This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Various deformities can occur in the forearm bones when the traumatically dislocated radial head is untreated for a long period. Without correction of all deformities, reduction of the dislocated radial head is difficult to maintain, and forearm and elbow motion will deteriorate after reduction. We evaluated radiographic parameters of forearms with traumatically dislocated radial heads (and of the normal sides) to understand the resulting deformities and the effectiveness of surgical treatment.
Methods
We analyzed pre- and postoperative anteroposterior and lateral radiographs of 22 forearms (22 patients) with traumatic radial head dislocation. We divided the forearm into three equal parts and measured various morphological parameters. All patients underwent surgical treatment and evaluation of radial head reduction and range of motion pre- and postoperatively.
Results
Before treatment, the middle of the ulna was significantly different from the unaffected side in both anteroposterior and lateral views. After surgery, the proximal ulna was significantly different from the unaffected side and the abnormal proximal radial neck angle persisted. The radial head was successfully reduced in 20 of 22 cases. Overall, the mean range of motion decreased after surgery, except for increased flexion-extension.
Conclusions
Complicated deformities developing during long-term remodeling after injury indicate that stable reduction is difficult to achieve with conventional one-bone osteotomy. Even after successful reduction, secondary deformity in the proximal ulna and/or remaining deformity in the proximal radius can hinder forearm rotation.
Keywords: Radial deformity, Ulnar deformity, Radiographic parameter
Chronic radial head dislocation in children, of both traumatic and congenital types, is a challenge for the physician. Treatment options range from nonsurgical treatment, ulnar osteotomy,
1234567) ulnar and radial osteotomy,
89) annular ligament reconstruction
1011121314) to ulnar osteotomy and annular ligament reconstruction.
9151617) However, the literature does not provide an optimal procedure for cases which have gone untreated for several years with various deformities. When the normal anatomy of the proximal radius and ulna is changed, stable reduction of the radial head cannot be obtained by a single osteotomy performed to correct anterior bowing of the ulna (caused by a previous Monteggia fracture). In the forearm where both the radius and ulna rotate on one axis, an uncorrected deformity in one bone may influence the other. Therefore, forearm rotation will deteriorate after surgery if all deformities in both bones are not corrected.
Although surgical treatment for traumatic dislocation primarily depends on radiographic findings, there have been no detailed studies on radiographic changes of the radius and ulna. In 22 patients whose traumatically dislocated radial heads were surgically reduced by traditional methods, we analyzed pre- and postoperative anteroposterior (AP) and lateral radiographs to shed light on the clinical efficacy of surgical treatment.
METHODS
We retrospectively reviewed radiographs of patients with traumatic radial head dislocation. Informed consent for participation in the study was obtained from all patients or parents. We evaluated 22 forearms (22 patients, nine females and 13 males) with traumatic anterior dislocation of the radial head. The mean age of patients at the time of dislocation was 8.3 years (range, 3 to 15 years); the mean duration of dislocation was 14.9 months (range, 1 to 96 months); and the mean age at the time of surgery was 9.6 years (range, 5.7 to 18 years). Each subject had two radiographs of the affected side before and after operation (a mean of 7.7 years [range, 3 to 13 years] after surgery). An AP radiograph taken with the elbow in full extension and the forearm in supination and a lateral radiograph taken with the elbow in 90° flexion and the forearm in neutral rotation were selected from the picture archiving and communication system.
Measurement of Radiographic Parameters
On AP and lateral radiographs, we divided the forearm into three equal parts (the proximal, middle, and distal thirds) and analyzed parameters we devised (described below) to evaluate deformities in each part (
Figs. 1 and
2). Two of the parameters, maximal radial bow (MRB) and location of MRB (LMRB), were only measured from the AP view (
Fig. 3) because of overlapping of the radius and the ulna in the lateral view. Parameters were measured using tools in the Marosis m-view 5.4 software (Marotech, Seoul, Korea).
Proximal third
Proximal radial tilt angle (PRTA) represents the angle between the rotational axis of the forearm (AA’, from the center of the radial head to the center of the distal ulna) and the axis of the radial neck (a). The axis of the radial neck is from the center of the radial head to the center of the radial neck which is just on the apex of the bicipital tuberosity.
Proximal ulnar tilt angle (PUTA) is the angle between the rotational axis of the forearm (AA’) and the axis of the proximal ulna (e). The axis of the proximal ulna is from the center of the ulna which is just below the coronoid process to the proximal third of the ulnar shaft.
Proximal radioulnar angle (PRUA) is the angle between the axis of the radial neck (a) and the axis of the proximal ulna (e).
Middle third
Middle radial tilt angle (MRTA) represents the angle between the rotational axis of the forearm (AA’) and the axis of the middle radius (c). The axis of the middle radial shaft is from the center of the junction of the proximal and middle radius to the center of the junction of the middle and distal radius.
