Abstract
Background
This study aimed to compare stability, functional outcome, and second-look arthroscopic findings after anterior cruciate ligament reconstruction between remnant-preserving tibialis tendon allograft and remnant-sacrificing hamstring tendon autograft.
Methods
We matched two groups (remnant-preserving tibialis tendon allograft group and hamstring tendon autograft group) in terms of demographic characteristics, associated injury, and knee characteristics. Each group consisted of 25 patients.
Results
Operation time was longer in the remnant-preserving tibialis tendon allograft group, but there was no significant intergroup difference in stability, clinical outcome, and second-look arthroscopic findings.
Conclusions
When an autograft is not feasible in anterior cruciate ligament reconstruction, the remnant-preserving technique can produce comparable results in terms of restoration of function, stability of the knee, and degree of synovium coverage at second-look arthroscopy compared to remnant-sacrificing hamstring autograft.
Graft options for anterior cruciate ligament reconstruction (ACLR) including bone-patellar tendon-bone autograft, hamstring autograft, quadriceps autograft, and bone-tendon-bone allograft generally have similar outcomes in the literature.1) Although the bone-patellar tendon-bone autograft has been considered the most suitable graft for ACLR, the use of hamstring autografts in ACLR has increased recently due to the advantage of lesser donor site morbidity.2) However, others have reported a deficit of knee flexor power and saphenous nerve injury in patients with hamstring tendon autografts.3) Due to these short-comings of autograft, the use of allograft tissue in primary ACLR has been increasing (from 17.4% in 2002 to 45.6% in 2008). The main advantage of allograft tissue is that it does not cause donor site morbidity. In addition, it has advantages such as shorter operation time, minimal incision, less postoperative pain, maintenance of the normal mechanism of flexors and extensors, and lager graft size.4) However, allograft also has major disadvantages with a potential of slower incorporation and inadequate ligamentization. 5) The use of allograft tissue in young athletic patients, especially in those less than 25 years of age, has recently been questioned because of documented failure rates as high as 23% compared to 6% for autograft.6)
Theoretically, ACLR with preservation of the remnant ACL has the following advantages: (1) accelerated revascularization and ligamentization, (2) preservation of proprioceptive nerve fibers, (3) enhanced biological environment for healing, (4) maintenance of the anchor point at the native tibial attachment, and (5) lower incidence of tibial bone tunnel enlargement.7) Therefore, if allograft tissue is selected instead of autograft tendon for various reasons in ACLR, care should be taken to preserve the remnants as much as possible. However, ACRL with a remnant-preserving technique is known to have disadvantages such as tunnel malposition and formation of cyclops lesions. Therefore, the use of a remnant-preserving technique in ACLR remains controversial.
It is currently unknown whether the remnant preservation technique could compensate for the disadvantages of allograft described above in ACLR. There are many literatures that simply compare allograft with autograft or compare a remnant preservation technique with a remnant sacrificing technique in ACLR. However, no previous study has compared a remnant-preserving allograft tendon and remnant-sacrificing autograft tendon. Therefore, the objective of this study is to compare postoperative stability, functional outcome, second-look arthroscopic findings, presence of cyclops lesions, operation time, and femoral and tibial tunnel positions of the knee after ACLR with remnant-preserving tibialis tendon allograft or with remnant sacrificing hamstring tendon autograft. We have the following hypotheses: (1) clinical outcome and second-look arthroscopic findings are comparable between remnant-preserving tibialis tendon allograft and remnant sacrificing hamstring tendon autograft and (2) remnant preservation technique does not increase the risk of cyclops lesions or incorrect tunnel position.
The protocol of this study was approved by the Ewha Womans University Mokdong Hospital Ethical Committee (IRB No. 2016-11-021-002) and performed in accordance with the principles of the Declaration of Helsinki. Advantages and disadvantages of both methods were explained to patients and informed consent was obtained from them before inclusion for this study.
