Abstract
Non-traumatic, spontaneous urinary bladder rupture is a rare complication of urethral stricture. Furthermore, its symptoms are often nonspecific, and misdiagnosis is common. The authors experienced a case of urethral stricture with spontaneous bladder rupture and bilateral hydronephrosis, mimicking obstructive uropathy attributed to cancer metastasis. A 55-year-old woman was admitted with abdominal pain and distension, oliguria, and an elevated serum creatinine level. She had undergone radical hysterectomy for uterine cervical cancer and received post-operative concurrent chemoradiation therapy 13 years previously. Non-contrast enhanced computed tomography showed massive ascites and bilateral hydronephrosis. The initial diagnosis was acute kidney injury due to obstructive uropathy caused by malignant disease. After improvement of her renal function by bilateral percutaneous nephrostomy catheterization, contrast-enhanced computed tomography and a cytologic examination of ascites showed no evidence of malignancy. However, during retrograde pyelography, a severe urethral stricture was found, and subsequent cystography showed leakage of contrast into the peritoneal cavity and cystoscopy revealed a defect of the posterior bladder wall. After urethral dilatation and primary closure of the bladder wall, acute kidney injury and ascites were resolved.
Go to : 
Non-traumatic, spontaneous urinary bladder rupture is a rare complication of ureterovesical stones, radiotherapy, binge alcohol drinking, or malignancy1). However, its symptoms are often nonspecific, and misdiagnosis is common, and sometimes, it can be a life-threatening event2,3).
We experienced a case presenting as oliguria with hydronephrosis and ascites on admission that was initially misdiagnosed as obstructive uropathy due to metastatic cancer, and later diagnosed as post-radiotherapy urethral stricture and spontaneous rupture of the urinary bladder.
Go to : 
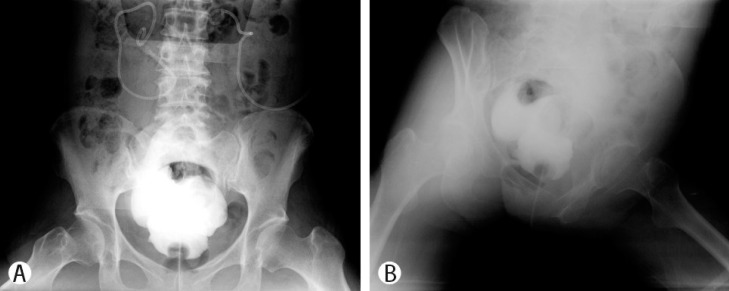
A 55 year-old woman was admitted to Inha University Hospital with abdominal pain, distension, and oliguria. She had undergone radical hysterectomy for uterine cervical cancer and received post-operative concurrent chemoradiation therapy 13 years previously. After a 5-year follow-up period, there was no evidence of the disease state and the patient was asymptomatic, and thus, regular follow-up was discontinued. At the time of admission, she had a 20 pack-year smoking history and consumed 1-2 bottles of alcohol per day, 3-4 times per week. Four days before admission, she visited another hospital with nausea, vomiting, abdominal pain, and abdominal distension of 7 days duration that started after drinking. Physician recommended admission because of the presence of features of acute kidney injury (blood urea nitrogen (BUN): 78mg/dL, creatinine: 4.9mg/dL), but she refused. Four days after discharge, she was admitted at the emergency department of our hospital due to aggravation of her symptoms. She had an acute ill-looking appearance, and her blood pressure, heart rate, respiration rate, and body temperature were 153/112mmHg, 109 pulses per minute, 20 per minute, and 36.6℃, respectively. She complained of general weakness, anorexia, weight loss (6 kg per 1 month), abdominal pain and distension, oliguria, and generalized edema. Physical examination revealed a dry tongue and skin. Chest auscultation showed a regular heart beat without murmur and clear breath sounds without crackle. She had moderate abdominal distension with hypoactive bowel sounds, and mild direct and rebound tenderness of the whole abdomen without organomegaly or a palpable mass. She had edematous lower legs but there was no definite pre-tibial pitting edema. Laboratory findings were as follows: BUN 162.9 mg/dL (reference range, 7.8-26), creatinine 7.74 mg/dL (0.3-1.2), pH 7.24, HCO3- 11.6mmol/L, pCO2 28 mmHg, sodium 119mEq/L, potassium 6.1mEq/L, serum osmolality 313mOsm/Kg. Complete blood cell count results showed mild leukocytosis (13,600/mm3 with 90% neutrophils), elevated hemoglobin (16.5 g/dL), and a normal platelet count. Liver function and coagulation battery tests were normal. Computed tomography (CT) without contrast media showed bilateral hydroureteronephrosis and a large amount of ascites but no evidence of liver cirrhosis (Fig. 1). During hospitalization, her urine output was less than 500mL per day and her renal function, including hyperkalemia and metabolic acidosis, were not improved by conservative management. Hemodialysis was performed for 2 days after admission, but oliguria was not improved. Paracentesis showed no evidence of malignancy or infection. Cell count and chemistry of ascites were as follows: RBC 2/mm3, WBC 42/mm3, polymorphonuclear leukocyte count 11%, glucose 152mg/dL, protein <1.0 g/dL, LDH 25U/L, BUN and creatinine level were not evaluated. On the third hospital day, bilateral percutaneous nephrostomy catheters were inserted, a large amount of urine was drained, her creatinine level decreased dramatically (2 and 4 days after catheter insertions creatinine levels were 1.45 and 0.73mg/dL, respectively), and ascites decreased simultaneously without additional paracentesis. Contrast enhanced CT showed improved hydronephrosis and ascites without evidence of malignancy or an obstructing stone. To determine the cause of the obstruction and to resolve the obstruction by D-J stent insertion, retrograde pyelography was performed. During the procedure, a severe urethral stricture was found, and after urethral dilation, contrast leakage revealed a bladder wall defect open to the peritoneal cavity at the posterior bladder wall (Fig. 2). Multiple bladder wall thinning and severe inflammation were visualized during cystoscopy but no mass or ureteral stricture. The patient was transferred to our urology department and open abdominal surgery was performed to repair the ruptured bladder wall. After surgery, she was well and her renal function remained normal.
