Abstract
Ammonia metabolism is a fundamental process in the maintenance of life in all living organisms. Recent studies have identified ammonia transporter family proteins in yeast (Mep), plants (Amt), and mammals (Rh glycoproteins). In mammalian kidneys, where ammonia metabolism and transport are critically important for the regulation of systemic acid-base homeostasis, basolateral Rh B glycoprotein and apical/basolateral Rh C glycoprotein are expressed along the distal nephron segments. Data from experimental animal models and knockout mice suggest that the Rh glycoproteins appear to mediate important roles in urinary ammonia excretion.
Renal ammonia metabolism and transport are critically important for the regulation of systemic acid-base homeostasis1-5). Ammonia exists in two molecular forms, NH3 gas and NH4+ ion. It has traditionally been thought that NH3 crosses plasma membranes via lipid diffusion and that NH4+ requires specific transporter proteins3-5). Recent studies have provided new insights into the mechanisms of renal ammonia transport. The traditional theory of simple NH3 diffusion has been replaced by a regulated model of NH3 and NH4+ transport. Indeed, when dissolved in water, ammonia exists predominantly as the NH4+ ion with a pKa of about 9 under physiological conditions6). Moreover, there is an increasing amount of evidence that even movement of gaseous molecules such as CO2 and O2 requires specific proteins to accelerate the transport where the diffusion is too slow for physiological needs7, 8). In the kidney, it has been known that at least two ammonia transporter proteins are expressed.
Ammonia is an important molecular form of nitrogen, and mediates a key role in nitrogen nutrition for plants and soil microorganisms. It is therefore not surprising that botany-related research discovered the first ammonia-specific transporters. In 1994, simultaneous studies by Marini et al.9) and Ninnemann et al.10) cloned the Mep1 gene encoding an ammonium transporter in yeast, Saccharomyces cerevisiae and from plants, Amt1, respectively. Both Mep and Amt mediated high affinity ammonium transport activity when expressed in yeast deficient in endogenous ammonium transporters9, 10). Their transport activity was insensitive to other cations including sodium and potassium. Subsequent studies identified multiple additional members of the ammonia transporter family. Yeasts have at least three members, Mep1, Mep2 and Mep3, and plants have at least two members, Amt1 and Amt2.
The Rh blood group, named after the Rhesus monkey, is very important in the field of transfusion medicine. There are two Rh genes, RHD and RHCE, and numerous genetic rearrangements between them produce a lot of distinct antigens, up to 49. Unlike most cell surface molecules, the RhD and RhCE are not glycosylated but they are closely associated with a glycosylated protein with a previously unknown function, Rh-associated glycoprotein (RhAG).
The first suggestion that Rh glycoproteins might be ammonia transporters was the findings by Marini et al. that the erythroid Rh antigen subunit, RhAG, and a kidney homologue, which they termed Rh glycoprotein-kidney (RhGK), have similar secondary structure to the yeast and plant ammonia transporters and could promote ammonium transport in yeast11, 12). In 2000, a separate group (Li et al.)13) cloned a novel Rh glycoprotein homologue, Rh C glycoprotein, from both human (RhCG) and mouse (Rhcg), which they reported to be predominantly expressed in the kidney, central nervous system and testis. RhGK and RhCG/Rhcg are now known to be identical and RhCG/Rhcg is the term preferred by most investigators. The following year, Li et al., identified another new member of mammalian ammonia transporter family, Rh B glycoprotein (RhBG/Rhbg)14). In mammals, three ammonia transporter family members, RhAG/Rhag, RhBG/Rhbg, and RhCG/Rhcg have been identified so far.