This was a single-center retrospective, nonrandomized, and matched-pair analysis study with prospectively collected data evaluating clinical and second-look arthroscopic findings of ACLR using remnant-preserving tendon allograft versus remnant-sacrificing hamstring tendon autograft. Among 185 patients having anatomical single-bundle ACLR using the outside-in technique for the femoral tunnel from February 2010 to March 2014, 135 patients who underwent second-look arthroscopy were included. Exclusion criteria were as follows: (1) multiple ligament injury requiring concomitant surgery, (2) evidence of osteoarthritis on radiographs, (3) revision ACLR, (4) patient who did not have three-dimensional computed tomography (3D CT), (5) tunnel entrance that could not be clearly identified in 3D CT, and (6) patients who did not have at least 2 years of follow-up. There were 25 patients in the remnant-preserving tibialis tendon allograft ACLR group (group A) and 25 patients in the hamstring tendon autograft ACLR group (group H). The two groups were matched in terms of demographic characteristics, associated injury, and knee characteristics. All patients were followed for at least 2 years.
All patients underwent examination under anesthesia and diagnostic arthroscopy for treatment of meniscal lesions before ACLR. Tibialis tendon allograft or hamstring autograft was prepared for ACL graft. For the hamstring autograft, a 3 cm longitudinal skin incision was made at 2 cm medial to the tibial tuberosity. Then, we harvested the semitendinosus tendon and gracilis tendon. A quadruple semitendinosus/gracilis graft was prepared. The procedure for remnant preservation technique is described in detail below.
A suture hook with Maxon (Covidien, Dublin, Ireland) monofilament absorbable suture was inserted into the anteromedial portal and passed through the remnant ACL tissue (Fig. 1). Both free ends of the suture were retrieved through the anterior portal. Repeatedly, two or three more stitches of the remnant ACL tissue were performed and pulled out through the anterior portal (Fig. 2).
The remaining ACL fibers were generally preserved. Anatomical femoral and tibial tunnels were made. A tibial tunnel was made with an ACL tibial guide set at 45° to 50° angle while a femoral tunnel was made with flipcutter (Arthrex, Naples, FL, USA) using the outside-in technique. After making the femoral tunnel, additional PDS (Covidien, Dublin, Ireland) suture was passed through the femoral tunnel with a shuttle relay method and retrieved through the anterior portal. When making the femoral tunnel, a posterolateral portal was made if necessary to ensure the field of view. The tip of the tibial guide was positioned toward the central portion of the remnant tissue. The space for passing the graft into the remnant tissue was prepared.
Ends of Maxon sutures were inserted into the PDS loop and retrieved through the femoral tunnel. Graft passage was then started from the tibial tunnel to the femoral tunnel. During graft passage, the remnant tissue was retracted by a probe to allow passage of the graft to the femoral tunnel. After confirming graft passage, the suture was tied with a TightRope device (Arthrex) over a button. Then, sutures were tied with each other (Fig. 3). For tibial side graft fixation, the knee joint was held at a flexion of about 20°–30°. Then, an absorbable interference screw was fixed in the tibial tunnel with a spiked washer and a cortical screw.
The same rehabilitation protocol was used for both groups. Quadriceps exercises were started immediately after operation. Two days after operation, an ACL hinge brace was applied with the knee joint fully extended. Flexion exercise was started and gradually increased to full range of motion at 2 weeks after operation with the ACL hinge brace in place. Patients progressed to active closed chain exercises by 6 weeks after operation, and then to running at 2 to 3 months after operation. They returned to sports and full activity at 6 months after operation. In cases of combined meniscus repair, a cylinder splint was maintained for about 4 weeks and full weight bearing was delayed for about 6 weeks.
Patients had routine postoperative follow-ups at 2 weeks, 6 weeks, 3 months, 6 months, 12 months, and 24 months. Knee stability was evaluated by radiological anterior draw test using a Telos stress device (Daiseung Medics, Seoul, Korea) and a KT-1000 arthrometer (MEDmetric, San Diego, CA, USA). Difference in anterior translation between the affected and contralateral uninjured knees was assessed to determine the laxity. The two groups were compared and analyzed preoperatively and at the final follow-up. For clinical evaluation, International Knee Documentation Committee (IKDC) score and Lysholm knee score were evaluated preoperatively and at the final follow-up.