Middle ulnar tilt angle (MUTA) represents the angle between the rotational axis of the forearm (AA’) and the axis of the middle ulna (f). The axis of the middle ulnar shaft is from the center of the proximal-middle ulna junction to the center of the middle-distal ulnar shaft junction.
MRB is the maximal distance (C to C’) from the ulnar side of the radius to the line connecting the bicipital tuberosity and the most ulnar aspect of the radius at the wrist (BB’).
LMRB is a ratio of the distance from the bicipital tuberosity to the point of MRB (B to MRB) to the distance from the bicipital tuberosity to the most ulnar aspect of the radius at the wrist (B to B’).
Distal third
Distal radial tilt angle (DRTA) represents the angle between the rotational axis of the forearm (AA’) and the axis of the distal radius (d). The axis of the distal radius is from the center of the junction of the middle and distal radius to the center of the distal radius.
Distal ulnar tilt angle (DUTA) represents the angle between the rotational axis of the forearm (AA’) and the axis of the distal ulna (g). The axis of the distal ulna is from the center of the junction of the middle and distal ulna to the center of the distal ulna.
Analysis of Deformities
We compared the nine parameters listed above between the affected and the unaffected sides, both before and after surgical treatment. The patients were divided into two groups according to the duration of dislocation. A cutoff value (4 months) was selected so that the number of patients in the two groups was similar. There were 10 patients with a duration of 4 months or less in one group and 12 patients with a duration of more than 4 months in the other group. We assessed differences between the groups.
Range of Motion of the Elbow and Forearm
Preoperative range of motion (ROM) of the elbow and forearm was obtained from the medical records, while postoperative ROM was measured at the last follow-up. ROM included flexion-extension, pronation, and supination measured with a hand-held goniometer using standard methods.
Surgical Treatment
Surgical treatment included various procedures.
18) Open reduction of the radial head, debridement of soft tissues between the radial head and capitellum, radial shortening when the radius was elongated, and annular ligament reconstruction using a pedicled central tendinous strip of the triceps were the main procedures on the radial side. Rotation of the proximal part of the osteotomized radius
19) and/or radial head arthroplasty were often performed when congruency between the radial head and the capitellum and/or stability of reduction were judged insufficient. Ulnar flexion osteotomy to correct anterior ulnar bowing was performed at the proximal site or at the location of maximal deformity in the diaphysis. Notchplasty in the proximal ulnar notch for the radial head (excision of osteophytes or hypertrophied bone) was performed when it improved stability of reduction of the radial head and/or forearm movement. Osteotomy sites in the radius and ulna (proximal or middle) were decided before the operation based on comparison of the AP and lateral radiographs of the unaffected and affected sides. Osteotomy sites chosen to correct deformity in the ulna were proximal in 12, middle in six, and distal in one. Combined radial osteotomy and/or shortening were performed in 10 cases (nine middle and one proximal). The amount of radial shortening was decided preoperatively by measuring the distance from the coronoid process to the displaced radial head in the radiograph, or during surgery by measuring the overlapping length of the osteotomized radius after radial head reduction. Selection of all procedures for each patient was decided by the senior author (HTK).
Statistical Analysis
Paired t-tests were used to compare parameters between the affected and the unaffected sides. The Mann-Whitney U-test was used to compare parameters between two groups of patients separated by the duration of dislocation. To compare values of ROM before and after surgery, we used a Wilcoxon signed-rank test. All variables are reported as means and standard deviations. Values of p < 0.05 were considered statistically significant. All data analyses were performed using IBM SPSS ver. 24.0 (IBM Corp., Armonk, NY, USA).
RESULTS
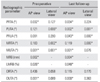
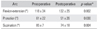
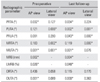
The values of all parameters measured on the unaffected side and on the affected side, both before surgery and at the last follow-up, are given in
Table 1. Statistical comparisons between parameter values on the unaffected and affected sides are given in
Table 2.
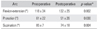
Table 3 gives a comparison of parameter values according to the duration of dislocation and,
Table 4 presents pre- and postoperative ROM measurements.
Before surgery, only one parameter (MUTA) was significantly different from the unaffected side in both AP and lateral views. PRUA and DRTA on the affected side were not significantly different from the unaffected side, while the other parameters were different in one view only (lateral or AP), not in both views.
At the last follow-up, two parameters concerning the proximal radius and ulna (PUTA and PRUA) were significantly different from the unaffected side in both AP and lateral views. MUTA, which had been significantly different between the affected and unaffected sides in both AP and lateral views before surgery, improved by the final follow-up, showing no side-to-side difference in the lateral view. For the other parameters, statistically significant changes were not noted in the comparison between affected and unaffected sides at the final follow-up.
Before surgery, only MRTA in AP view was significantly different between two groups of patients separated by duration of disease (
Table 3). Comparison of ROM values before and after surgery (
