Abstract
Background
Sacral slanting is a frequent unique phenomenon in patients with adolescent idiopathic scoliosis (AIS) and may be important for selecting the distal fusion level. However, the reason of the phenomenon remains unknown. The purpose of this study was to determine the association between sacral slanting and adjacent structures in patients with AIS.
Methods
A total of 303 AIS patients who underwent both whole spine standing anteroposterior (AP) and whole leg standing AP radiography were included. The degree of sacral slanting, pelvic obliquity, lumbar curve angles (L1-L4), and L4 tilt were assessed on whole spine standing AP radiographs. Whole leg standing AP radiographs were used to assess the degree of leg length discrepancy (LLD). Demographic data and radiological parameters were analyzed descriptively. Pearson correlation analysis and partial correlation analysis of the parameters were performed. A p-value of less than 0.05 was considered statistically significant.
Results
The proportion of patients with ≥ 5° of sacral slanting among those with < 3° of pelvic obliquity was 8.9% (27/303). Thirty-two patients (10.6%, 32/303) showed more than 10 mm of LLD. Sacral slanting was positively correlated with pelvic obliquity and lumbar curve (r = 0.445 and r = 0.325, respectively). Pelvic obliquity was also correlated with LLD and L4 tilt (r = 0.123 and r = 0.311, respectively). However, partial correlation analysis showed that LLD was not directly correlated with sacral slanting (r = −0.034).
Sacral slanting is a unique and frequent finding in patients with adolescent idiopathic scoliosis (AIS).1) It is defined by slanting of the upper surface of the sacrum, which can be measured on standing anteroposterior (AP) radiographs. The sacrum is frequently slanted to the left side, which could have a protective effect by preventing the aggravation of distal lumbar curve.1) Therefore, understanding the mechanism underlying sacral slanting is important. However, the cause of sacral slanting has not been studied previously.
Anatomically, the sacrum is connected to the fifth lumbar vertebra and pelvis by the disc and sacroiliac joint, respectively. Therefore, it is reasonable to assume that tilting of the lower lumbar vertebrae or pelvic obliquity may be associated with sacral slanting. In addition, leg length discrepancy (LLD) may be related to sacral slanting because pelvic obliquity is related to LLD.23) The degree of LLD can be measured on whole leg standing AP radiographs. We thought it would be possible to reveal the cause of sacral slanting by investigating the relationship among the abovementioned factors. Presumed causes of sacral slanting were (1) compensation for large lumbar curves, which could be accompanied by pelvic obliquity; (2) LLD; or (3) congenital anomaly of the sacrum, which could be suspected if pelvic obliquity or LLD did not exist. The purpose of this study was (1) to assess the association between sacral slanting and adjacent structures in patients with AIS and (2) to determine the plausible cause of sacral slanting.
A total of 303 AIS patients who underwent corrective surgery and agreed to participate in this study conducted at Asan Medical Center between January 2012 and December 2014 were included in this study. All surgeries were performed by a single surgeon at the center. Patients with a specific cause of scoliosis, such as neuromuscular disease, syringomyelia, congenital heart disease, and syndrome-related scoliosis, were excluded. Demographic and radiological data were collected though a review of the electronic medical records and the picture archiving communication system of Asan Medical Center. Demographic data included patient age, sex, height, weight, and body mass index (BMI). Curve types were classified by one rater who had experience with spine surgery for 5 years by using the King and Lenke methods.45) Whole spine AP and lateral radiographs were obtained with the patient in an upright standing posture for both views and with arms folded forward for lateral views pre- and postoperatively. Preoperatively, whole leg standing AP radiographs were additionally obtained with the patella facing forward to determine LLD. To minimize radiation exposure, breasts were protected when whole leg radiographs were taken. This study was approved by the Institutional Review Board (IRB No. S2016-0802-0001) of Asan Medical Center, which waived the requirement for informed consent due to the retrospective nature of the analysis.
The degree of sacral slanting was defined as the angle between a horizontal line and the upper endplate of the sacrum. The degree of pelvic obliquity was defined as the angle between a line connecting the top of both iliac crests and the horizontal line. Lumbar curve angle was measured by the Cobb's angle between the upper endplate of L1 and the lower endplate of L4. L4 tilt was measured as the angle between the horizontal line and the upper endplate of L4. The abovementioned four radiological parameters were assessed on whole spine standing AP radiographs. All values for the parameters were preceded by a positive sign if the apex of the curve was towards the left or if left inclination was shown. The degree of LLD was defined as the difference between the right and left lower limb lengths measured by the distance between the top of the femoral head and the ankle center on whole leg AP radiographs. It was denoted with a positive sign if the right leg was longer than the left leg. The methods of measurement are illustrated in Fig. 1.
Radiological parameters were measured by two raters who had experience with spine surgery for 5 years and 1 year, respectively. Each parameter was measured twice with a 1-month interval.
Demographic data, curve type, and each radiological parameter were analyzed descriptively. The frequency of sacral slanting and pelvic obliquity was assessed by different angle criteria. Interobserver and intraobserver agreement was assessed by calculating intraclass correlation coefficients (ICCs), with ICCs of 0.8–1.0, 0.6–0.79, and < 0.6 defined as good, moderate, and poor, respectively.
Pearson correlation analysis was used to determine correlations between radiological parameters. Partial correlation analysis was also conducted to exclude confounding variables. Correlation coefficient (r) was interpreted as follows: > 0.7, strong positive; 0.3–0.7, moderate positive; 0.1–0.3, weak positive; < 0.1, no correlation. All statistical analyses were performed using the IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA), with a p-value less than 0.05 considered to indicate statistical significance.
This study included 47 male and 256 female patients, with a mean age of 15.37 ± 3.02 years. Patient demographic data and curve types are summarized in Table 1 and Fig. 2. King type II was the most common curve type (32.7%), followed by type I (19.1%) in this population. Frequently observed types by the Lenke classification included 1A-(10.6%), 3CN (10.6%), and 5CN (10.2%).
For all radiological parameters, the interobserver and intraobserver agreement was good. The interobserver and intraobserver reliability of each radiological parameter is summarized in Table 2.