Second-look arthroscopy was performed only in patients who agreed to have tibial fixation screw removed. Risks and benefits of second-look arthroscopy were explained. In second-look arthroscopy, the following were assessed: subjective extent of the synovial coverage and prevalence of cyclops-like mass formation. The degree of synovial coverage was recorded as follows: less than 50% (pale), more than 50% (half), nearly entirely covered (good) (Fig. 4). All complications such as infection and harvest-site morbidity were evaluated.
CT scanning was performed with the knee in extended position within 1 week after the surgery. Images were taken with a Somatom Sensation Cardiac 64 (Siemens, Munich, Germany). Conventional volume-rendering 3D surface models were obtained using 3D-inspace software (Siemens). Files were converted to Digital Imaging and Communication in Medicine format and transmitted to picture archiving and communication system (PiViewSTAR 5.0; Infinitt, Seoul, Korea) for geometric measurements. From these 3D CT images, placements of femoral and tibial tunnels were assessed by determining centers of femoral and tibial tunnel apertures.8) To evaluate femoral tunnel placement, the quadrant method described by Bernard et al.9) was used for a true medial view of the femur (Fig. 5). To evaluate tibial tunnel placement, a true proximal-to-distal view on the tibial plateau described by Tsuda et al.10) was used (Fig. 6).
The operation time was checked retrospectively based on the operation record. Operation time was calculated as the time during which the tourniquet was applied.
Continuous variables are reported as mean ± standard deviation. Clinical scores, displacement on stress test and KT-1000 arthrometer, and degree of synovial coverage in second-look arthrography were compared between the two groups using Mann-Whitney test. Quantitative variables were described and compared using mean scores with 95% confidence interval. All statistical analyses were performed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was considered at p < 0.05 for all analyses.
Demographic characteristics and results of comparison for combined meniscal injuries and surgical procedures between the two groups are shown in Table 1. At the time of initial evaluation, the two groups were similar to each other with respect to demographic data. There was no deep infection, neurologic complication, or wound problem in either group postoperatively.
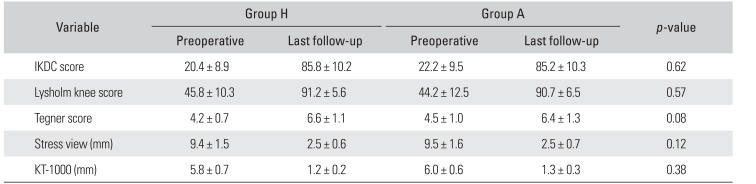
The average subjective IKDC score was increased from 22.2 preoperatively to 85.2 at the final follow-up in group A and from 20.4 to 85.8 in group H. The average Lysholm score was increased from 44.2 preoperatively to 90.7 in group A and from 45.8 to 91.2 in group H. Subjective IKDC knee score and Lysholm score were significantly improved postoperatively in both groups. However, the two groups did not differ significantly in functional assessment at the final follow-up.
On the instrumented stability test performed using the Telos device, the mean preoperative anterior translation was 9.49 mm and the mean final follow-up anterior translation was 2.53 mm in group A. In group H, the mean preoperative anterior translation was 9.38 mm and the mean final follow-up anterior translation was 2.49 mm. On the test performed using the KT-1000 arthrometer, the mean preoperative anterior translation was 6.0 mm and the mean final follow-up anterior translation was 1.3 mm in group A. In group H, the mean preoperative anterior translation was 5.8 mm and the mean final follow-up anterior translation was 1.2 mm. Stability was improved postoperatively in both groups. However, the two groups did not differ significantly in the improvement of stability between the preoperative and final follow-up assessments. Results of comparison of knee stability and clinical outcome between the two groups are summarized in Table 2.