Go to : 
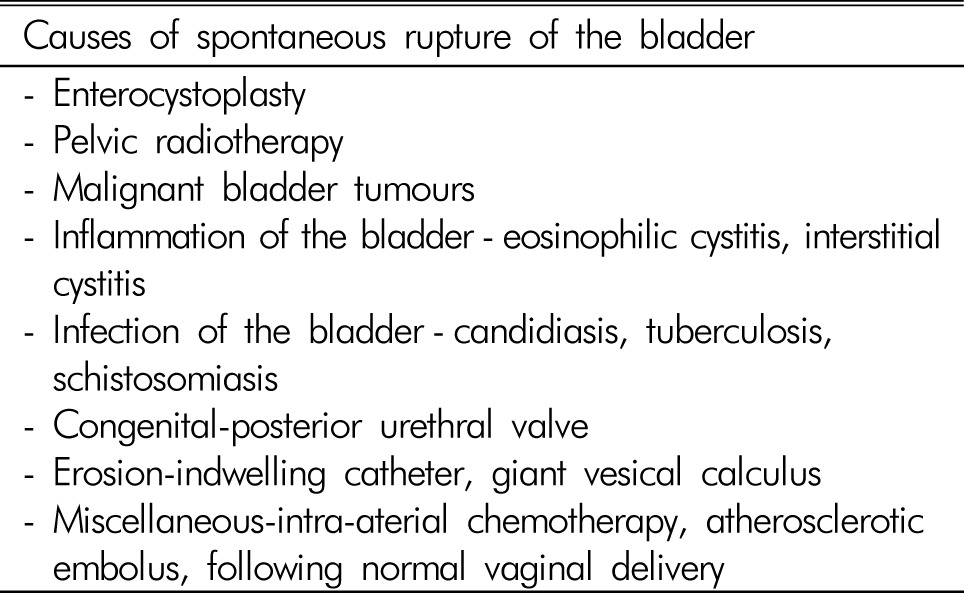
Spontaneous bladder rupture is a rare event, but can be life-threatening. Thus, prompt diagnosis followed by surgical intervention is important to achieve a satisfactory treatment outcome. The symptoms of spontaneous bladder rupture at presentation vary from abdominal distension to acute abdomen, and its most common cause is chronic inflammation (other possible causes are detailed in Table 1)4). Diagnosis is made by history taking and radiologic examination, computed tomography (CT), and urinary cystography. Although cystography is the diagnostic test of choice, Lowe et al. reported the successful use of CT for confirming the diagnosis when cystography was negative or equivocal5). Therefore, CT and cystography in combination appear to provide an accurate, non-invasive means for the diagnosis of bladder pathologies, such as, spontaneous bladder rupture.
Several cases of bladder rupture detected at an early stage have been reported1), and several cases6,7,8,9) of spontaneous bladder rupture presenting as acute kidney injury have been described, but no case of spontaneous bladder rupture combined with definite bilateral hydroureteronephrosis has been previously published. Initially, we considered a diagnosis of post-renal AKI caused by recurrent cervical cancer or intraperitoneal metastasis from an unknown gastrointestinal tract cancer, because the patient was cachexic and complained of substantial weight loss, rather than of urinary frequency, residual urine sensation, or voiding difficulty, and thus, we did not suspect complications of radiotherapy. However, our investigation showed that the primary cause of the bilateral hydronephrosis and spontaneous bladder rupture was severe urethral stricture. Except for mechanical injury, the mechanisms of spontaneous bladder rupture are increased intravesical pressure and weakening of the bladder wall4). In our case, we consider that both mechanisms were involved. That is prior radiotherapy could have weakened the bladder wall10) and caused the urethral stricture, which then progressively increased intravesical pressure and led to bilateral hydronephrosis and finally to spontaneous bladder rupture.
Urethral stricture is a possible complication of radiotherapy for cervical cancer. Theoretically, radiation damagesthe DNA contents of actively dividing cells, and cause chronic fibrosis, progressive endarteritis, and tissue scarring in poorly oxygenated submucosal and muscular tissues, leading to radiation cystitis, hemorrhagic cystitis, neurogenic bladder, and ureteral and urethral stricture. Ureteral stricture and radiation cystitis are the most common long-term post-radiation urinary complications in cervical cancer patients11). However, only a small number of reports have mentioned urethral stricture associated with cervical cancer. In particular, Fujikawa reported that hydronephrosis was the second most common radiation-induced complication rather than urethral stenosis in Japanese patients10).
Some cases of spontaneous bladder rupture have been related to heavy alcohol drinking. Lee et al. reported the case of 65-year-old man with spontaneous bladder rupture after a bout of heavy drinking. This case was diagnosed by testing creatinine level in ascitic fluid following retrograde cystography, and the defect was repaired surgically7). Although the relationship is unclear, some authors have suggested that a diminished sense of voiding and a sudden change in intravesical pressure caused by alcohol intoxication increase the risk of spontaneous bladder rupture12). In our case, alcohol was a possible cause because of her drinking habit and the timing of symptom onset.
In conclusion, we experienced a case of bilateral hydronephrosis and spontaneous rupture of the urinary bladder due to urethral stricture. When a patient with an acute abdomen or ascites with oliguria of unknown origin presents, especially when there is a history of radiotherapy to the pelvis, the possibility of spontaneous bladder rupture should be considered. In cases of bladder rupture, prompt, precise diagnosis and proper surgical treatment are mandatory to avoid the risk of mortality.
Go to : 
References
1. Saleem MA, Mahmoud AM, Gopinath BR. Spontaneous urinary bladder rupture: a rare differential for lower abdominal pain in a female patient. Singapore Med J. 2009; 50:e410–e411. PMID: 20087542.
2. Limon O, Unluer EE, Unay FC, Oyar O, Sener A. An unusual cause of death: spontaneous urinary bladder perforation. Am J Emerg Med. 2012; 30:2081.e3–2081.e5. PMID: 23158061.