Table 4) showed decreased mean pronation and supination arcs after surgery, while the flexion-extension arc of the elbow was increased. After surgical reduction, two of the 22 patients (9%) had anterior subluxation of the radial head.
DISCUSSION
The nine parameters we measured on AP and lateral radiographs helped us to understand the changes of forearm bones following radial head dislocation. We found the MUTA to be significantly different in AP and lateral planes from the unaffected side before surgery, suggesting that the middle third of the ulna was mainly deformed (anteriorly in the lateral view and medially or laterally in the AP view). Similarly, Lincoln and Mubarak
20) described an abnormal middle ulna in which the ulnar bow sign in the lateral radiograph occurred near the midpoint, at a mean distance of 45% ± 2% from the proximal end. We found an anterior ulnar bow sign on the affected side in 12 of 22 patients, while five patients showed no bow sign in both arms, and five showed it on both sides. Thus, the bow sign was only helpful in 54% of our cases.
At the last follow-up, the two parameters measuring the proximal radial and ulnar angles (PUTA and PRUA) were significantly different from the unaffected side in both the AP and lateral planes (
Table 2). However, PUTA was different from the unaffected side only in the lateral view before surgery. PRUA was not different from the unaffected side preoperatively in either plane. We suspect this worsening is due to secondary deformation of the proximal radius and ulna because the radial head was reduced with a combined flexion osteotomy of the proximal ulna in some cases and annular ligament reconstruction. When the rotational axis of the two bones is not completely normalized after surgery, forearm rotation may be limited not only by remaining bony deformity. Excessive flexion osteotomy of the proximal ulna, aimed at placing the radial head in a correct position by tightening the interosseous membrane, can affect forearm rotation. An uncorrected proximal radial neck angle (PRTA) may also decrease forearm rotation.
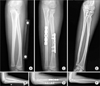
For a good result consisting of perfect reduction of the radial head and full ROM of the elbow and forearm, we believe that the surgeon must successfully correct all deformities (
Fig. 4). However, this is not feasible in reality due to overlooked, overcorrected, and/or newly formed deformities after surgery. Based on our results, the middle of the ulna should be corrected in both AP and lateral views, but not with too much of a flexion component in the proximal ulna. Also, the PRTA should be carefully evaluated before surgery because a deformity there might go unrecognized and become a factor limiting forearm rotation when combined with a too-tightly reconstructed annular ligament. Rarely, the radial head may be stably reduced by corrective osteotomy alone in the ulna (the area of greatest deformity), and additional procedures (such as an annular ligament, etc.) may simply increase the risk of limited motion.
We found notching in the radial neck due to constriction by the reconstructed annular ligament in 13 of 22 cases. Because the triceps tendon has different elasticity from the original annular ligament, its greater constriction pressure may lead to notching in the neck during forceful rotation of the forearm, especially when the radial head is not rotated on the normal axis of rotation but instead is translated due to deformity. Similarly, the shape of the radial head also changed in eight of our 22 cases to adapt to the newly established radiocapitellar joint after surgery. Obviously, uncorrected deformities and/or deformity occurring after corrective osteotomy can lead to secondary deformity in this area.
Comparison of ROM before surgery and at the last follow-up (
Table 3) showed decreased mean pronation and supination arcs, while the flexion-extension arc of the elbow was increased by reduction of the anteriorly dislocated radial head, which had been an obstacle for flexion and extension motion. The decreased arc of rotation again means that the deformities were not corrected sufficiently for the two bones to rotate normally. As Oka et al.
21) described, little attention has been paid to morphologic features of the proximal radioulnar joint in chronic radial head dislocation because of the difficulties in evaluating them on plain radiographs. Tatebe et al.
22) found a relation between PRTA and forearm rotation; the lesser the PRTA, the better the forearm rotation. Many studies indicate that the radial head becomes misshapen and overgrown within 3 years after injury and difficult to reduce.
1117212324) However, the literature provides no clear guidance on what treatments may be required depending on the duration of dislocation or on the severity of deformity.
When we separated our patients by duration of dislocation of 4 months, we did not find any significant difference in parameters measured except in the middle radius. This result is difficult to explain. We certainly expect that the longer the duration of dislocation, the more severe the deformities should be. Our patients showed a wide range of duration of dislocation ranging from 1 to 96 months, with more procedures being required in the longer period cases. Two patients who had subluxation after reduction of the radial head had been untreated for 3 months and 96 months, respectively; the former had technical problems in the surgery and refracture at the osteotomy site by repeated trauma. However, other patients who were untreated for several years were successfully reduced.
