Abstract
Background
Fixation of proximal chevron metatarsal osteotomy has been accomplished using K-wires traditionally and with a locking plate recently. However, both methods have many disadvantages. Hence, we developed an intramedullary fixation technique using headless cannulated screws and conducted a biomechanical study to evaluate the superiority of the technique to K-wire and locking plate fixations.
Methods
Proximal chevron metatarsal osteotomy was performed on 30 synthetic metatarsal models using three fixation techniques. Specimens in group I were fixated with K-wires (1.6 mm × 2) and in group II with headless cannulated screws (3.0 mm × 2) distally through the intramedullary canal. Specimens in group III were fixated with a locking X-shaped plate (1.3-mm thick) and screws (2.5 mm × 4). Eight metatarsal specimens were selected from each group for walking fatigue test. Bending stiffness and dorsal angulation were measured by 1,000 repetitions of a cantilever bending protocol in a plantar to dorsal direction. The remaining two samples from each group were subjected to 5 mm per minute axial loading to assess the maximal loading tolerance.
Results
All samples in group I failed walking fatigue test while group II and group III tolerated the walking fatigue test. Group II showed greater resistance to bending force and smaller dorsal angulation than group III (p = 0.001). On the axial loading test, group I and group II demonstrated superior maximum tolerance to group III (54.8 N vs. 47.2 N vs. 28.3 N).
Conclusions
Authors have demonstrated proximal chevron metatarsal osteotomy with intramedullary screw fixation provides superior biomechanical stability to locking plate and K-wire fixations. The new technique using intramedullary screw fixation can offer robust fixation and may lead to better outcomes in surgical treatment of hallux valgus.
There are more than 130 surgical procedures for hallux valgus (HV) deformity,1) and they are categorized into proximal, distal and midshaft procedures. Proximal procedures are often more popular for moderate to severe HV deformity as they allow a larger amount of correction compared to distal and midshaft procedures.23)
Common proximal procedures include the Ludloff osteotomy, proximal crescentic osteotomy, and proximal chevron metatarsal osteotomy (PCMO). The PCMO is known for its powerful reduction of the intermetatarsal angle by lateral angulation, translation and supination of fragments, and it has been reported to have relatively few complications.4) In comparison to the proximal crescentic osteotomy, the PCMO has shown a lower risk of malunion in the osteotomy site, less shortening and better sesamoid reduction,5) and when compared to the Ludloff osteotomy, the PCMO provides larger intermetatarsal angle correction with minimal changes in distal metatarsal articulation by translation.6)
Despite these benefits, lateral translation and angulation decrease the contact surface between two fragments, resulting in less stable fixation.6) In addition, the small proximal bone fragment and irregular medial cortical contour may make it difficult to secure. The conventional pin and screw fixation and the recent locking plate fixation all seem insufficient to provide stable fixation due to the small fixation surface and technical difficulties.7) It has also been reported that complications associated with insufficient fixation, loss of correction, and excessive shortening range from 17% to 28%.58)
We conjectured that considering the vectors of cantilever bending stress, locking plate fixation would not offer sufficient stability. Thus, we have introduced two 3.0-mm headless cannulated screws to secure intramedullary fixation comparable to the conventional K-wire fixation. We postulated that the headless screw fixation may deliver more ideal fixation with stability. The aims of our study are to compare our technique with other popular fixation techniques (two K-wire and locking plate fixations) in terms of various properties of biomechanical stability.
