Abstract
Background
This study aims to compare the surgical outcomes of open reduction and internal fixation (ORIF) and minimally invasive plate osteosynthesis (MIPO) using a screw compression method in simple humeral shaft fractures.
Methods
This retrospective study was performed with 50 patients who had surgical interventions for the treatment of simple humeral shaft fractures and had follow-ups of at least 12 months in Ulsan University Hospital between August 2008 and June 2015. Group 1 included 23 patients treated with ORIF and group 2 included 27 patients treated with the MIPO technique using a locking screw plate. The time to clinical/radiographic union, the joint range of motion (ROM), and function were evaluated.
Results
The average time to clinical/radiographic bone union was shorter in group 2 (12.0 ± 3.7 weeks/14.8 ± 2.0 weeks in group 1 and 9.4 ± 1.3 weeks/12.0 ± 3.3 weeks in group 2; p = 0.022/p = 0.034). Shoulder and elbow joint function evaluated by joint ROM and visual analogue scale (VAS), Korean Shoulder Elbow Society (KSS), American Shoulder and Elbow Surgeons (ASES), and the University of California at Los Angeles (UCLA) scores was excellent in both groups. On the average shoulder ROM at 12 months after the operation, group 1 had forward elevation of 160°, external rotation of 30° in adduction and lumbar vertebra 10 level in internal rotation and group 2 had forward elevation of 170°, external rotation of 35° in adduction and lumbar vertebra 9 level in internal rotation. The mean VAS, KSS, ASES, and UCLA scores were 2.8, 87.0 ± 0.9, 89.4 ± 0.9, and 31.0 ± 1.4, respectively, in group 1 and 1.7, 89.1 ± 2.7, 91.0 ± 1.6, and 32.4 ± 3.2, respectively, in group 2. There were statistically significant intergroup differences in VAS score (p = 0.011). There were significantly less postoperative infections in group 2 (three cases, 10.7% in group 1 and 0 case in group 2; p = 0.041) although all of them were superficial infections and well-treated by an average 4-week course of antibiotics (range, 2 to 6 weeks).
Increasing traffic accidents and sports activities result in the increased incidence of humeral fractures, about 30%–50% of which are humeral shaft fractures.1) It is known that union can be achieved by conservative management in humeral shaft fractures but operative intervention may be helpful to accelerate bone union and rehabilitation.234) Although there are established surgical indications for humeral shaft fractures,5) in recent years, operative treatment is often performed for early rehabilitation and return to daily life activities.6) In the case of tibial fractures, the minimally invasive plate osteosynthesis (MIPO) technique is commonly used for internal fixation to increase the chance of bone union by preserving the biological environment.7) Although there are growing attempts to implement the MIPO technique in humeral shaft fractures, the treatment outcome of MIPO in simple humeral fractures has not been satisfactory because it is difficult to obtain additional compressive strength at the fracture site.89)
Therefore, open reduction and internal fixation (ORIF) is the preferred surgical method for simple humeral fractures, despite the problems innate in the open reduction technique. Extensive skin incisions raise the risk of postoperative infection and cosmetic problems and periosteal exposure requires a longer bone union time. To avoid such problems inherent to ORIF, we have attempted to perform the MIPO technique using a screw compression method, which we believed would provide additional compressive strength at the fracture site.
In this study, we compared the surgical outcomes of ORIF and MIPO using a screw compression method in simple humeral shaft fractures.
This retrospective study was performed with 50 patients who had surgical interventions for the treatment of simple humeral shaft fractures and had follow-ups for at least 12 months in Ulsan University Hospital between August 2008 and June 2015. The demographics of study population are presented in Table 1. Patients with open fractures and any nerve injury before surgery were excluded in this study.
The subjects were divided into two groups. Group 1 included 23 patients who had ORIF and group 2 included 27 patients who were treated with the MIPO technique using a locking screw plate. This study was approved by the Institutional Review Board of Ulsan University Hospital (IRB No. 2017-02-021) and informed consent was obtained from all subjects. The mean age of the subjects was 50 years (range, 35 to 70 years) and there were 34 male patients and 16 female patients. There were 11 cases of transverse fracture, five cases of oblique fracture, and seven cases of spiral fracture in group 1 and 16 cases of transverse fracture, five cases of oblique fracture, and six cases of spiral fracture in group 2. The sufficient sample size suggested by a power analysis was 52 patients (26 patients in each group) to achieve a statistical power of 99% with a two-sided α level of 0.05 presuming an effect size of 0.8.
For all subjects, 4.5-mm narrow limited contact locking compression plates (LC-LCP; Synthes, Zuchwil, Switzerland) and locking screws were used and conventional screws were additionally used for effective reduction. The patients were positioned in supine position under general anesthesia and the upper arm was abducted to 90° and the forearm was supinated to visualize the anterior site of the upper arm.
In group 1, a conventional anterolateral approach was used. In supine position, a 10-cm skin incision was made on the fracture site and the deltoid muscle and the biceps brachii muscle were exposed. The biceps brachii was medially retracted and the brachialis muscle was vertically incised to expose the fracture site. Once the periosteum was detached and a hematoma was evacuated, a locking plate and screws were applied using a reduction clamp.