We question, however, whether it would be possible to correct all deformities in actual surgery even if we did know everything about the existing deformities before the operation. We performed only one or two osteotomies in each bone of the forearm, which might not be sufficient in cases which have gone untreated for several years, especially those associated with deformities in the radial head and neck. For these, we need other procedures, including osteotomy in the proximal radius with shortening, radial head arthroplasty, and ulnar notchplasty to avoid impingement from the radial head. We can also add simultaneous rotation of the proximal part of the radius after the osteotomy, with angular correction and/or shortening to achieve more stable and congruent reduction. When the surgeon corrects the abnormal proximal radius, he or she should be very cautious to prevent nonunion or radioulnar synostosis.
The ROM of the forearm depends on many aspects of the bones and soft tissues,
2526) but our radiographic study has not considered the latter. No matter how well the osteotomy sites are chosen, it is surely too much to expect that one or two osteotomies in the radius and/or ulna will suffice to restore normal anatomy and motion, especially in long-untreated cases including severe deformities. Our high success rate (91%) must be due to the various additional procedures
18) which we performed.
We successfully reduced the dislocated radial head in 91% of our traumatic cases with a combination of many different procedures, in which the osteotomy sites were selected on the AP and lateral radiographs of the forearm. However, our patients showed decreased pronation and supination arcs after surgery, suggesting that uncorrected or newly developed deformities still remained, which was confirmed by our detailed analysis of patient radiographs.
Figures and Tables
 | Fig. 1Anteroposterior radiograph of a forearm with an anteriorly dislocated radial head showing mid-axial lines in the proximal, middle, and distal radius and ulna used for measurement of the parameters. The line AA’ indicates the rotational axis of the forearm connecting from the center of the radial head to the center of the distal ulna. Proximal radial tilt angle, the angle between lines AA’ and a; proximal ulnar tilt angle, the angle between lines AA’ and e; proximal radioulnar angle, the angle between lines a and e; middle radial tilt angle, the angle between lines AA’ and c; middle ulnar tilt angle, the angle between lines AA’ and f; distal radial tilt angle, the angle between lines AA’ and d; and distal ulnar tilt angle, the angle between lines AA’ and g. a: the axis of the radial neck, b: the axis of the proximal radius, c: the axis of the middle radius, d: the axis of the distal radius, e: the axis of the proximal ulna, f: the axis of the middle ulna, g: the axis of the distal ulna.
|
 | Fig. 2Lateral radiograph showing mid-axial lines in the same segments of the radius and ulna as in the anteroposterior radiograph. The line AA’ indicates the rotational axis of the forearm. The white line from the proximal to the distal ulna is used for measurement of anterior ulnar bowing. a: the axis of the radial neck, b: the axis of the proximal radius, c: the axis of the middle radius, d: the axis of the distal radius, e: the axis of the proximal ulna, f: the axis of the middle ulna, g: the axis of the distal ulna.
|
 | Fig. 3Anteroposterior radiograph showing maximal radial bow and the location of maximal radial bow (calculated as a ratio of the distance from maximal radial bow to bicipital tuberosity to the distance from the bicipital tuberosity to the most ulnar aspect of the radius at the wrist). BB’: the distance from the bicipital tuberosity to the most ulnar aspect of the radius at the wrist, CC’: the maximal distance between the radius and ulna.
|
 | Fig. 4Anteroposterior (AP, A) and lateral (B) radiographs of a 7-year-old boy with anterior dislocation of the radial head. He slid down and underwent cast immobilization at another hospital 2 years ago (when he was 5 years old). In the lateral radiograph, the ulna was bowed anteriorly at the middle of the shaft with a positive ulna bow sign. The radial head was located anteriorly and beyond the anterior margin of the capitellum, suggesting overgrowth of the radius. He was treated with corrective osteotomy in the middle of the ulna (the area of maximal deformity). Also, a radial shortening osteotomy was performed to reduce the radial head. In addition, a notchplasty in the proximal ulna and annular ligament reconstruction were performed to maintain stable reduction because the radial head was translated out of the ulnar notch when the forearm was pronated. This meant the reduced radial head and ulna did not rotate on the same rotational axis of the forearm. AP (C) and lateral (D) radiographs taken 2 years after surgery (before metal removal) showing reduction of the radial head and correction of the ulnar deformity. The elbow extension-flexion and forearm supination arcs were similar to the normal side but the pronation arc was decreased (15° less than the normal side). Increased proximal radial tilt angle and proximal ulnar tilt angle in the AP radiograph compared to the preoperative values (and the normal side) and a radiological finding of mild radial neck-notching suggest that a secondary deformity occurred during the 2 years the patient had forceful range of motion exercises. Remaining or unrecognized bony deformities and/or tight ligament reconstruction might have contributed to these deformities and also affected the state of reduction of the radial head. Further close follow-up was required because the lateral radiograph showed slight anterior subluxation of the radial head which varied with the amount of supination-pronation. AP (E) and lateral (F) radiographs taken 10 years after surgery showing reduction of the radial head. Clinically, the patient had no limitation in daily activities and had a good result.
|
Table 1
Values of Parameters Measured on the Unaffected and Affected Sides