As Hidden Markov Modeling techniques predicted, the atomic structures of the ammonia transporter family showed that they are integral proteins crossing the membrane 11 times. Khademi et al. resolved the crystallographic structure of a bacterial ammonia transporter, AmtB, at 1.35 Å resolution and revealed that they form symmetric trimers in the membrane15). This report identified that AmtB has the same structure in both the absence and presence of ammonia or methylammonia, suggesting that it may be a channel rather than a transporter. However, Zheng et al.16) reported that slow conformational changes were needed for transient pore opening of AmtB and that its transport rate was rather typical for transporters and far below that of open channels and thus they concluded that AmtB was a transporter, not a channel. At the two ends of the pore, AmtB has recruitment vestibules for NH4+. These recruitment sites are able to change the pKa of the ammonia buffer reaction, resulting in preferential conversion of NH4+ to NH3 and H+. The NH3 appears to traverse the protein through a narrow hydrophobic element which allows only the passage of NH3 but not the NH4+ ion. Thus, Khademi et al. concluded that AmtB might not mediate the net transfer of protons and not directly alter the membrane potential, although several previous studies showed that ammonia translocation is affected by pH and voltage gradients4, 5, 9). Whether other ammonia transporter family members mediate electrogenic ammonia transport or electroneutral NH4+/H+ ion exchange remains an active area of investigation. Some bacterial ammonia transporter family members have been shown to mediate electrogenic NH4+ transport. Whether this involves parallel NH3 and H+ transport or separate NH4+ transport has not been determined.
To date, no studies have reported that RhAG/Rhag is expressed in renal tubular epithelial cells. In particular, there is no evidence of RhAG/Rhag expression in the kidney5).
In the mouse and rat kidney, Rhbg is expressed in the basolateral membrane throughout the distal tubular epithelium (Fig. 1)17-22). In 2003, Quentin et al. microdissected nephron segments and performed RT-PCR experiments19). The expression level of Rhbg mRNA was highest in the connecting tubule (CNT), cortical collecting duct (CCD), and outer medullary collecting duct (OMCD) and lowest in distal convoluted tubule (DCT). In both the mouse and rat kidney, Rhbg appeared to be expressed in all cells within the CNT. In the CCD, cells exhibited two distinct patterns of labeling; the principal cells had thin or no basolateral staining, whereas the intercalated cells had more intense basolateral staining. The number of stained cells fell sharply in the inner medulla and none was found in deeper regions of the inner medulla19).
The same year, a separate group (Verlander et al.) published a more detailed study in the mouse kidney22). The cellular distribution of Rhbg was similar with the report of Quentin et al.. However, Verlander et al. demonstrated that a subpopulation of intercalated cells do not express detectable Rhbg immunoreactivity. Colocalization with pendrin, an apical anion exchanger present in type B and non-A-non-B intercalated cells, revealed that CNT pendrin-positive cells (non-A-non-B intercalated cells) typically exhibited basolateral Rhbg immunoreactivity, whereas CCD pendrin-positive cells (type B intercalated cell) were negative for Rhbg. Subsequent studies also confirmed similar findings in the rat kidney.
The distribution pattern of RhBG has not been established in the human kidney. Brown et al., reported, despite RhBG mRNA expression, that they could not detect RhBG protein expression in human tissue lysates or tissue sections, although the same antibodies detected Rhbg in rat tissues23). Whether this indicates a lack of RhBG protein expression or unexpected lack of antibody-antigen recognition is not to be determined definitively at present.
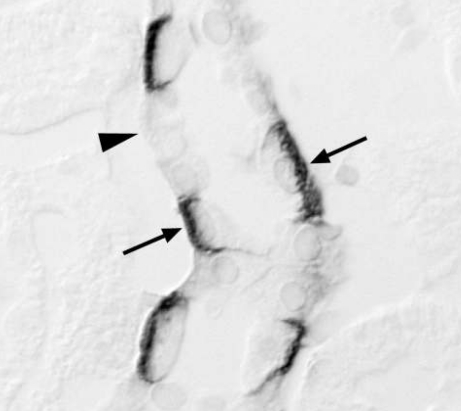
In the kidney, RhCG/Rhcg has a similar distribution as Rhbg along nephron segments. Although initial studies reported only apical immunolabeling22, 24), recent studies have yielded conflicting results regarding the membrane location of RhCG/Rhcg17, 18, 20, 21, 25, 26). Both apical and basolateral immunolabeling have been observed in the kidney of rat, human, and some mouse species (Fig. 2). Kim et al.26) performed extensive morphological studies using immunogold electron microscopy in Balb/c, C57BL/6, C3H, and Black Swiss 129 mice and showed both apical and basolateral Rhcg expression in all strains, although strain-dependent differences in the intensity of basolateral Rhcg immunolabel were apparent. Moreover, in the human kidney, RhCG expression is predominantly basolateral, with a lesser degree of apical immunoreactivity25). Basolateral Rhcg expression increases in parallel with urine ammonia excretion in experimental animal models, suggesting that basolateral Rhcg may play a role in certain physiological conditions. The trafficking mechanisms of the same protein to both the apical and basolateral plasma membrane remain to be established.