In group 2, about 4-cm skin incision (range, 2 to 6 cm) was made on the proximal area of the fracture site for proximal window. With the anterolateral approach, an incision was made on the proximal humerus and the periosteum of the proximal humerus shaft was exposed between the deltoid muscle and the long head of the biceps brachii. About 3-cm skin incision (range, 2 to 4 cm) was anteriorly made on the distal humerus from 5–6 cm superior to the elbow joint for distal window. The biceps brachii muscle was medially retracted and the musculocutaneous nerve was carefully dissected and laterally retracted. When the brachialis was exposed, a vertical incision was made in the middle portion, and the distal humerus was exposed. Paying special attention not to damage the nearby soft tissues and the periosteum around the fracture site, a locking plate was placed on the anterior surface of the humeral shaft and a locking screw was inserted through the proximal incision. Then, indirect reduction was performed using an image intensifier and another locking screw was inserted through the distal incision. To avoid periosteal tears and radial nerve injuries during the insertion of the locking plate and screws, external rotation of the forearm during the intervention is recommended. When a proper bone alignment was achieved, compressive strength was obtained using conventional screws. For that purpose, the locking screws were slightly loosened (about 1/3) to maintain the bone alignment, and the conventional screws were inserted into the nearest holes from the fracture site to obtain compression. The holes were drilled further away from the fracture site and conventional screws were applied to obtain compression. Once the compressive strength was obtained on the fracture site, 2–3 locking screws were additionally applied inferior and superior to the fracture site. The locking screws initially inserted to maintain the bone alignment were removed at the end. Only after satisfactory reduction was achieved, two compression screws were replaced with locking screws. This operative procedure is demonstrated in Fig. 1 and a successful case using this technique is demonstrated in Figs. 2, 3, 4. The understanding of the anatomy of the radial nerve is important because percutaneous insertion of a plate can cause radial nerve palsy. The radial nerve runs medially from the humeral shaft in the proximal third of the humerus, posteriorly from the humeral shaft in the middle third of the humerus and laterally from the humeral shaft in the distal third of the humerus. Thus, the plate was anteriorly inserted to minimize lateral dissection and radial nerve injuries. If a plate is laterally inserted during MIPO, special attention should be paid during the advancement of the plate towards the distal humerus. The plate should be placed posterior to the long head of the biceps brachii and the holes should be carefully drilled through the other side of the cortex of the humerus to prevent radial nerve damage.
The length of the plate was determined allowing for insertion of 3–4 screws in the plate holes from the fracture site. The distance to the nearest screws on both sides from the fracture site (working distance) was determined to evenly distribute the stress on the plate.
A right-angled long arm splint that protects the elbow joint was applied immediately after the operation, and the development of radial nerve injury was closely observed on a regular basis. Shoulder, elbow, finger, and wrist range of motion (ROM) exercises were carefully started on the postoperative day 2 or 3. After 2 weeks, the long arm splint was removed and active exercises were commenced. Resistant exercises were initiated after 3 months.
Radiographic examination was performed immediately after the operation and then every 2 weeks for the first 4 months, every month for the next 2 months, and every 3 months afterwards to evaluate radiographic union and deformity. Radiographic union was considered achieved when bone bridges of the three cortices became visible on anteroposterior and lateral X-ray views. Clinical union was defined as the absence of pain or tenderness at the fracture site. The subjects were followed up every 6 months for functional assessment after union. Postoperative evaluation was done in an outpatient clinic setting solely by a single operator.
Postoperative functional ability was evaluated using Korean Shoulder Elbow Society (KSS) score (100 points) which is comprised of activities of daily living function (30 points), pain (20 points), self-reported assessment (10 points), shoulder ROM (20 points), muscle strength (10 points), and endurance (10 points). American Shoulder and Elbow Surgeons (ASES) score and the University of California at Los Angeles (UCLA) score (35 points) were also used to evaluate shoulder function. Pain was assessed using a visual analogue scale (VAS). For the evaluation of the shoulder ROM, forward elevation, external rotation, and internal rotation were measured with the shoulder abducted, and flexion and extension angles of the elbow joint were assessed.
Statistical analysis was performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) with a significance level set at p < 0.05. To evaluate characteristics of study population and compare postoperative outcomes between two groups, statistical analyses were performed using a Mann-Whitney U-test. Due to the limitation of the retrospective study design, there were a slightly insufficient number of subjects, which was compensated by using nonparametric statistics.
There were no significant differences in the mean age, sex, follow-up time, delayed surgical days, and fracture patterns between the two patient groups (Table 1). Complete bone union was obtained during the follow-up period in all subjects. The average time to clinical/radiographic bone union was shorter in group 2 (12.0 ± 3.7 weeks/14.8 ± 2.0 weeks in group 1 vs. 9.4 ± 1.3 weeks/12.0 ± 3.3 weeks in group 2), showing statistically significant difference (p = 0.022 and p = 0.034).
Shoulder and elbow joint function evaluated by joint ROM and VAS, KSS, ASES, and UCLA scores was excellent in both groups. The average shoulder ROM of group 1 at 12 months after the operation was forward elevation of 160°, external rotation of 30° in adduction and thoracic vertebra 10 level in internal rotation. The average shoulder ROM of the group 2 at 12 months after the operation was forward elevation of 170°, external rotation in adduction of 35° and thoracic vertebra 9 level in internal rotation. The mean VAS, KSS, ASES, and UCLA scores of group 1 were 2.8, 87.0 ± 0.9, 89.4 ± 0.9, and 31.0 ± 1.4, respectively. Those of group 2 were 1.7, 89.1 ± 2.7, 91.0 ± 1.6, and 32.4 ± 3.2, respectively. There were statistically significant differences in VAS scores (p = 0.011) (Table 2). Radial nerve palsy occurred in two patients in group 1 (7.2%) and in one patient in group 2 (4.2%), all of which subsided within 3 months. There were significantly less postoperative infections in group 2 (three cases, 10.7% in group 1 vs. 0 case in group 2; p = 0.041) although all were superficial infections and well-treated by an average 4-week course of antibiotics (range, 2 to 6 weeks).