|
Radiographic parameter |
Unaffected side |
Affected side |
|
AP view |
Lateral view |
Preoperative |
Postoperative (last follow-up) |
|
AP view |
Lateral view |
AP view |
Lateral view |
|
PRTA (°) |
3.4 ± 1.8 |
4.4 ± 2.2 |
5.3 ± 3.6 |
5.4 ± 2.8 |
5.2 ± 3.5 |
5.0 ± 2.1 |
|
PUTA (°) |
9.1 ± 2.0 |
3.0 ± 1.7 |
8.1 ± 2.5 |
6.1 ± 3.9 |
5.9 ± 3.9 |
6.6 ± 3.9 |
|
PRUA (°) |
6.5 ± 4.7 |
5.7 ± 3.2 |
8.2 ± 4.9 |
6.3 ± 3.9 |
9.4 ± 6.5 |
12.8 ± 6.6 |
|
MRTA (°) |
8.0 ± 1.3 |
1.5 ± 1.0 |
7.3 ± 3.4 |
3.0 ± 2.2 |
7.3 ± 2.5 |
4.3 ± 2.7 |
|
MUTA (°) |
2.6 ± 1.3 |
5.8 ± 1.7 |
4.6 ± 2.7 |
8.3 ± 3.1 |
5.5 ± 2.8 |
4.9 ± 2.8 |
|
MRB (mm) |
11.8 ± 2.2 |
- |
9.0 ± 3.4 |
- |
9.3 ± 3.7 |
- |
|
LMRB (%) |
61.7 ± 4.3 |
- |
57.6 ± 6.0 |
- |
58.3 ± 6.2 |
- |
|
DRTA (°) |
2.1 ± 1.4 |
2.8 ± 1.4 |
2.2 ± 1.4 |
3.7 ± 2.1 |
3.4 ± 3.8 |
3.3 ± 2.4 |
|
DUTA (°) |
4.5 ± 1.9 |
7.2 ± 1.4 |
7.0 ± 2.6 |
8.3 ± 3.1 |
7.8 ± 2.9 |
6.8 ± 4.8 |

