Abstract
We report a rare case of the concurrent manifestation of central diabetes insipidus (CDI) and type 2 diabetes mellitus (DM). A 56 year-old man was diagnosed as a type 2 DM on the basis of hyperglycemia with polyuria and polydipsia at a local clinic two months ago and started an oral hypoglycemic medication, but resulted in no symptomatic improvement at all. Upon admission to the university hospital, the patient's initial fasting blood sugar level was 140 mg/dL, and he showed polydipsic and polyuric conditions more than 8 L urine/day. Despite the hyperglycemia controlled with metformin and diet, his symptoms persisted. Further investigations including water deprivation test confirmed the coexisting CDI of unknown origin, and the patient's symptoms including an intense thirst were markedly improved by desmopressin nasal spray (10 µg/day). The possibility of a common origin of CDI and type 2 DM is raised in a review of the few relevant adult cases in the literature.
Syndrome of inappropriate secretion of antidiuretic hormone (SIADH), also known as the syndrome of inappropriate antidiuresis (SIAD), is one of the most common causes of hyponatremia1). It is associated with increased morbidity and mortality2). SIADH is a well-known cause of isovolemic, hypotonic hyponatremia. Impaired water excretion in the absence of renal insufficiency, glucocorticoid deficiency, hypothyroidism and decreased effective arterial blood volume are the hallmarks of this syndrome. Although a growing number of drugs have been reported to produce SIADH, most published reports concern vasopressin and its analogues such as thiazide and thiazide-like diuretics, chlorpropamide, carbamazepine, antipsychotics, antidepressants and nonsteroidal anti-inflammatory drugs. Old age seems a risk factor of SIADH following the use of many of these drugs. A combined use of these drugs, excessive fluid intake, and other underlying conditions which limit free water excretion will increase the risk3).
Sodium valproic acid (VPA), known as a carboxylic acid, is being used for an anti-epileptic in idiopathic and symptomatic generalized epilepsies and for some symptomatic focal epilepsies as well as trigeminal neuralgia, migraine and bipolar disorders4). Its mechanism is unknown; however it is probably associated with the metabolism of the GABA neurotransmitter. The toxic effect it provokes can be a dose-dependent or idiosyncratic. There are several VPA-related idiosyncrasies; the most noteworthy are alopecia, bone marrow aplasia, immune-mediated hepatotoxicity and pancreatitis5).
Here we describe a patient with hyponatremia caused during the treatment with the antiepileptic drug, i.e., sodium valproic acid (VPA). The clinical course indicated that VPA contributed to an SIADH6). To our knowledge, this is a rare case of example in the medical literature in English which shows an association between VPA and SIADH.
A 55-year-old man was admitted to hospital with seizure and confusion. He had suffered from generalized tonic clonic epilepsy that occurred after a craniectomy due to right epidural hematoma. The patient was treated with sodium valproate in a dose of 900 mg/day for 9 months. He had been removed a brain tumor 4 years before and he had craniectomy for an epidural hematoma 10 months ago. He was admitted to our hospital with a reported seizure, dizziness, nausea and vomiting for the day.
His vital signs, physical and neurological examination on arrival were within normal limits except drowsy consciousness. He appeared euvolemic without evidence of congestion or dehydration. An electroencephalography showed slow background activity with no evidence of epileptiform discharges. Mild bilateral cortical atrophy was observed on magnetic resonance imaging of the brain. Significant laboratory findings were: sodium of 111 (135-145) mmol/l , potassium of 2.6(3.5-5.0) mmol/l, chloride 66 (95-110) mmol/l and serum osmolarity of 245 (280-300) mosm/kg. Urine sodium and urine osmolarity were 58 mmol/l and 751 (50-1,200) mosm/kg, respectively.
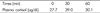
Ante meridiem cortisol level, thyroid stimulating hormone, and free thyroxine level were within normal limits. The results of her rapid ACTH stimulation tests were also within normal ranges (Table 1). Valproic acid level was revealed to be within therapeutic range (62.76 µg/ml; an optimum therapeutic range 50 to 100 µg/ml). After she was discharged, she did not restrict her water consumption.
The diagnosis of SIADH was made based on hyponatremia, and low serum and high urine osmolality. No other causes of hyponatremia, including diuretic therapy, tumors and respiratory system disease, were present. The sodium valproate treatment was discontinued, and hypertonic saline was infused because of his symptomatic and profound hyponatremia. His serum sodium concentration increased to 131 mmol/l over 48 hours with the use of hypertonic saline. The symptoms resolved immediately after the correction of hyponatremia. During the next 48 hours, normal saline infusion was given, and serum sodium level was restored to 134 mmol/l. Serum sodium concentration was maintained at 134-136 mmol/l after stopping saline infusion and VPA (Fig. 1). Lamotrigine was prescribed and he was subsequently discharged. The follow-up sodium levels for 3-weeks and 6-months after discharge were normal.
This patient developed confusion and seizure secondary to hyponatremia most probably induced by VPA. The patient presented with hyponatremia, hypoosmolality, impaired excretion of water, which are all features of SIADH7) and of generalized tonic clonic convulsions. We consider these seizures to be caused by hyponatremia due to SIADH; because other symptoms differed from those of the initial convulsive episode and serum VPA level which was useful to assess the patient compliance was within the target therapeutic range. Other causes of hyponatremia such as volume depletion, hypothyroidism, renal or adrenal insufficiency and diuretic abuse, and vomiting were excluded. The correction of the patient's hyponatremia, combined with the discontinuation of sodium valproate, resulted in the resolution of his hyponatremia. This is the first report in Korea on such an adverse reaction to this medication.
Use of VPA could lead to gastrointestinal discomfort, weight gain, hair loss, tremor and sedation, but these side effects seems rather uncommon, mild, and transient during VPA monotherapy8). Potentially hazardous reactions such as hepatitis and pancreatitis have occurred in a few patients on VPA, generally in multidrug therapy8). Others of the side effects are caused by dose related ones. They infrequently led to withdrawal of VPA8). In our MEDLINE search (Consider including this in the introduction before noting side effects are quoted), we could find only a few patients who reported hyponatremia at different times after sodium valproate use9-13).
The mechanism by which valproic acid could cause hyponatremia or SIADH has not been fully elucidated. Most cases of drug-induced hyponatremia involve the elderly, and could be related to an altered antidiuretic hormone (ADH) regulation or action of ADH on kidneys12). We speculate that dopaminergic, serotonergic and noradrenergic systems may play a role in SIADH due to sodium valproate14). Another hypothesis is that valproic acid has a direct effect on tubular cell function, because a few cases of tubular dysfunction in association with valproic acid with a positive dechallenge have been described5). Valproic aciduse could lead to reduced sensitivity of the hypothalamic osmoreceptors13). It could be a doseor concentration-related adverse effect13). Thus, we consider this episode of SIADH to be due to a combination of factors including serotonergic stimulation of ADH, reduced sensitivity of the hypothalamic osmoreceptors, and reduced renal ability to conserve salt and water.
Hyponatremia accompanied by CNS disorders has shown to increase delayed cerebral ischemia and mortality rates15). Therefore, we suggest that patients who have high risk of hyponatremia are recommended to measure the baseline electrolyte levels before starting therapy with sodium valproate16), and to monitor for electrolyte levels throughout the full course of treatment.
Figures and Tables
References
1. Baylis PH. The syndrome of inappropriate antidiuretic hormone secretion. Int J Biochem Cell Biol. 2003. 35:1495–1499.