The study results demonstrated satisfactory surgical outcomes of MIPO using a screw compression method in the treatment of humeral simple fractures. The use of MIPO technique is gradually increasing not only for the treatment of humeral shaft fractures but also for other fractures since it facilitates bone healing process by preserving the biological environment of fracture sites and the technique is easy to perform.10) Conservative management used to be the gold standard for the treatment of humeral shaft fractures. Lately, however, the use of operative treatment is increasing for rapid return to daily life. In the past, internal fixation or intramedullary nailing fixation with conventional screws and plates was primarily performed for the treatment of humeral shaft fracture, but, in recent years, the use of MIPO technique is increasing.11121314) The MIPO technique is generally used for shaft fractures and metaphyseal fractures accompanying osteoporosis, which can be treated with indirect reduction as anatomical reduction is not required and for multi-fragmentary fractures, which can be treated with bridging plate fixation. However, the MIPO technique can also be used for simple shaft fractures and metaphyseal fractures.151617181920)
Bae et al.6) reported that there were no statistically significant differences in the time to union among the plate fixation, intramedullary fixation and external fixation performed for the treatment of humeral shaft fractures. Among humeral shaft fractures, simple fractures which can be treated with conventional ORIF with excellent surgical outcomes can also be an indication for MIPO considering the convenience of the MIPO technique. The convenience of the technique includes wide acceptable range of fragmentary displacement and unproblematic use of the devices.
In cases of simple humeral shaft fractures, conventional ORIF without excessive stripping of soft tissues, performed by experienced surgeons, resulted in excellent postoperative ROM and minimal postoperative infections. In general, postoperative infection rates are lower in MIPO than in conventional ORIF because MIPO preserves blood supply to the bone and nearby soft tissues.21222324) Furthermore, postoperative infections after MIPO are less aggressive and easier to manage than those after conventional ORIF because infection after MIPO tends to be limited in the plate and soft tissues and the periosteum is well preserved. 7) Despite the advantages of MIPO, ORIF remains the most popular treatment option for the management of simple humeral shaft fractures by achieving anatomical reduction; MIPO has not yet been fully proven to be an equally effective method for the treatment of humeral shaft fractures.
We have achieved satisfactory results by using the MIPO technique to overcome the disadvantages of ORIF; by applying additional compressive force to the fracture site using compression screws, we have successfully minimized the fracture gap size. In addition to the technical convenience mentioned above, the advantages of MIPO encompass creating a better biological environment around the fracture site, omission of plate bending and cosmetic benefits.2526) Moreover, possible complications such as iatrogenic fractures and limited ROM after intramedullary fixation were significantly reduced.27)
In our study, significantly shorter clinical/radiographic bone union time was found in the MIPO group, probably due to the intact periosteum and periosteal vessels. In addition, the VAS score 1 year postoperatively was also significantly lower in the MIPO group due to the relatively small skin incision and less soft tissue stripping. Elbow and shoulder function and ROM assessed using KSS, UCLA, and ASES scoring systems showed excellent results in both groups.
Risks of secondary radial nerve injury, as one of the most serious complications that may occur in both ORIF and MIPO groups, associated with surgical treatment of humeral shaft fractures should be acknowledged. In ORIF, the radial nerve can be exposed and protected. In MIPO, however, the understanding of the anatomic course of the nerves is required as nerves cannot be visualized, increasing the risk of intraoperative nerve injury. The radial nerve can be damaged by a retractor or a plate and screws because it is located medial to the proximal one third of the humerus, posterior to the middle one third of the humerus, and lateral to the distal one third of the humerus.1928) Thus, special attention should be paid when a retractor is used during the operation and a plate is inserted into the distal humerus. Apivatthakakul et al.28) reported that radial nerve damages and plate bending can be prevented if the forearm is kept in full supination during the insertion of a plate in a cadaver study. We also used this method in this study, which resulted in temporary radial nerve palsy in one case. Drilling at the middle of the humerus to make holes for screws as well as screw insertion should be carefully done to avoid too deep insertion of the screws. Radial nerve damage could be minimized with this method, so there was only one case of postoperative radial nerve palsy in group 2 in contrast to two cases in group 1.
Although there is a risk of radial nerve damage in the MIPO technique, it can be prevented by careful manipulation to maximize advantages of the technique. This study results showed that the use of MIPO technique in the treatment of humeral shaft fractures provided an excellent bone union rate and functional outcome. Limitations of this study include the small sample size and the retrospective study design. Therefore, prospective studies involving a greater number of subjects are needed for objective comparison with our findings in the future.
The surgical outcome of MIPO using a screw compression method in simple humeral shaft fractures demonstrated results superior to those of ORIF in terms of the time to clinical/radiographic union, pain score, and postoperative infection rate.
Figures and Tables
 | Fig. 1Minimally invasive plate osteosynthesis using a screw compression method. (A) A proper bone alignment is achieved using two locking screws. (B) Compressive force is obtained at the fracture site using two compression screws. (C) Additional locking screws are inserted. (D) Compression screws are replaced with locking screws. |
 | Fig. 2Preoperative radiographs of a 33-year-old male showing a transverse fracture in the middle portion of the humeral shaft. (A) Anteroposterior view. (B) Lateral view. |
 | Fig. 3Simple radiographs showing satisfactory results in the immediate postoperative period. (A) Anteroposterior view. (B) Lateral view. |
 | Fig. 4Simple radiographs showing radiologic union 5 months postoperatively. (A) Anteroposterior view. (B) Lateral view. |
Table 1
Characteristics of Study Population
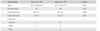
Table 2
Comparison of 12-Month Postoperative Outcomes between Two Groups