The degree of sacral slanting was 1.86° ± 3.06° (range, −10° to 14°). The degree of pelvic obliquity was 1.10° ± 2.28° (range, −6° to 8°). The frequency of ≥ 3° of sacral slanting and pelvic obliquity were 39.6% (sum of 36.3% with ≥ 3° of sacral slanting and 3.3% with ≤ −3° of sacral slanting) and 31.4% (sum of 25.4% with ≥ 3° of pelvic obliquity and 5.9% with ≤ −3° of pelvic obliquity), respectively. The frequency of ≥ 3° of difference between sacral slanting and pelvic obliquity was 25.1%. The distribution of patients by different angle criteria is summarized in Table 3. The proportion of patients with ≥ 5° of sacral slanting among those with less than 3° of pelvic obliquity was 8.9% (27/303).
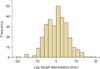
The degree of lumbar curve was 24.48° ± 11.54° (range, −47° to 52°) and that of L4 tilt was 9.23° ± 11.85° (range, −27° to 41°). The degree of LLD was 0.02 ± 5.63 mm (range, −20 to 18 mm). The distribution of patients according to LLD is shown in Fig. 3. The percentages of patients with LLD of more than 10 mm, 8 mm, and 6 mm were 10.6% (32 patients), 16.8% (51 patients), and 27.8% (88 patients), respectively.
Pearson correlation analysis showed positive correlations among all radiological parameters (Table 4). However, partial correlation analysis showed no correlation between some factors (Table 5). The results showed that sacral slanting was correlated with pelvic obliquity (r = 0.445) and lumbar curve (r = 0.325). In addition, pelvic obliquity was also correlated with LLD (r = 0.123) and L4 tilt (r = 0.311). There was a positive correlation found between lumbar curve and L4 tilt (r = 0.223). However, sacral slanting was not directly correlated with LLD (r = −0.034).
In 32 patients with > 10 mm of LLD, the partial correlation analysis showed no correlation between LLD and pelvic obliquity (r = 0.135, p = 0.511), and between pelvic obliquity and lumbar curve (r = −0.112, p = 0.585). No association was found between LLD and sacral slanting (r = −0.103, p = 0.616)
Sacral slanting is defined as a slanted angle of the upper sacrum on whole spine standing AP radiographs. The frequency of sacral slanting was previously reported to be 19.5%, 29.6%, and 40.6% by the angle criteria of 5°, 4°, and 3°, respectively.1) The values were similar in our present study with 20.2%, 27.1%, and 39.6% using the same criteria. Sacral slanting has been proposed to be important for selection of the distal fusion level.1) However, the mechanism underlying this association has not been evaluated because the mechanism of sacral slanting remains unknown.
Anatomically, the sacrum is connected to the L5 vertebra and the pelvis by the L5-S1 disc and sacroiliac joint, respectively. The pelvis is also connected to the legs by the hip joint. Therefore, possible correlation factors that can affect sacral slanting include the lumbar curve, pelvic obliquity, and LLD. Evaluation of the L4 tilt was added in the radiological assessment because it can represent a large distal lumbar curve.
Positive correlations were seen for all parameters in the Pearson correlation analysis. However, partial correlation analysis, aimed at eliminating confounding factors and revealing true positive correlations, showed that L4 tilt was correlated to pelvic obliquity, which was also correlated to sacral slanting. This can mean that sacral slanting is an indirect compensation mechanism for large distal lumbar curves caused by pelvic obliquity. In addition, the direct positive correlation between sacral slanting and lumbar curve indicates sacral slanting can be a direct compensation mechanism for large lumbar curve. In contrast, it could be inferred from some cases that sacral slanting may cause lumbar curve: 8.9% of patients showed ≥ 5° of sacral slanting with < 3° of pelvic obliquity. Furthermore, the frequencies of showing more than 3°, 4°, and 5° of difference between sacral slanting and pelvic obliquity were 19.5%, 13.2%, and 8.6%, respectively. This may be attributable to congenital anomalies such as asymmetrical vertical growth of the sacrum. However, we could not determine the cause and effect relationship between sacral slanting and lumbar curve in the current correlation analysis.
LLD is another important factor for scoliosis and sacral slanting because it is likely related to pelvic obliquity.23) The proportion of patients with an LLD of more than 1 cm was 10.6% (32/303) in our study, which is in agreement with a previous study suggesting an LLD frequency of 3%–15% in the general population.6) It has been proposed that functional scoliosis may be caused by even mild degrees of LLD.67) Furthermore, a significant correlation has been found between different leg lengths and changes in pelvic position.8) However, asymmetry of the pelvis has been known to cause a type of LLD that is reversible and termed apparent LLD.9) This bidirectional relationship was supported by the positive correlation between LLD and pelvic obliquity found in our analysis (r = 0.123). However, sacral slanting did not directly correlate with LLD based on our partial correlation findings (r = −0.034). Our proposed mechanism is briefly illustrated in Fig. 4. The relationships between LLD and other radiological parameters were evaluated in further analysis involving 32 patients who showed more than 10 mm of LLD. Although the sample size was not sufficient for statistical analysis, LLD was not related with other radiological parameters. In addition, sacral slanting was not related with LLD in the subgroup analysis. Thus, we could not determine the effect of LLD on lumbar scoliosis in the current study.
There were a few limitations to our current study. First, our correlation analysis could not reveal the cause and effect relationship. Therefore, we could not determine whether sacral slanting itself could be the cause of scoliosis in the lumbar region. Further anatomic studies on the sacrum are needed to clarify this relationship. Second, our study population was limited to patients who underwent surgery. Therefore, the suggested causes of sacral slanting cannot be generalized to all AIS patients. Further studies targeting patients with mild scoliosis who do not require surgery are needed.
However, it is noteworthy that our current study reports several new findings and concepts. First, the concept and frequency of sacral slanting in patients with AIS were validated. Second, possible mechanisms of sacral slanting were assessed in correlation analysis despite some methodological limitations. Third, the frequency of LLD in patients with AIS has never been reported previously. Our present report could, therefore, be a cornerstone for future studies regarding LLD in patients with AIS.
In conclusion, sacral slanting can be thought as a compensatory mechanism for large lumbar curves accompanied by pelvic obliquity. In some cases, a congenitally slanted upper sacrum may cause scoliosis although further anatomic studies are needed to confirm these findings. In addition, LLD was not directly correlated with sacral slanting.
Figures and Tables
 | Fig. 1Measurements of radiological parameters. a: degree of sacral slanting, b: degree of pelvic obliquity, c: degree of L4 tilt, d: degree of lumbar curve. |
 | Fig. 4Illustration of the relationship between sacral slanting and other radiological parameters. Plausible cause and effect relationships are indicated with white arrows. LLD: leg length discrepancy. |
Table 1
Demographic Data and Curve Types in AIS Patients