Chronic metabolic acidosis increases net acid excretion through urinary ammonia metabolism. Seshadri et al.20) demonstrated that chronic HCl ingestion increased urinary ammonia excretion 25 fold and increased Rhcg protein expression. Rhcg expression was increased in the outer medulla and inner medulla but not altered in the cortex. Chronic metabolic acidosis also altered the subcellular distribution of the ammonia transporter protein21). In both intercalated cells and principal cells, apical plasma membrane Rhcg significantly increased, whereas, intracellular Rhcg decreased in response to acidosis. However, chronic metabolic acidosis did not alter Rhbg protein expression or immunoreactivity in the cortex, outer medulla, or inner medulla.
Similar changes in subcellular Rhcg localization were observed in a reduced renal mass-chronic renal failure model18). Despite a substantial decrease in nephron number, 5/6 ablation-infarcted kidneys maintained normal ammonia excretion and acid-base homeostasis. This was associated with increased apical and basolateral Rhcg expression in collecting duct cells. In contrast, loss of ammonia transporting cells may contribute to the development of metabolic acidosis. In renal ischemia-reperfusion injury, Rh glycoproteins-positive collecting duct cells specifically detached into the tubular lumen and underwent apoptosis resulting in decreased urinary ammonia excretion17). In chronic cyclosporine nephropathy there was development of metabolic acidosis and an accompanying decrease in Rhcg expression27). Moreover, urinary ammonia excretion was inappropriately low, suggesting that the decreased Rhcg expression, by decreasing ammonia excretion, leads to the development of metabolic acidosis.
Chambrey et al.28) inactivated the mouse Rhbg gene by insertional mutagenesis and examined whether the mice displayed disturbed ammonia metabolism. Unexpectedly, the Rhbg knockout mice did not exhibit encephalopathy or renal tubular acidosis and adapted well to a chronic acid-load by increasing urinary NH4+ excretion approximately 3-4 fold. Moreover, NH3 or NH4+ entry across the basolateral membrane of collecting duct cells was identical in the knockout and wild-type mice suggesting that Rhbg may not be a critical determinant of ammonia excretion by the kidney. However, one cannot exclude the possibility at present that basolateral Rhcg expression is able to compensate for the lack of Rhbg and thus maintain normal ammonia transport.
In contrast, both global and collecting duct-specific Rhcg deletion altered renal urinary ammonia excretion29, 30). Biver et al.29) deleted the Rhcg gene in mice and demonstrated that Rhcg absence resulted in marked reduction of ammonia movement across the collecting-duct epithelial cells and a significant drop in blood pH. Male Rhcg-knockout mice also represented a reduction in reproductive capability associated with altered epididymal function. Lee et al.30) generated collecting duct-specific Rhcg knockout mice having loxP sites flanking exons 5-9 of the Rhcg gene and expressing Cre-recominase under control of the Ksp-cadherin promoter. The collecting duct-specific Rhcg knockout mice excreted less urinary ammonia under basal conditions and developed more severe metabolic acidosis after acid loading. Thus, collecting duct Rhcg expression is necessary for normal renal ammonia transport, both under basal conditions and in response to metabolic acidosis.
Ammonia transporter family members, Rh B glycoprotein and Rh C glycoprotein, are expressed in mammalian kidneys along the distal nephron segments. Basolateral Rh B glycoprotein expression does not change with metabolic acidosis and genetic ablation of Rhbg does not alter renal ammonia excretion, either. Rh C glycoprotein exhibits both apical and basolateral membrane localization, albeit with species- and strain-dependent variations in basolateral Rhcg immunolabel intensity. Chronic metabolic acidosis increases Rhcg protein abundance and Rhcg deletion alters renal urinary ammonia excretion. These data suggest that collecting duct ammonia secretion may be mediated, at least, by RhCG/Rhcg.
References
1. Alper SL, Natale J, Gluck S, Lodish HF, Brown D. Subtypes of intercalated cells in rat kidney collecting duct defined by antibodies against erythroid band 3 and renal vacuolar H+-ATPase. Proc Natl Acad Sci USA. 1989; 86:5429–5433. PMID: 2526338.
2. Kim J, Kim YH, Cha JH, Tisher CC, Madsen KM. Intercalated cell subtypes in connecting tubule and cortical collecting duct of rat and mouse. J Am Soc Nephrol. 1999; 10:1–12. PMID: 9890303.