Values are presented as mean ± standard deviation.
Group 1: patients who had open reduction and internal fixation, Group 2: patients who were treated with the minimally invasive plate osteosynthesis technique using a locking screw plate, VAS: visual analogue scale, KSS: Korean Shoulder Elbow Society, UCLA: University of California at Los Angeles, ASES: American Shoulder and Elbow Surgeons.
References
1. Volgas DA, Stannard JP, Alonso JE. Nonunions of the humerus. Clin Orthop Relat Res. 2004; (419):46–50.

2. Fears RL, Gleis GE, Seligson D. Diagnosis and treatment of complications: fractures of the diaphyseal humerus. In : Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma: fractures, dislocations, ligamentous injuries. Toronto: WB Saunders;1998. p. 567–578.
3. Gregory PR. Fractures of the humeral shaft. In : Rockwood CA, Green DP, Heckman JD, Bucholz RW, editors. Rockwood and Green's fractures in adults. Philadelphia, PA: Lippincott Williams & Wilkins;2002. p. 973–976.
4. Schemitsch EH, Bhandari M. Fractures of the diaphyseal humerus. In : Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma: basic science, management, and reconstruction. Toronto: WB Saunders;2003. p. 1481–1511.
5. McKee MD. Fractures of the shaft of the humerus. In : Bucholz RW, Heckman JD, Court-Brown C, Koval KJ, Tornetta P, Wirth MA, editors. Rockwood and Green's fractures in adults. Philadelphia, PA: Lippincott Williams & Wilkins;2006. p. 1117–1159.
6. Bae SW, Kim WJ, Song BY, Choi NH, Lee JH. Postoperative functional assessments in adult humerus shaft fractures: comparison among plates and screws, intramedullary nail and external fixator. J Korean Soc Fract. 2001; 14(2):228–235.