In second-look arthroscopy, there was no significant difference (p > 0.05) in the degree of synovium coverage between the two groups (group A: 18 good cases, 6 half cases, and 1 pale case; group H: 17 good cases, 7 half cases, and 1 pale case). There was no complete discontinuity of the ACL graft on diagnostic arthroscopy in either group. There was no cyclops-like mass at the second-look arthroscopy in either group.
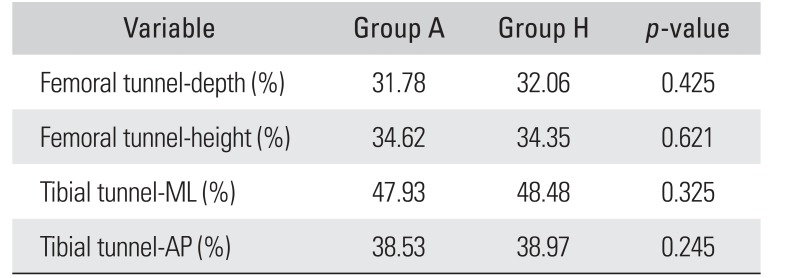
In group A, the center of the femoral tunnel was located at 31.78% in the shallow/deep direction along the Blumensaat's line and at 34.62% in the high/low direction from the intercondylar roof. The center of the tibial tunnel was located at 38.53% of the distance from the anterior edge of the tibia in the anteroposterior direction and at 47.93% in the mediolateral direction. In group H, the center of the femoral tunnel was located at 32.06% in the shallow/deep direction along the Blumensaat's line and at 34.35% in the high/low direction from the intercondylar roof. The center of the tibial tunnel was located at 38.97% of the distance from the anterior edge of the tibia in the anteroposterior direction and at 48.48% in the mediolateral direction. There was no significant difference in the femoral or tibial tunnel location between the two groups (p > 0.05). Results are summarized in Table 3.
The principal finding of this study was that tibialis allograft with a remnant preservation technique was a good surgical option with good clinical results. Tunnel malposition and cyclops lesions are known disadvantages of the remnant preservation technique. However, according to results of this study, there was no significant difference in femoral or tibial tunnel location between the two groups. No cyclops-like mass was seen during second-look arthroscopy in either group.
Operative treatment of the ACL-deficient knee in all age groups now has strong support in the literature. However, there are still many debates over the selection of which graft material to use for ACLR in any age group.11) A number of clinical studies and meta-analyses have shown significant differences that favor autografts over allografts. Li et al.12) have shown that, after ACLR, autograft tissue appears to mature faster than allograft tissue on magnetic resonance imaging. On the other hand, several studies have found no significant difference between autografts and allografts.13) For instance, Sun et al.14) conducted a long-term randomized controlled trial comparing quadrupled hamstring tendon autografts and fresh-frozen hamstring allografts. After a mean follow-up period of 7.8 years, there was no significant difference in IKDC, Lysholm, Cincinnati score, or Tegner score between the two graft types. Although the question of allograft versus autograft for reconstruction of the ACL is a heavily debated topic among orthopedic surgeons, few research studies have compared the clinical benefit of using a remnantpreserving technique with a tibialis allograft or a hamstring autograft. When the use of an autograft tendon is not feasible for various reasons, we are compelled to use an allograft tendon. Under such a circumstance, the remnantpreserving technique would help early graft incorporation and graft synovialization, ultimately leading to good clinical outcomes without graft failure. In this study, the stability and function of the knee were compared between ACLR performed with the tibialis allograft using the remnant-preserving technique and ACLR with the hamstring autograft. Our results support our hypotheses. There was no significant difference in clinical outcomes, stability, or degree of synovial coverage between the two groups. According to Yoo et al.,3) although both hamstring autografts and tibialis allografts used in ACLR provided good clinical and radiological outcomes, the second-look arthroscopy revealed that the hamstring autograft produced better synovial coverage than the tibialis allograft. In their study, there was no mention about whether the remnant tissue was preserved.