A total of 30 synthetic models of the first metatarsal (#3422, 4th Generation Metacarpal, Sawbones; Pacific Research Laboratories, Vashon, WA, USA) were included in this study. Each specimen model was a cortical bone analog containing short glass fiber reinforced epoxy that offered the possibility of improving the uniformity of mechanical properties within a composite replicate bone, allowing for greater anatomic detail to be added to the bones.9) The specimens were randomly assigned to three equal groups of 10 specimens. Group I was fixated with two K-wires of 1.6-mm diameter that was inserted along the intramedullary canal distally from the base of metatarsal. Group II was fixated with two 3.0-mm headless partial threaded cannulated screws (Titanium; Jeil Medical Corp., Seoul, Korea) in the same way as in group I. Group III was fixated with a 1.3-mm depth locking plate with four 2.5-mm locking screws (Titanium, Jeil Medical Corp.) (Fig. 1).
Proximal reverse chevron osteotomy was performed in all three groups. Using a 90° chevron cutting guide, each specimen was prepared with a reverse chevron cut at 10 mm distal from the base using a microsagittal saw. After Osteotomy, the distal fragment was displaced about 3 mm and 15° by lateral translation and rotation, and K-wire was used for temporary fixation. Ten osteotomized specimens were then randomly allocated to each group. Group I was fixated with two 1.6-mm K-wires advanced from the base of specimens to the metatarsal head through the intramedullary canal while group II was fixated with two 50 mm of 3.0-mm headless cannulated screws in the same way as in group I. Group III was fixated with a 1.3-mm locking plate and four 2.5-mm locking screws after slightly trimming the surface of specimens for better bone-to-locking plate contact. All specimens were examined under C-arm to confirm the degree of correction, the location of fixators, and fixation condition.
The metatarsocuneiform joint complex was stabilized by a uniaxial testing frame called Instron (E3000; Instron, Norwood, MA, USA) with a load cell of ± 5 kN Dynacell. The walking fatigue and axial loading tests were done. The axial loading test was performed at a loading speed of 5 mm per minute in the lateral to medial direction for all specimens. While the walking fatigue test was performed by applying 1,000 repetitions of bending force at 0.5 Hz, the sine wave ranged from 0 to 31 N in the plantar to dorsal direction (Fig. 2).610)
The axial loading test data were plotted in a load-displacement graph (N/mm) where the maximum load was shown instantly. The average of sudden descent of resistance in the graph was compared among groups. In the walking fatigue test, both bending stiffness and dorsal angulation at the peak load of 31 N were documented on the 1st, 10th, 50th, and 100th cycle, and then every 100 cycles until the 1,000th cycle. The slope of the latter one-quarter of the ascending load-displacement curve, a region that was consistently linear, was utilized to measure the stiffness of deflection of the distal metatarsal head. The number of broken specimens was calculated in each cycle, and the average bending stiffness and dorsal angulation of the intact specimens were compared among groups.
In the axial loading test, the maximum load for the K-wire was 54.8 N and for the headless cannulated screw was 47.2 N while it was only 28.3 N for the locking plate. The resistance of the locking plate construct to the load in the medial direction was significantly lower than that of the others (Fig. 3).
In the walking fatigue test, all the biomechanical variables were measured and constructs of cannulated screws and locking plates were compared statistically. All the eight K-wires were broken by cantilever bending force within the first 10 cycles: three in the first cycle, another three in the second cycle, one in the third cycle, and another one in the eighth cycle. On the other hand, cannulated screws and locking plates were intact until the 1,000th cycle or greater than 10° of distal fragment angulation (Table 1).
The mean bending stiffness of group I, II, and III were 3.21 N/mm (standard deviation [SD], 1.13 N/mm), 24.67 N/mm (SD, 0.54 N/mm), and 19.63 N/mm (SD, 1.22 N/mm), respectively (Fig. 4). Cannulated screws demonstrated superior bending stiffness to locking plates in all loading cycles, showing statistical significance (p = 0.001). K-wires were broken within the first 10 cycles.