2. Hoorn EJ, Lindemans J, Zietse R. Development of severe hyponatraemia in hospitalized patients: treatment-related risk factors and inadequate management. Nephrol Dial Transplant. 2006. 21:70–76.

3. Chan TY. Drug-induced syndrome of inappropriate antidiuretic hormone secretion. Causes, diagnosis and management. Drugs Aging. 1997. 11:27–44.
4. Genton P, Gelisse P. Levy RH, Mattson RH, Meldrum BS, Perucca E, editors. Valproic acid. Adverse effects. Antiepileptic drugs. 2002. 5th Ed. Philadelphia: Lippincott William & Wilkins;838–851.
5. Zaccara G, Franciotta D, Perucca E. Idiosyncratic adverse reactions to antiepileptic drugs. Epilepsia. 2007. 48:1223–1244.

6. Branten AJ, Wetzels JF, Weber AM, Koene RA. Hyponatremia due to sodium valproate. Ann Neurol. 1998. 43:265–267.

7. Bartter FC, Schwartz WB. The syndrome of inappropriate secretion of antidiuretic hormone. Am J Med. 1967. 42:790–806.

8. Keranen T, Sivenius J. Side effects of carbamazepine, valproate and clonazepam during long-term treatment of epilepsy. Acta Neurol Scand Suppl. 1983. 97:69–80.
10. Miyaoka T, et al. Contribution of sodium valproate to the syndrome of inappropriate secretion of antidiuretic hormone. Int Clin Psychopharmacol. 2001. 16:59–61.

11. Herment N, et al. Hyponatremia induced by sodium valproate. A case report. Therapie. 2006. 61:544–547.
12. Bavbek N, et al. Hyponatremia associated with sodium valproate in a 22-year-old male. Nephrol Dial Transplant. 2008. 23:410.
13. Beers E, et al. Syndrome of inappropriate antidiuretic hormone secretion (SIADH) or hyponatraemia associated with valproic Acid: four case reports from the Netherlands and a case/non-case analysis of vigibase. Drug Saf. 2010. 33:47–55.

14. Corda C, et al. Hyponatremia under sodium valproate: search a drug interaction. Therapie. 1991. 46:169.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download