Our study has some limitations. First, this study was retrospective in nature with a relatively small patient number. Second, patient selection was performed in a non-randomized pattern in both groups. To minimize the effect of selection bias, two groups were matched with respect to preoperative features and findings.4) However, they were not perfectly matched in design. Third, we could not completely rule out the possibility of graft failure in patients who were lost during follow-up.
If an autograft tendon is not feasible in ACLR, a remnant-preserving technique with a tibialis allograft can be a viable option. In this study, the outcomes of remnant-preserving ACLR using a tibialis allograft were comparable to remnant-sacrificing ACLR using a hamstring autograft.
References
1. Cvetanovich GL, Mascarenhas R, Saccomanno MF, et al. Hamstring autograft versus soft-tissue allograft in anterior cruciate ligament reconstruction: a systematic review and meta-analysis of randomized controlled trials. Arthroscopy. 2014; 30(12):1616–1624. PMID: 25108904.

2. Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS. Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ. 2006; 332(7548):995–1001. PMID: 16603564.

3. Yoo SH, Song EK, Shin YR, Kim SK, Seon JK. Comparison of clinical outcomes and second-look arthroscopic findings after ACL reconstruction using a hamstring autograft or a tibialis allograft. Knee Surg Sports Traumatol Arthrosc. 2017; 25(4):1290–1297. PMID: 26718638.

4. Mardani-Kivi M, Karimi-Mobarakeh M, Keyhani S, Saheb-Ekhtiari K, Hashemi-Motlagh K, Sarvi A. Hamstring tendon autograft versus fresh-frozen tibialis posterior allograft in primary arthroscopic anterior cruciate ligament reconstruction: a retrospective cohort study with three to six years follow-up. Int Orthop. 2016; 40(9):1905–1911. PMID: 26987981.
5. Carey JL, Dunn WR, Dahm DL, Zeger SL, Spindler KP. A systematic review of anterior cruciate ligament reconstruction with autograft compared with allograft. J Bone Joint Surg Am. 2009; 91(9):2242–2250. PMID: 19724004.

6. Leo BM, Krill M, Barksdale L, Alvarez-Pinzon AM. Failure rate and clinical outcomes of anterior cruciate ligament reconstruction using autograft hamstring versus a hybrid graft. Arthroscopy. 2016; 32(11):2357–2363. PMID: 27286700.

7. Ahn JH, Wang JH, Lee YS, Kim JG, Kang JH, Koh KH. Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: clinical and magnetic resonance imaging results. Arthroscopy. 2011; 27(8):1079–1089. PMID: 21704468.

8. Ko YW, Rhee SJ, Kim IW, Yoo JD. The correlation of tunnel position, orientation and tunnel enlargement in outside-in single-bundle anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2015; 27(4):247–254. PMID: 26672479.

9. Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL: radiographic quadrant method. Am J Knee Surg. 1997; 10(1):14–21. PMID: 9051173.
10. Tsuda E, Ishibashi Y, Fukuda A, Yamamoto Y, Tsukada H, Ono S. Tunnel position and relationship to postoperative knee laxity after double-bundle anterior cruciate ligament reconstruction with a transtibial technique. Am J Sports Med. 2010; 38(4):698–706. PMID: 20139333.

11. Barrett G, Stokes D, White M. Anterior cruciate ligament reconstruction in patients older than 40 years: allograft versus autograft patellar tendon. Am J Sports Med. 2005; 33(10):1505–1512. PMID: 16009990.
12. Li H, Tao H, Cho S, Chen S, Yao Z, Chen S. Difference in graft maturity of the reconstructed anterior cruciate ligament 2 years postoperatively: a comparison between auto-grafts and allografts in young men using clinical and 3.0-T magnetic resonance imaging evaluation. Am J Sports Med. 2012; 40(7):1519–1526. PMID: 22495290.
