Abstract
We describe a patient with severe hypernatremia and uremia caused by paranoid adipsia who was treated successfully with hydration and hemodialysis. A previously healthy 40-year-old woman developed the paranoid idea that her water was poisoned, so she refused to drink any water. On admission, her blood urea nitrogen was 208mg/dL, creatinine 4.90mg/dL, serum osmolality 452mOsm/L, serum sodium 172mEq/L, urine specific gravity ≥1.030, urine osmolality 698mOsm/L, and urine sodium/potassium/chloride 34/85.6/8mEq/L. We diagnosed her with uremic encephalopathy and started intravenous dextrose, but the sodium correction was incomplete. She underwent two sessions of hemodialysis to treat the uremic encephalopathy and hypernatremia, and recovered fully without neurological sequelae. Although the standard treatment for severe hypernatremia is hydration, hemodialysis can be an additional treatment in cases of combined uremic encephalopathy.
Go to : 
Hypernatremia is usually seen in elderly patients with cerebral lesions who cannot sense a water deficit or in distressed people1). Psychiatric patients can also lack the perception of water deficiency and develop hypernatremia and uremia2,3). However, there are no clinical reports on a Korean with severe hypernatremia and uremia caused by hydrophobia related to paranoid psychosis and treated with hemodialysis.
Prerenal acute kidney injury (AKI) is commonly seen with hypernatremia because of the severe water deficit, and both require large volume fluid replacement. In some cases of prerenal AKI with severe hypernatremia, the blood urea nitrogen (BUN) increases over 100mg/dL, which can cause uremic complications, such as encephalopathy, bleeding, and uremic effusion. Clinically, uremic encephalopathy presents as altered consciousness or personality caused by markedly elevated uremic toxins in the blood and can cause organic brain damage if left untreated4). Hypernatremia can be controlled via adequate intravenous water treatment and seldom requires hemodialysis therapy, unless it is combined with uremic syndrome. However, it has not been established whether hypernatremia with severe uremia and uremic encephalopathy should be treated with hydration alone, or hydration with hemodialysis.
We report a young woman with psychotic paranoid adipsia who developed severe hypernatremia (172mEq/L) and uremia (208mEq/L) with uremic encephalopathy. She was treated successfully with hydration and hemodialysis.
Go to : 
This previously healthy 40-year-old female was transported to the emergency room by her neighbors, who heard her moaning in her house. She lived alone, and 1 month prior to her admission, she developed the paranoid idea that her water was poisoned, and did not drink any water or beverages since then.
Her blood pressure was 100/60 mmHg, pulse rate 106/min, respiration rate 16/min, and body temperature 36.5℃. She looked chronically ill, and her skin and mucosa were extremely dehydrated. There was no evidence of trauma. A chest examination revealed a regular heart beat and clear breathing sounds. The abdomen was soft and flat with no palpable mass.
She was light, drowsy and disorientated. Her pupils were intact and reactive. The Glasgow Coma Scale was 11. No cranial nerve problem or peripheral nerve dysfunction was found.
White blood cell count 21,900/mm3 (4000-10,000/mm3), hemoglobin 11.2 g/dL(men 13-17 g/dL: women 12-16 g/dL), hematocrit 51%(men: 42-50%: women 36-44%), and platelets 207,000/mm3 (150,000-400,000/mm3). Her coagulation profile showed an international normalized ratio of 1.71 (1.2 below) and activated partial thromboplastin time of 177.4 sec (24-33 sec). Laboratory chemistry showed blood urea nitrogen 208mg/dL (8.0-20 mg/dL), creatinine 4.90mg/dL(0.6-1.2mg/dL), serum osmolality 452mOsm/L(289-302mOsm/L), protein 7.5 g/dL (6.5-8.2mg/dL), albumin 4.5 g/dL(3.5-5.1 g/dL), ionized calcium 4.6mg/dL (4.2-5.4mg/dL), magnesium 4.5mg/dL (1.9-2.5 mg/dL), serum sodium 172mEq/L(135-145mEq/L), potassium 4.4mEq/L(3.5-5.5mEq/L), chloride 127mEq/L(98-110 mEq/L), total CO2 21mEq/L (24-31mEq/L), aspiratetransaminase 22 IU/L (0-40 IU/L), alanine aminotransferase 16 IU/L (0-40 IU/L), total bilirubin 1.1mg/dL(0.2-1.1 mg/dL), myoglobin 1,949 ng/mL (28-72 ng/mL), creatine phsphokanase 389 IU/L (190 below IU/L), anti-diuretic hormone 8.95 pg/mL(0.0-6.7 pg/mL), adrenocorticotropic hormone (ACTH) 111 pg/mL(10-60 pg/mL), and cortisol 71 g/mL (morning 9.4-26.1/evening 1.8-12.7 g/mL). Breathing room air, the arterial blood gas analysis revealed pH 7.422, PaCO2 35.4mmHg, PaO2 106mmHg, and bicarbonate 22.6mEq/L. Urinalysis showed specific gravity was >1.030, urine pH 5.0, urine osmolality 698mOsm/L (300-900mOsm/L), and urine sodium/potassium/chloride34/85.6/8mEq/L.