Group II showed less dorsal angulation than group III in all loading cycles, showing statistical significance (p = 0.001). The average breaking point for all eight samples in group I was 12.23° (SD, 4.72°). The average dorsal angulation for group II was 2.19° (SD, 0.99°) at the 1st cycle, 2.32° (SD, 1.20°) at the 10th cycle, and 2.19° (SD, 1.06°) at the 1,000th cycle while the average dorsal angulation for the locking plate showed a tendency to decrease from 2.77° (SD, 1.21°) at the first cycle to 2.41° (SD, 1.23°) at the 1,000th cycle (Fig. 5).
There are many procedures for HV correction that have been proven to be safe and effective in previous research.11) Acevedo et al.12) demonstrated in a mechanical comparison test that the fatigue resistance of PCMO was not only superior to both the crescentic osteotomy and scarf osteotomy but also similar to the Ludloff osteotomy. To our knowledge, K-wire fixation has shown some complications such as dorsal malunion, pin irritation, and recurrence of deformity due to loss of correction caused by insufficient stability.1314) Hence, we decided to investigate a new fixation technique and its biomechanical property to prove the effectiveness of PCMO.
PCMO allows a large deformity correction and is relatively safe to perform due to the presence of a large surface area between two bone fragments. However, the long lever arm of the weight bearing metatarsal head yields a higher loading force and therefore less biomechanical stability than the distal chevron osteotomy.15) Because of this, complications including clinical recurrence, shortening, and dorsiflexion malunion are found in 18.7%.1314) Recently, biomechanical and clinical studies have emphasized the importance of robust fixation and described the results of new devices and techniques.
In recent studies, locking plates have proven superior fixation to K-wires or screws,4131617) and Schuh et al.10) emphasised the superior biomechanical properties of locking plate fixation. However, Park et al.7) compared the fixation properties of a 1.6-mm K-wire and a 2.4-mm minilocking plate and found a couple of limitations of locking plate fixation on the metatarsal surface. First, precise placement of the locking plate on the metatarsal surface was difficult due to the irregular bony surface, and locking screw holes were distorted by bending of the plate. In addition, there were more complications reported such as skin irritation, loss of correction, and recurrence of deformity. Schuh et al.10) carried out a biomechanical comparison study between the open wedge osteotomy with plate fixation and the Ludloff osteotomy with screw fixation and reported that the medial plate did not produce sufficient fixation strength under cantilever bending stress.
It has been believed that the conventional screw fixation is not only more prone to loss of correction due to bone spicule compression during insertion but also has limitations related to the direction and length of the screw as the osteotomy site is close to the first metatarsalcuneiform joint, possibly causing damage to the joint.1618) Moreover, it is contraindicated in osteoporotic bone due to the higher pull-out risk.19) K-wire fixation is one of the most popular methods using three-point fixation. It has a lower risk of loss of correction during operation; however, an insufficient fixation may lead to dorsal malunion upon weight bearing and pin irritation that requires additional procedure to remove the pin.19) Hence, we introduced new screw fixation technique, which showed a minimal correction loss during surgery comparable to K-wire fixation. With use of two 3.0-mm cannulated screws jammed in the medullary canal, the technique provided stable fixation and thus was found effective in our biomechanical study.
In the axial loading test, the K-wires and headless cannulated screws showed a resistance of 54.8 N and 47.2 N, respectively, which were higher than 28.3 N of the locking plate. These results may reinforce the following facts: (1) locking plates located on the side that receives the compression force can fail to act as support; (2) intramedullary fixation provides more distal fixation than the locking plate from the osteotomy site and therefore gives a larger load sharing surface of fixation; and (3) the location of the K-wire closer to the point where the maximum load is generated allows a high endurance to a gradual increase in the loading force.14) Moreover, these fixation techniques can be used for internal fixation, which clinically promotes secondary bone healing. K-wires showed a better resistance than headless cannulated screws in this study. We think that this is because the two 1.6-mm K-wires reaching the metatarsal head allows for “triple-stabilization” from the osteotomy site while the same cannulated screws of 50 mm in length do not reach the metatarsal head by being jammed in the intramedullary canal. Therefore, We believe this could be improved by precise measurement of screw length during surgery.