Table 2
Statistical Comparison of Radiographic Parameter Values between Unaffected and Affected Sides (Pre- and Postoperative)
|
Radiographic parameter |
Preoperative |
Last follow-up |
|
AP view |
Lateral view |
AP view |
Lateral view |
|
PRTA (°) |
0.032*
|
0.127 |
0.034*
|
0.224 |
|
PUTA (°) |
0.121 |
0.006*
|
0.002*
|
0.001*
|
|
PRUA (°) |
0.091 |
0.280 |
0.043*
|
0.000*
|
|
MRTA (°) |
0.183 |
0.002*
|
0.119 |
0.000*
|
|
MUTA (°) |
0.001*
|
0.001*
|
0.001*
|
0.076 |
|
MRB (mm) |
0.002*
|
- |
0.004*
|
- |
|
LMRB (%) |
0.026*
|
- |
0.048*
|
- |
|
DRTA (°) |
0.436 |
0.058 |
0.115 |
0.170 |
|
DUTA (°) |
0.001*
|
0.089 |
0.000*
|
0.363 |

Table 3
Comparison of Parameter Values According to the Duration
of Dislocation

|
Radiographic parameter |
≤ 4 Months (n = 10) |
> 4 Months (n = 12) |
p-value*
|
|
PRTA (°) |
AP |
5.2 ± 2.5 |
5.5 ± 4.7 |
0.330 |
|
Lateral |
5.9 ± 3.5 |
4.8 ± 1.9 |
0.342 |
|
PUTA (°) |
AP |
8.7 ± 2.6 |
7.4 ± 2.3 |
0.121 |
|
Lateral |
5.0 ± 3.3 |
7.4 ± 4.3 |
0.174 |
|
PRUA (°) |
AP |
9.3 ± 4.6 |
7.0 ± 5.1 |
0.153 |
|
Lateral |
6.2 ± 4.1 |
6.4 ± 4.0 |
0.500 |
|
MRTA (°) |
AP |
5.6 ± 3.8 |
9.1 ± 1.3 |
0.014 |
|
Lateral |
3.4 ± 2.3 |
2.6 ± 2.1 |
0.312 |
|
MUTA (°) |
AP |
4.0 ± 2.7 |
5.3 ± 2.6 |
0.200 |
|
Lateral |
8.2 ± 3.3 |
8.4 ± 3.1 |
0.435 |
|
MRB (mm) |
AP |
8.7 ± 3.6 |
9.2 ± 3.4 |
0.390 |
|
LMRB (%) |
AP |
58.4 ± 5.9 |
56.7 ± 6.3 |
0.256 |
|
DRTA (°) |
AP |
2.7 ± 1.5 |
1.7 ± 1.3 |
0.051 |
|
Lateral |
3.8 ± 2.7 |
3.5 ± 1.4 |
0.403 |
|
DUTA (°) |
AP |
7.1 ± 2.3 |
7.0 ± 3.1 |
0.484 |
|
Lateral |
7.7 ± 2.3 |
9.0 ± 3.9 |
0.118 |

Table 4
Comparison of Pre- and Postoperative Range of Motion on the Affected Side
|
Arc |
Preoperative |
Postoperative |
p-value*
|
|
Flexion-extension (°) |
118 ± 34 |
132 ± 25 |
0.002 |
|
Pronation (°) |
61 ± 22 |
51 ± 26 |
0.030 |
|
Supination (°) |
85 ± 7 |
74 ± 18 |
0.004 |

ACKNOWLEDGEMENTS
This work was supported by a 2-Year Research Grant of Pusan National University, Busan, Korea.
References
1. Fowles JV, Sliman N, Kassab MT. The Monteggia lesion in children: fracture of the ulna and dislocation of the radial head. J Bone Joint Surg Am. 1983; 65(9):1276–1282.

2. Letts M, Locht R, Wiens J. Monteggia fracture-dislocations in children. J Bone Joint Surg Br. 1985; 67(5):724–727.

3. Kalamchi A. Monteggia fracture-dislocation in children: late treatment in two cases. J Bone Joint Surg Am. 1986; 68(4):615–619.

4. Hirayama T, Takemitsu Y, Yagihara K, Mikita A. Operation for chronic dislocation of the radial head in children: reduction by osteotomy of the ulna. J Bone Joint Surg Br. 1987; 69(4):639–642.