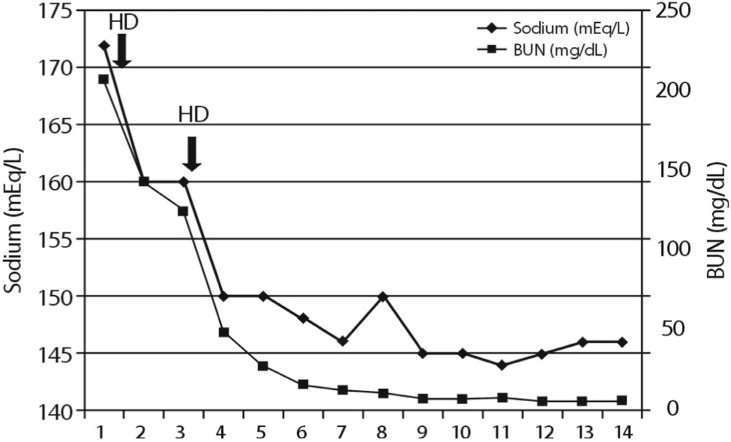
She was diagnosed with uremic encephalopathy due to severe prerenal acute renal failure. Her estimated water deficit was 5.94 L. We started intravenous dextrose for 4h, but the changein serum sodium was minimal (171mEq/L). We therefore started hemodialysis to treat the uremic encephalopathy. The dialysate sodium level was 150mEq/L. After dialysis, the serum sodium decreased to 160mEq/L, potassium was 4.2mEq/L, chloride 124 mEq/L, and total CO2 23mEq/L. After a second dialysis treatment, the sodium was 150mEq/L and she became alert without neurological sequelae. We continued an intravenous dextrose fluid infusion with oral hydration, and the sodium level normalized on day 3 of hospitalization (Fig. 1). After discharge, her sodium and chemistry profile remained normal.
Go to : 
This is the first report of hypernatremia and uremia caused by paranoid hydrophobia in Korea. Paranoid hydrophobia can create a water deficit, but is not known to create severe dehydration or uremic pre-renal acute kidney injury. Patients with a psychiatric illness can develop dehydration-induced hypernatremia. Farleyet al. reported a boy with severe water-deficit-induced hypernatremia (181mEq/L) and shock that developed during the treatment of schizophrenia; he had no sense of thirst, was hostile and withdrawn, and had neither drunk any water nor eaten for 6 days. This case showed that adipsic hypernatremia can occur even in a young healthy patient2). Decreased water intake can easily cause hypernatremia in elderly patients. Psychotic depression in such patients can also result in adipsia-induced hypernatremia5). The sodium levels in three patients who had hypovolemic hypotension were 157-164mEq/L. Hypernatremia developed in a young man who suffered psychotic depression and psychotic adipsia3). He had no sense of thirst, and had neither eaten nor drunk water. In comparison, our case was unusual because the patient felt thirsty, but had not drunk water due to a paranoid delusion that all liquids contained poison.
The standard treatment for severe hypernatremia is hydration. Isotonic saline is recommended for cases of volume depletion, while a 5% dextrose water solution is the treatment of choice for euvolemic hypernatremia1). Even in extremely severe hypernatremia >200mEq/L, rapid infusion of fluid can improve the patient's condition without neurological sequelae6). It should be emphasized that rapid correction of hypernatremia can cause cerebral edema via rapid water shifting into the brain, whereas central pontine myelinolysis can be developed by rapid correction of serum sodium. It is also important that additional water be added as the amount of urinary and insensible water is lost during the correction of hypernatremia.
It is not known whether hemodialysis can help a patient with severe hypernatremia. Hypernatremic patients with acute kidney failure and metabolic acidosis7) or rhabdomyolysis8) can be treated with continuous renal replacement therapy (CRRT). Park et al. reported the usefulness of CRRT in a patient with congestive heart failureand severe hypernatremia9). Although our patient did not show severe metabolic acidosis or rhabdomyolysis, only uremic encephalopathy, we tried to resolve the hypernatremia and uremic encephalopathy, as she was young. We worried that acute hemodialysis might rapidly reduce her serum sodium level and could create cerebral edema, so we set the dialysate sodium at the maximum concentration. It is not clear whether rapid correction of hypernatremia via hemodialysis can lead to neurologic complications. Yang et al. reported successful treatment of acute severe hypernatremia and uremia with hemodialysis therapy without any neurological complications10).
In conclusion, we experienced a case of paranoid adipsia that led to severe hypernatremia and uremia, which was treated with hemodialysis therapy without neurological complications.
Go to : 
References
2. Farley PC, Lau KY, Suba S. Severe hypernatremia in a patient with psychiatric illness. Arch Intern Med. 1986; 146:1214–1215. PMID: 3718109.