Bending stiffness and dorsal angulation in the walking fatigue test showed different resistances in relation to the continuous axial plane load due to both the vertical force of the cycling pattern and the bone spicule condition after the chevron cut. Bending stiffness of the cannulated screws and the locking plates were 7.7 and 6.1 times greater than that of the K-wires, and the cannulated screws were 26.3% stronger than the locking plates. We believe that the vertical force on the plantar aspect of the metatarsal head was transformed into anterior sliding force and dorsal bending force due to the chevron shape of the bony contour. The presence of a thread in the cannulated screw and locking plate allowed them better position to resist a sliding force, and intramedullary fixation was more effective in tolerating higher dorsal bending force than the medial locking plate. Due to these two properties, cannulated screw is believed to provide superior stiffness and resistance.
The average intramedullary diameter of the first metatarsal diaphysis has not been fully studied but Badwey et al.20) documented that the mean width of the metatarsal measured at 15 mm from the medial osteochondral junction was 15.3 mm (range, 13 to 18 mm; SD, 1.6 mm) in male specimens and 14.5 mm (range, 11 to 18 mm; SD, 1.6 mm) in female specimens. Considering this, we believe that two 3.0-mm cannulated screws can be introduced in the intramedullary canal and cross fixation would allow tight jamming. Studies on the width of medullary canal are warranted for patients with osteoporosis or a large metatarsal where two divergent fixed screws do not provide sufficient fixation and thus the use of one or two additional screws is considered. Our technique increases the chance of bone union due to the reaming effect of screw advancement and prevents the risk of skin irritation from headless screw, which is a huge clinical advantage. We are currently conducting clinical research on the effectiveness of the technique in the correction of HV.
In this study, we did not perform power analysis for sample size calculation, and the sample size may be too small to draw any meaningful statistical conclusion, especially on the axial loading test. We think that large size biomechanical studies are needed to confirm the results observed in this preliminary report. However, even though the viscoelastic properties of real bones were not perfectly reflected in saw bone models in our pilot study, the possible influence of bone mineral density difference as in cadaveric studies could be excluded and the reproducibility of our results were high as the mechanical property tests were conducted in the same condition.1120) Another limitation is that this was a biomechanical study with saw bone models that may not necessarily reflect clinical outcomes that require a clinical trial and follow-up. However, although axial loading in the cantilever test may not exactly reflect weight bearing force on the first metatarsal, our method had previously been used in other studies and allows comparison.1021)
Our biomechanical study has demonstrated superior fixation properties of the cannulated headless screws to K-wire and locking plate fixation in PCMO. However, one should keep in mind that the biomechanical results obtained in the present study have yet to be demonstrated in the clinical context. This preliminary report should be followed by further biomechanical studies using cadaver specimens.
Figures and Tables
Fig. 1
Fixation constructs for three groups. (A) Group I: K-wires (1.6 mm × 2). (B) Group II: headless cannulated screws (3.0 mm × 2). (C) Group III: locking plate (1.3 mm in depth) and screws (2.5 mm).