5. Best TN. Management of old unreduced Monteggia fracture dislocations of the elbow in children. J Pediatr Orthop. 1994; 14(2):193–199.

6. Tajima T, Yoshizu T. Treatment of long-standing dislocation of the radial head in neglected Monteggia fractures. J Hand Surg Am. 1995; 20(3 Pt 2):S91–S94.

7. Inoue G, Shionoya K. Corrective ulnar osteotomy for malunited anterior Monteggia lesions in children: 12 patients followed for 1-12 years. Acta Orthop Scand. 1998; 69(1):73–76.

8. Freedman L, Luk K, Leong JC. Radial head reduction after a missed Monteggia fracture: brief report. J Bone Joint Surg Br. 1988; 70(5):846–847.

9. Stoll TM, Willis RB, Paterson DC. Treatment of the missed Monteggia fracture in the child. J Bone Joint Surg Br. 1992; 74(3):436–440.

10. Bell Tawse AJ. The treatment of malunited anterior Monteggia fractures in children. J Bone Joint Surg Br. 1965; 47(4):718–723.

11. Lloyd-Roberts GC, Bucknill TM. Anterior dislocation of the radial head in children: aetiology, natural history and management. J Bone Joint Surg Br. 1977; 59(4):402–407.

12. Hurst LC, Dubrow EN. Surgical treatment of symptomatic chronic radial head dislocation: a neglected Monteggia fracture. J Pediatr Orthop. 1983; 3(2):227–230.
13. Oner FC, Diepstraten AF. Treatment of chronic post-traumatic dislocation of the radial head in children. J Bone Joint Surg Br. 1993; 75(4):577–581.

14. Seel MJ, Peterson HA. Management of chronic posttraumatic radial head dislocation in children. J Pediatr Orthop. 1999; 19(3):306–312.

15. Rodgers WB, Waters PM, Hall JE. Chronic Monteggia lesions in children: complications and results of reconstruction. J Bone Joint Surg Am. 1996; 78(9):1322–1329.

16. Horii E, Nakamura R, Koh S, Inagaki H, Yajima H, Nakao E. Surgical treatment for chronic radial head dislocation. J Bone Joint Surg Am. 2002; 84(7):1183–1188.

17. Wang MN, Chang WN. Chronic posttraumatic anterior dislocation of the radial head in children: thirteen cases treated by open reduction, ulnar osteotomy, and annular ligament reconstruction through a Boyd incision. J Orthop Trauma. 2006; 20(1):1–5.

18. Kim HT, Conjares JN, Suh JT, Yoo CI. Chronic radial head dislocation in children. Part I: pathologic changes preventing stable reduction and surgical correction. J Pediatr Orthop. 2002; 22(5):583–590.

19. Futami T, Tsukamoto Y, Fujita T. Rotation osteotomy for dislocation of the radial head: 6 cases followed for 7 (3-10) years. Acta Orthop Scand. 1992; 63(4):455–456.
20. Lincoln TL, Mubarak SJ. “Isolated” traumatic radial-head dislocation. J Pediatr Orthop. 1994; 14(4):454–457.

21. Oka K, Murase T, Moritomo H, Sugamoto K, Yoshikawa H. Morphologic evaluation of chronic radial head dislocation: three-dimensional and quantitative analyses. Clin Orthop Relat Res. 2010; 468(9):2410–2418.

22. Tatebe M, Shinohara T, Okui N, Yamamoto M, Kurimoto S, Hirata H. Tilt of the radius from forearm rotational axis reliably predicts rotational improvement after corrective osteotomy for malunited forearm fractures. Nagoya J Med Sci. 2012; 74(1-2):167–171.
23. Wilkins KE. Changes in the management of monteggia fractures. J Pediatr Orthop. 2002; 22(4):548–554.

24. Hui JH, Sulaiman AR, Lee HC, Lam KS, Lee EH. Open reduction and annular ligament reconstruction with fascia of the forearm in chronic monteggia lesions in children. J Pediatr Orthop. 2005; 25(4):501–506.

25. Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981; 63(6):872–877.

26. Colaris JW, Allema JH, Reijman M, et al. Which factors affect limitation of pronation/supination after forearm fractures in children? A prospective multicentre study. Injury. 2014; 45(4):696–700.










 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download