3. Knepper MA, Packer R, Good DW. Ammonium transport in the kidney. Physiol Rev. 1989; 69:179–249. PMID: 2643123.

4. Weiner ID, Verlander JW. Renal and hepatic expression of the ammonium transporter proteins, Rh B Glycoprotein and Rh C Glycoprotein. Acta Physiol Scand. 2003; 179:331–338. PMID: 14656370.

5. Weiner ID. The Rh gene family and renal ammonium transport. Curr Opin Nephrol Hypertens. 2004; 13:533–540. PMID: 15300160.

6. Lang W, Block TM, Zander R. Solubility of NH3 and apparent pK of NH4+ in human plasma, isotonic salt solutions and water at 37 degrees C. Clin Chim Acta. 1998; 273:43–58. PMID: 9620469.
7. Echevarría M, Muñoz-Cabello AM, Sánchez-Silva R, Toledo-Aral JJ, López-Barneo J. Development of cytosolic hypoxia and hypoxia-inducible factor stabilization are facilitated by aquaporin-1 expression. J Biol Chem. 2007; 282:30207–30215. PMID: 17673462.

8. Han KH, Mekala K, Babida V, Kim HY, Handlogten ME, Verlander JW, et al. Expression of the gas transporting proteins, Rh B glycoprotein and Rh C glycoprotein, in the murine lung. Am J Physiol Lung Cell Mol Physiol. in press.
9. Marini AM, Vissers S, Urrestarazu A, Andre B. Cloning and expression of the MEP1 gene encoding an ammonium transporter in Saccharomyces cerevisiae. EMBO J. 1994; 13:3456–3463. PMID: 8062822.

10. Ninnemann O, Jauniaux JC, Frommer WB. Identification of a high affinity NH4+ transporter from plants. EMBO J. 1994; 13:3464–3471. PMID: 8062823.

11. Marini AM, Matassi G, Raynal V, Andre B, Cartron JP, Cherif-Zahar B. The human Rhesus-associated RhAG protein and a kidney homologue promote ammonium transport in yeast. Nat Genet. 2000; 26:341–344. PMID: 11062476.

12. Marini AM, Urrestarazu A, Beauwens R, Andre B. The Rh (rhesus) blood group polypeptides are related to NH4+ transporters. Trends Biochem Sci. 1997; 22:460–461. PMID: 9433124.

13. Liu Z, Chen Y, Mo R, Hui C, Cheng JF, Mohandas N, et al. Characterization of human RhCG and mouse Rhcg as novel nonerythroid Rh glycoprotein homologues predominantly expressed in kidney and testis. J Biol Chem. 2000; 275:25641–25651. PMID: 10852913.

14. Liu Z, Peng J, Mo R, Hui C, Huang CH. Rh type B glycoprotein is a new member of the Rh superfamily and a putative ammonia transporter in mammals. J Biol Chem. 2001; 276:1424–1433. PMID: 11024028.

15. Khademi S, O'Connell J 3rd, Remis J, Robles-Colmenares Y, Miercke LJ, Stroud RM. Mechanism of ammonia transport by Amt/MEP/Rh: structure of AmtB at 1.35 A. Science. 2004; 305:1587–1594. PMID: 15361618.

16. Zheng L, Kostrewa D, Bernèche S, Winkler FK, Li XD. The mechanism of ammonia transport based on the crystal structure of AmtB of Escherichia coli. Proc Natl Acad Sci USA. 2004; 101:17090–17095. PMID: 15563598.
17. Han KH, Kim HY, Croker BP, Reungjui S, Lee SY, Kim J, et al. Effects of Ischemia-reperfusion Injury on Renal Ammonia Metabolism and the Collecting Duct. Am J Physiol Renal Physiol. 2007; 293:F1342–F1354. PMID: 17686949.