Fig. 3
Resistance capacity against laterally directed force. (A) K-wire group: maximum load, 54.8 N. (B) Cannulated screw group: maximum load, 47.2 N. (C) Locking plate group: maximum load, 28.3 N.
Fig. 4
Bending stiffness during loading of cantilever bending force. (A) Cannulated screw group. (B) Locking plate group.

Fig. 5
Dorsal angulation of distal fragment during loading of cantilever bending force. (A) Cannulated screw group. (B) Locking plate group.

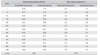
Table 1
Mean Bending Stiffness and Mean Angulation of the Walking Fatigue Test
Notes
CONFLICT OF INTEREST The authors did not receive financial support for this research. Although Jeil Medical Corporation donated materials for the study, such as specimens, screws, and plates and allowed us to use the equipment necessary for the biomechanical test, they had no influence on the conduct of the research.
References
1. Goldie I, Nielsen JM, Lundh N. Hallux valgus: review and results of surgical treatment. Lakartidningen. 1974; 71(1):63–68.
2. Aminian A, Kelikian A, Moen T. Scarf osteotomy for hallux valgus deformity: an intermediate followup of clinical and radiographic outcomes. Foot Ankle Int. 2006; 27(11):883–886.

3. Coetzee JC, Rippstein P. Surgical strategies: scarf osteotomy for hallux valgus. Foot Ankle Int. 2007; 28(4):529–535.

4. Schuh R, Willegger M, Holinka J, Ristl R, Windhager R, Wanivenhaus AH. Angular correction and complications of proximal first metatarsal osteotomies for hallux valgus deformity. Int Orthop. 2013; 37(9):1771–1780.

5. Easley ME, Kiebzak GM, Davis WH, Anderson RB. Prospective, randomized comparison of proximal crescentic and proximal chevron osteotomies for correction of hallux valgus deformity. Foot Ankle Int. 1996; 17(6):307–316.

6. Scott AT, DeOrio JK, Montijo HE, Glisson RR. Biomechanical comparison of hallux valgus correction using the proximal chevron osteotomy fixed with a medial locking plate and the Ludloff osteotomy fixed with two screws. Clin Biomech (Bristol, Avon). 2010; 25(3):271–276.

7. Park CH, Ahn JY, Kim YM, Lee WC. Plate fixation for proximal chevron osteotomy has greater risk for hallux valgus recurrence than Kirschner wire fixation. Int Orthop. 2013; 37(6):1085–1092.

8. Mann RA, Rudicel S, Graves SC. Repair of hallux valgus with a distal soft-tissue procedure and proximal metatarsal osteotomy: a long-term follow-up. J Bone Joint Surg Am. 1992; 74(1):124–129.

9. Heiner AD, Brown TD. Structural properties of a new design of composite replicate femurs and tibias. J Biomech. 2001; 34(6):773–781.

10. Schuh R, Hofstaetter JG, Benca E, et al. Biomechanical analysis of two fixation methods for proximal chevron osteotomy of the first metatarsal. Int Orthop. 2014; 38(5):983–989.

12. Acevedo JI, Sammarco VJ, Boucher HR, Parks BG, Schon LC, Myerson MS. Mechanical comparison of cyclic loading in five different first metatarsal shaft osteotomies. Foot Ankle Int. 2002; 23(8):711–716.

13. Varner KE, Matt V, Alexander JW, et al. Screw versus plate fixation of proximal first metatarsal crescentic osteotomy. Foot Ankle Int. 2009; 30(2):142–149.

14. Bong MR, Kummer FJ, Koval KJ, Egol KA. Intramedullary nailing of the lower extremity: biomechanics and biology. J Am Acad Orthop Surg. 2007; 15(2):97–106.

15. Shereff MJ, Sobel MA, Kummer FJ. The stability of fixation of first metatarsal osteotomies. Foot Ankle. 1991; 11(4):208–211.

16. Jones C, Coughlin M, Petersen W, Herbot M, Paletta J. Mechanical comparison of two types of fixation for proximal first metatarsal crescentic osteotomy. Foot Ankle Int. 2005; 26(5):371–374.

17. Gallentine JW, Deorio JK, Deorio MJ. Bunion surgery using locking-plate fixation of proximal metatarsal chevron osteotomies. Foot Ankle Int. 2007; 28(3):361–368.

18. Sammarco VJ, Acevedo J. Stability and fixation techniques in first metatarsal osteotomies. Foot Ankle Clin. 2001; 6(3):409–432.

19. Lian GJ, Markolf K, Cracchiolo A 3rd. Strength of fixation constructs for basilar osteotomies of the first metatarsal. Foot Ankle. 1992; 13(9):509–514.

20. Badwey TM, Dutkowsky JP, Graves SC, Richardson EG. An anatomical basis for the degree of displacement of the distal chevron osteotomy in the treatment of hallux valgus. Foot Ankle Int. 1997; 18(4):213–215.

21. Trnka HJ, Parks BG, Ivanic G, et al. Six first metatarsal shaft osteotomies: mechanical and immobilization comparisons. Clin Orthop Relat Res. 2000; (381):256–265.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download