3. Phillips MG, Gabow PA. Psychogenic adipsia in a patient with psychotic depression. Am J Kidney Dis. 1990; 15:592–594. PMID: 2368698.

4. Brouns R, De Deyn PP. Neurological complications in renal failure: a review. Clin Neurol Neurosurg. 2004; 107:1–16. PMID: 15567546.

5. Jana DK, Romano-Jana L. Hypernatremic psychosis in the elderly: case reports. J Am Geriatr Soc. 1973; 21:473–477. PMID: 4729012.

6. Park YJ, Kim YC, Kim MO, Ruy JH, Han SW, Kim HJ. Successful treatment in the patient with serum sodium level greater than 200mEq/L. J Korean Med Sci. 2000; 15:701–703. PMID: 11194198.

7. Yang YF, Wu VC, Huang CC. Successful management of extreme hypernatraemia by haemofiltration in a patient with severe metabolic acidosis and renal failure. Nephrol Dial Transplant. 2005; 20:2013–2014. PMID: 15985507.

8. Yang TY, Chang JW, Tseng MH, Wang HH, Niu DM, Yang LY. Extreme hypernatremia combined with rhabdomyolysis and acute renal failure. J Chin Med Assoc. 2009; 72:555–558. PMID: 19837653.

9. Park HS, Hong YA, Kim HG, Choi SR, Sun IO, Chung BH, Park CW, Yang CW, Kim YS, Choi BS. Usefulness of continuous renal replacement therapy for correcting hypernatremia in a patient with severe congestive heart failure. Hemodial Int. 2012; 16:559–563. PMID: 22515501.

10. Yang CW, Kim YS, Park IS, Chang YS, Yoon YS, Bang BK. Treatment of severe acute hypernatremia and renal failure by hemodialysis. Nephron. 1995; 70:372–373. PMID: 7477631.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download