13. Mascarenhas R, Erickson BJ, Sayegh ET, et al. Is there a higher failure rate of allografts compared with autografts in anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Arthroscopy. 2015; 31(2):364–372. PMID: 25220350.
14. Sun K, Zhang J, Wang Y, et al. Arthroscopic reconstruction of the anterior cruciate ligament with hamstring tendon autograft and fresh-frozen allograft: a prospective, randomized controlled study. Am J Sports Med. 2011; 39(7):1430–1438. PMID: 21441418.
Fig. 1
A suture hook with Maxon monofilament absorbable suture was inserted through the anteromedial portal and passed through the remnant anterior cruciate ligament tissue.
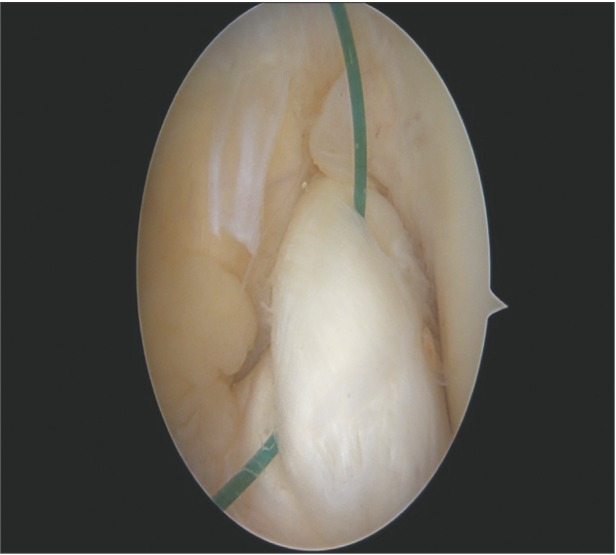
Fig. 2
Two or three more stitches of the remnant anterior cruciate ligament tissue were performed and pulled out through the anterior portal.
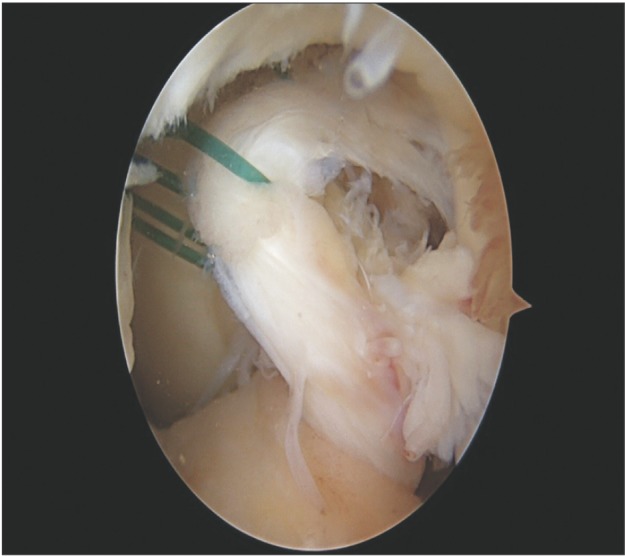
Fig. 3
After confirmation of the graft passage, the suture was tied with a TightRope device over the button. Then, the sutures were tied with each other.
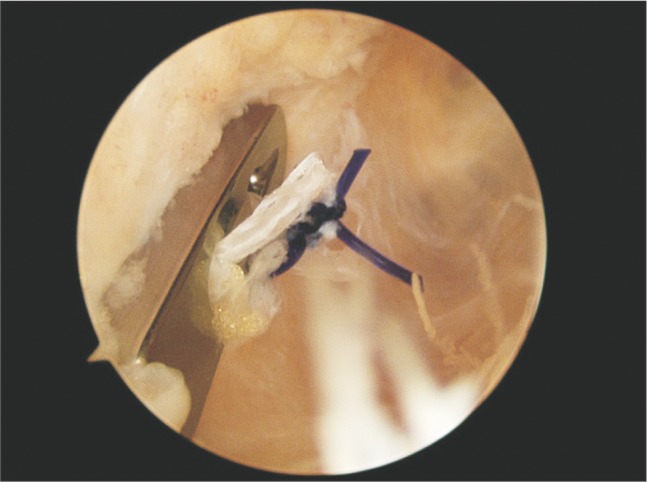
Fig. 4
(A) Synovial coverage less than 50%. (B) Synovial coverage more than 50%. (C) Nearly entire synovial coverage.