18. Kim HY, Baylis C, Verlander JW, Han KH, Reungjui S, Handlogten ME, et al. Effect of Reduced Renal Mass on Renal Ammonia Transporter Family, Rh C Glycoprotein and Rh B Glycoprotein, Expression. Am J Physiol Renal Physiol. 2007; 293:F1238–F1247. PMID: 17652373.

19. Quentin F, Eladari D, Cheval L, Lopez C, Goossens D, Colin Y, et al. RhBG and RhCG, the putative ammonia transporters, are expressed in the same cells in the distal nephron. J Am Soc Nephrol. 2003; 14:545–554. PMID: 12595489.

20. Seshadri RM, Klein JD, Kozlowski S, Sands JM, Kim YH, Han KH, et al. Renal Expression of the Ammonia Transporters, Rhbg and Rhcg, In Response to Chronic Metabolic Acidosis. Am J Physiol Renal Physiol. 2006; 290:F397–F408. PMID: 16144966.

21. Seshadri RM, Klein JD, Smith T, Sands JM, Handlogten ME, Verlander JW, et al. Changes in subcellular distribution of the ammonia transporter, Rhcg, in response to chronic metabolic acidosis. Am J Physiol Renal Physiol. 2006; 290:F1443–F1452. PMID: 16434569.

22. Verlander JW, Miller RT, Frank AE, Royaux IE, Kim YH, Weiner ID. Localization of the ammonium transporter proteins RhBG and RhCG in mouse kidney. Am J Physiol Renal Physiol. 2003; 284:F323–F337. PMID: 12388412.
23. Brown AC, Hallouane D, Mawby WJ, Karet FE, Saleem MA, Howie AJ, et al. RhCG is the major putative ammonia transporter expressed in the human kidney, and RhBG is not expressed at detectable levels. Am J Physiol Renal Physiol. 2009; 296:F1279–F1290. PMID: 19357182.

24. Eladari D, Cheval L, Quentin F, Bertrand O, Mouro I, Cherif-Zahar B, et al. Expression of RhCG, a new putative NH3/NH4+ transporter, along the rat nephron. J Am Soc Nephrol. 2002; 13:1999–2008. PMID: 12138130.
25. Han KH, Croker BP, Clapp WL, Werner D, Sahni M, Kim J, et al. Expression of the ammonia transporter, Rh C glycoprotein, in normal and neoplastic human kidney. J Am Soc Nephrol. 2006; 17:2670–2679. PMID: 16928804.

26. Kim HY, Verlander JW, Bishop JM, Cain BD, Han KH, Igarashi P, et al. Basolateral Expression of the ammonia transporter family member, Rh C Glycoprotein, in the Mouse Kidney. Am J Physiol Renal Physiol. 2009; 296:F543–F555. PMID: 19129254.

27. Lim SW, Ahn KO, Kim WY, Han DH, Li C, Ghee JY, et al. Expression of ammonia transporters, Rhbg and Rhcg, in chronic cyclosporine nephropathy in rats. Nephron Exp Nephrol. 2008; 110:e49–e58. PMID: 18776723.

28. Chambrey R, Goossens D, Bourgeois S, Picard N, Bloch-Faure M, Leviel F, et al. Genetic ablation of Rhbg in the mouse does not impair renal ammonium excretion. Am J Physiol Renal Physiol. 2005; 289:F1281–F1290. PMID: 16077082.

29. Biver S, Belge H, Bourgeois S, Van Vooren P, Nowik M, Scohy S, et al. A role for Rhesus factor Rhcg in renal ammonium excretion and male fertility. Nature. 2008; 456:339–343. PMID: 19020613.

30. Lee HW, Verlander JW, Bishop JM, Igarashi P, Handlogten ME, Weiner ID. Collecting duct-specific Rh C glycoprotein deletion alters basal and acidosis-stimulated renal ammonia excretion. Am J Physiol Renal Physiol. 2009; 296:F1364–F1375. PMID: 19321595.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download