Table 2
Reliability Test for Each Radiological Parameter

| Variable | Interobserver agreement | Intraobserver agreement |
|---|---|---|
| Sacral slanting | 0.893 | 0.917 |
| Pelvic obliquity | 0.978 | 0.963 |
| Lumbar curve | 0.913 | 0.962 |
| L4 tilt | 0.916 | 0.921 |
| Leg length discrepancy | 0.968 | 0.975 |
Table 3
Distribution of Sacral Slanting and Pelvic Obliquity
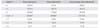
Table 4
Pearson Correlation Analysis among Various Radiological Parameters

Table 5
Partial Correlation Analysis among Various Radiological Parameters

References
1. Lee CS, Ha JK, Kim DG, et al. The clinical importance of sacral slanting in patients with adolescent idiopathic scoliosis undergoing surgery. Spine J. 2015; 15(5):834–840.

2. Needham R, Chockalingam N, Dunning D, Healy A, Ahmed EB, Ward A. The effect of leg length discrepancy on pelvis and spine kinematics during gait. Stud Health Technol Inform. 2012; 176:104–107.
3. Cummings G, Scholz JP, Barnes K. The effect of imposed leg length difference on pelvic bone symmetry. Spine (Phila Pa 1976). 1993; 18(3):368–373.

4. King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983; 65(9):1302–1313.

5. Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001; 83(8):1169–1181.
6. Raczkowski JW, Daniszewska B, Zolynski K. Functional scoliosis caused by leg length discrepancy. Arch Med Sci. 2010; 6(3):393–398.
7. Zabjek KF, Leroux MA, Coillard C, et al. Acute postural adaptations induced by a shoe lift in idiopathic scoliosis patients. Eur Spine J. 2001; 10(2):107–113.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download