print. German multicenter drug surveillance program7) found out that about 0.06% patients who took SSRI developed severe hyponatremia. However, in certain subgroups the incidence appears to be much higher. Estimates of hyponatremia associated with SSRI and SNRI use vary from 0.5-32%. Curiously, there are only few case reports published regarding bupropion induced hyponatremia1,2). Some experts have suspected the mechanism that serotonin plays a role in regulating the secretion and release of alcoholdehydrogenase (ADH)7-9). Nevertheless, the exact mechanism associated with bupropion and hyponatremia remains unknown. Bupropion perhaps release ADH as usual.
Aging is one of the most significant risk factor for antipsychotic agent induced hypontremia10). Incidence rate ranges from 12% to 33% in the elderly population8,11). The cause of high risk in elderly patients may be altered renal function, increased ADH secretion, increased sensitivity to ADH, presence of concomitant illnesses and other medications that contribute to hyponatremia10). Other risk factors include diuretic drug use12), recent or current pneumonia, lower base line serum sodium levels and lower body mass index11). Monitoring of electrolytes is indicated for especially the elderly patients taking SSRI and bupropion in this context. The serum sodium levels checked at the start of therapy and then weekly during the first month of treatment13). If the patient develops mental status change including lethargy, delirium, nausea, or seizures, we should immediately check serum sodium levels. Symptomatic hyponatremia is a medical emergency requiring rapid correction to prevent the worsening of brain edema but, hyponatremia must be corrected slowly (< 10-12 mEq/L within the first 24 hours, and < 18 mEq/L within the first 48 hours) to avoid osmotic myelinolysis14).
This patient has a history of hypertension, old myocardial infarction, benign prostate hypertrophy and depressive disorder that requires a variety of medications. At first, the psychiatric drugs, including SSRI and bupropion, were thought to be the offending agents for hyponatremia, so they were withdrawn from the treatment. However, the time course of the development of the severe hyponatremic episodes corresponds to begin treatment with bupropion. Also, after re-challenge with bupropion, the hyponatremic episode developed again. After stopping bupropion, the serum sodium concentration was normalized. We also added low dose of prednisolone because of secondary adrenal insufficiency. Although, secondary adrenal insufficiency could have induced hyponatremia, it does not lead to severe hyponatremia such as in our case, since the secretion of aldosterone is intact during rapid ACTH test. Therefore, we believe that bupropion was thought to cause the hyponatremia in this case. A detailed serum sodium levels should be checked closely follow-up in this patient. In conclusion, elderly patients who are taking antipsychotic drugs, especially bupropion, should carefully monitor their serum sodium levels, so could avoid any potential fatal side effects of bupropion induced hyponatremia.
Go to : 
References
1. Bagley SC, Yaeger D. Hyponatremia associated with bupropion, a case verified by rechallenge. J Clin Psychopharmacol. 2005; 25:98–99. PMID: 15643110.

2. Liskin B, Walsh BT, Roose SP, Jackson W. Imipramine-induced inappropriate ADH secretion. J Clin Psychopharmacol. 1984; 4:146–147. PMID: 6429213.

3. Malik AR, Wolf PK, Ravasia S. Recurrent paroxetine-induced hyponatremia. Can J Psychiatry. 2004; 49:785. PMID: 15633859.
4. Atalay A, Turhan N, Aki OE. A challenging case of syndrome of inappropriate secretion of antidiuretic hormone in an elderly patient secondary to quetiapine. South Med J. 2007; 100:832–833. PMID: 17713312.

5. Madhusoodanan S, Bogunovic OJ, Moise D, Brenner R, Markowitz S, Sotelo J. Hyponatraemia associated with psychotropic medications. A review of the literature and spontaneous reports. Adverse Drug React Toxicol Rev. 2002; 21:17–29. PMID: 12140905.
6. Kim SW, Yeom CH, Na MY, Kim NH, Choi KC. Hyponatremia. Korean J Nephrol. 2001; 20(Suppl 3):S378–S390.
7. Degner D, Grohmann R, Kropp S, et al. Severe adverse drug reactions of antidepressants: results of the German multicenter drug surveillance program AMSP. Pharmacopsychiatry. 2004; 37(Suppl 1):S39–S45. PMID: 15052513.

8. Fabian TJ, Amico JA, Kroboth PD, et al. Paroxetine-induced hyponatremia in older adults: a 12-week prospective study. Arch Intern Med. 2004; 164:327–332. PMID: 14769630.
9. Jacob S, Spinler SA. Hyponatremia associated with selective serotonin-reuptake inhibitors in older adults. Ann Pharmacother. 2006; 40:1618–1622. PMID: 16896026.

10. Liu BA, Mittmann N, Knowles SR, Shear NH. Hyponatremia and the syndrome of inappropriate secretion of antidiuretic hormone associated with the use of selective serotonin reuptake inhibitors: a review of spontaneous reports. CMAJ. 1996; 155:519–527. PMID: 8804257.
11. Wee R, Lim WK. Selective serotonin re-uptake inhibitors (SSRIs) and hyponatraemia in the elderly. Int J Geriatr Psychiatry. 2004; 19:590–591. PMID: 15211542.
12. Hwang KS, Kim GH. Thiazide-induced hyponatremia. Electrolyte Blood Press. 2010; 8:51–57. PMID: 21468197.

13. Rottmann CN. SSRIs and the syndrome of inappropriate antidiuretic hormone secretion. Am J Nurs. 2007; 107:51–58. quiz 58-59. PMID: 17200634.

14. Bea EH. Management of chronic asymptomatic hyponatremia. Korean J Med. 2011; 80:15–19.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download