1. Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J. Harrison's principles of internal medicine. Sjögren's Syndrome. 18th ed. New York: McGraw-Hill;2012. p. 2770–2773.
2. Goules AV, Tatouli IP, Moutsopoulos HM, Tzioufas AG. Clinically significant renal involvement in primary Sjogren's syndrome: clinical presentation and outcome. Arthritis Rheum. 2013; 65:2945–2953. PMID:
24166794.
3. Seror R, Ravaud P, Bowman SJ, et al. EULAR Sjogren's syndrome disease activity index: development of a consensus systemic disease activity index for primary Sjogren's syndrome. Ann Rheum Dis. 2010; 69:1103–1109. PMID:
19561361.
4. Francois H, Mariette X. Renal involvement in primary Sjogren syndrome. Nat Rev Nephrol. 2016; 12:82–93. PMID:
26568188.
5. Yilmaz H, Kaya M, Ozbek M, K UU, Safa Yildirim I. Hypokalemic periodic paralysis in Sjogren's syndrome secondary to distal renal tubular acidosis. Rheumatol Int. 2013; 33:1879–1882. PMID:
22212410.

6. Han JS, Kim GH, Kim J, et al. Secretory-defect distal renal tubular acidosis is associated with transporter defect in H(+)-ATPase and anion exchanger-1. J Am Soc Nephrol. 2002; 13:1425–1432. PMID:
12039970.

7. Walsh S, Turner CM, Toye A, et al. Immunohistochemical comparison of a case of inherited distal renal tubular acidosis (with a unique AE1 mutation) with an acquired case secondary to autoimmune disease. Nephrol Dial Transplant. 2007; 22:807–812. PMID:
17205967.

8. Kim HY, Kim SS, Bae EH, Ma SK, Kim SW. Decreased Renal Expression of H(+)-ATPase and Pendrin in a Patient with Distal Renal Tubular Acidosis Associated with Sjogren's Syndrome. Intern Med. 2015; 54:2899–2904. PMID:
26568006.
9. Khandelwal D, Bhattacharya S, Gadodia A, Khadgawat R, Tandon N, Ammini AC. Metabolic bone disease as a presenting manifestation of primary Sjogren's syndrome: Three cases and review of literature. Indian J Endocrinol Metab. 2011; 15:341–345. PMID:
22029009.
10. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23. PMID:
23712442.

11. Fulop M, Mackay M. Renal tubular acidosis, Sjogren syndrome, and bone disease. Arch Intern Med. 2004; 164:905–909. PMID:
15111378.
12. Geng Y, Zhao Y, Zhang Z. Tubulointerstitial nephritis-induced hypophosphatemic osteomalacia in Sjogren's syndrome: a case report and review of the literature. Clin Rheumatol. 2017.
13. Vitali C, Bombardieri S, Jonsson R, et al. Classification criteria for Sjogren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002; 61:554–558. PMID:
12006334.

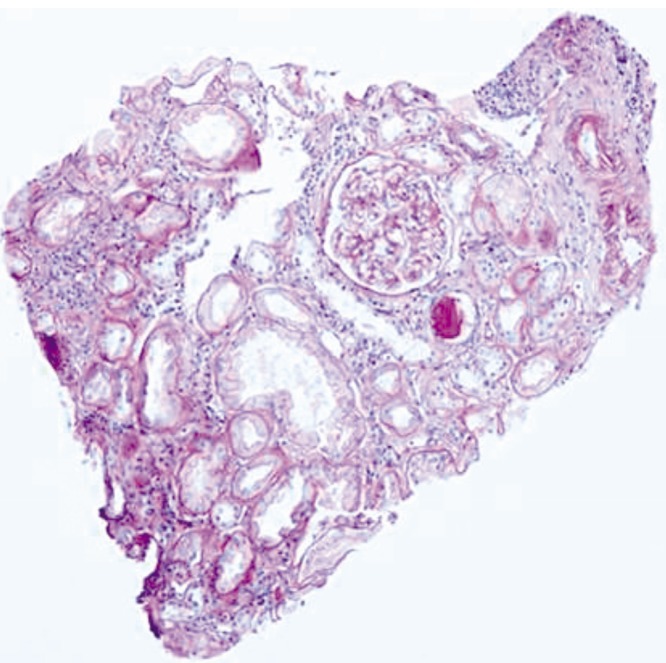
14. Maripuri S, Grande JP, Osborn TG, et al. Renal involvement in primary Sjogren's syndrome: a clinicopathologic study. Clin J Am Soc Nephrol. 2009; 4:1423–1431. PMID:
19679669.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download