8. Sohn HS, Shin SJ. Minimally invasive plate osteosynthesis for proximal humeral fractures: clinical and radiologic outcomes according to fracture type. J Shoulder Elbow Surg. 2014; 23(9):1334–1340.

9. Shin SJ, Sohn HS, Do NH. Minimally invasive plate osteosynthesis of humeral shaft fractures: a technique to aid fracture reduction and minimize complications. J Orthop Trauma. 2012; 26(10):585–589.
10. Xue Z, Jiang C, Hu C, Qin H, Ding H, An Z. Effects of different surgical techniques on mid-distal humeral shaft vascularity: open reduction and internal fixation versus minimally invasive plate osteosynthesis. BMC Musculoskelet Disord. 2016; 17:370.

11. Kim JW, Oh CW, Byun YS, Kim JJ, Park KC. A prospective randomized study of operative treatment for noncomminuted humeral shaft fractures: conventional open plating versus minimal invasive plate osteosynthesis. J Orthop Trauma. 2015; 29(4):189–194.

12. Moon JG, Kwon HN, Biraris S, Shon WY. Minimally invasive plate osteosynthesis using a helical plate for metadiaphyseal complex fractures of the proximal humerus. Orthopedics. 2014; 37(3):e237–e243.

13. Esmailiejah AA, Abbasian MR, Safdari F, Ashoori K. Treatment of humeral shaft fractures: minimally invasive plate osteosynthesis versus open reduction and internal fixation. Trauma Mon. 2015; 20(3):e26271.

14. Shetty MS, Kumar MA, Sujay K, Kini AR, Kanthi KG. Minimally invasive plate osteosynthesis for humerus diaphyseal fractures. Indian J Orthop. 2011; 45(6):520–526.

15. Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003; 34:Suppl 2. B63–B76.

16. Mast J, Jakob R, Ganz R. Planning and reduction technique in fracture surgery. Berlin, Germany: Springer-Verlag;1989. p. 49–54.
17. Perren SM. Evolution of the internal fixation of long bone fractures: the scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002; 84(8):1093–1110.
18. Ruedi TP, Murphy WM. AO principles of fracture management. Stuttgart, Germany: Thieme;2000. p. 68–75.
19. Tong GO, Bavonratanavech S. Minimally invasive plate osteosynthesis (MIPO): concepts and cases presented by AO East Aisa. Stuttgart, Germany: Thieme;2007. p. 99–108.
20. Wagner M. General principles for the clinical use of the LCP. Injury. 2003; 34:Suppl 2. B31–B42.

21. Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000; (375):69–77.

22. Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury. 1997; 28:Suppl 1. A20–A30.

23. Schutz M, Muller M, Krettek C, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001; 32:Suppl 3. SC48–SC54.

24. Stannard JP, Wilson TC, Volgas DA, Alonso JE. Fracture stabilization of proximal tibial fractures with the proximal tibial LISS: early experience in Birmingham, Alabama (USA). Injury. 2003; 34:Suppl 1. A36–A42.

25. Jung SW. Indirect reduction maneuver and minimally invasive approach for displaced proximal humerus fractures in elderly patients. Clin Orthop Surg. 2013; 5(1):66–73.

26. Park J, Jeong SY. Complications and outcomes of minimally invasive percutaneous plating for proximal humeral fractures. Clin Orthop Surg. 2014; 6(2):146–152.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download