3. Albrecht K, Günther D, Oelke M, Wilke N, Wagner C, Törger HD. Spontaneous rupture of the urinary bladder. Arch Kriminol. 2004; 213:154–164. PMID: 15328924.
4. Basavaraj DR, Zachariah KK, Feggetter JGW. Acute abdomen - remember spontaneous perforation of the urinary bladder. J R Coll Surg Edinb. 2001; 46:316–317. PMID: 11697704.
5. Lowe FC, Fishman EK, Oesterling JE. Computerized tomography in diagnosis of bladder rupture. Urology. 1989; 33:341–343. PMID: 2929071.

6. Albino G, Bilardi F, Gattulli D, Maggi P, Corvasce A, Marucco EC. Spontaneous rupture of urinary bladder: a case report and review. Arch Ital Urol Androl. 2012; 84:224–226. PMID: 23427749.
7. Lee MH, Jung JY, Baek DH, et al. A case of spontaneous-bladder rupture after a bout of heavy drinking. Korean J Med. 2009; 76:370–373.
8. Park JW. A case of peritonitis induced by urinary ascites due to spontaneous intraperitoneal bladder rupture. J Korean Geriatr Soc. 2011; 15:230–233.

9. Dubey IB, Mohanty D, Jain BK. Diverse presentation of spontaneous rupture of urinary bladder: review of two cases and literature. Am J Emerg Med. 2012; 30:832.e1–832.e3. PMID: 21570232.

10. Fujikawa K, Miyamoto T, Ihara Y, Matsui Y, Takeuchi H. High incidence of severe urologic complications following radiotherapy for cervical cancer in Japanese women. Gynecol Oncol. 2001; 80:21–23. PMID: 11136564.

11. Elliott SP, Bahaa SM. Long-term urinary adverse effects of pelvic radiotherapy. World J Urol. 2011; 29:35–41. PMID: 20959990.

12. Lynn SJ, Mark SD, Searle M. Idiopathic spontaneous bladder rupture in an intoxicated patient. Clin Nephrol. 2003; 60:430–432. PMID: 14690262.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download