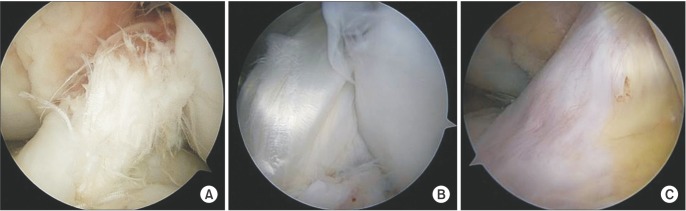
Fig. 5
The location of the femoral tunnel was calculated as a percentage of the distance from the most posterior contour with respect to the total length of the lateral condyle parallel to the Blumensaat's line and a percentage of the distance from the intercondylar roof with respect to the total depth of the intercondylar notch perpendicular to the Blumensaat's line. H: perpendicular to the Blumensaat's line, D: parallel to the Blumensaat's line.
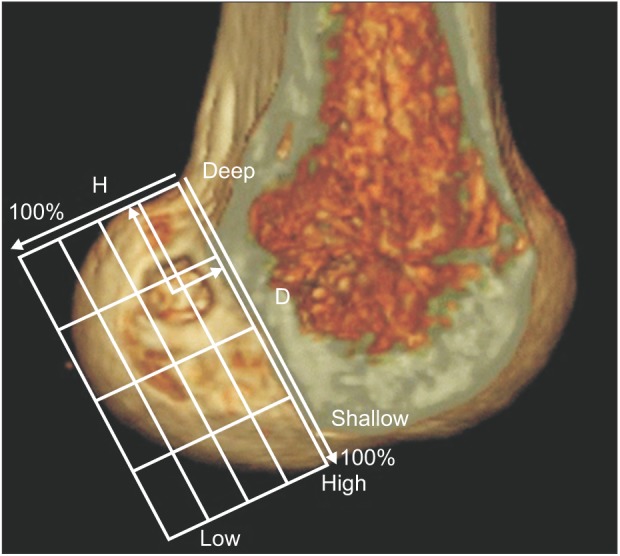
Fig. 6
The location of the tibial tunnel was calculated as a percentage of the distance from the most medial contour with respect to the mediolateral (ML) width of the tibial plateau and a percentage of the distance from the most anterior contour with respect to the anteroposterior (AP) length of the tibial plateau.
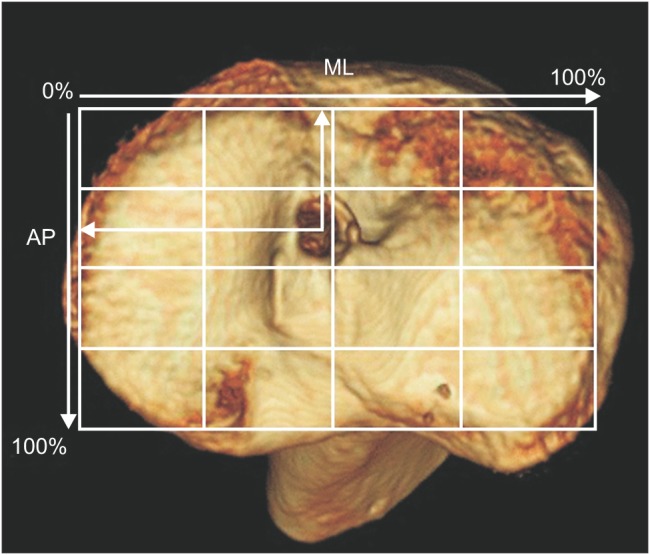
Table 1
Comparison of Demographic Data between Two Groups
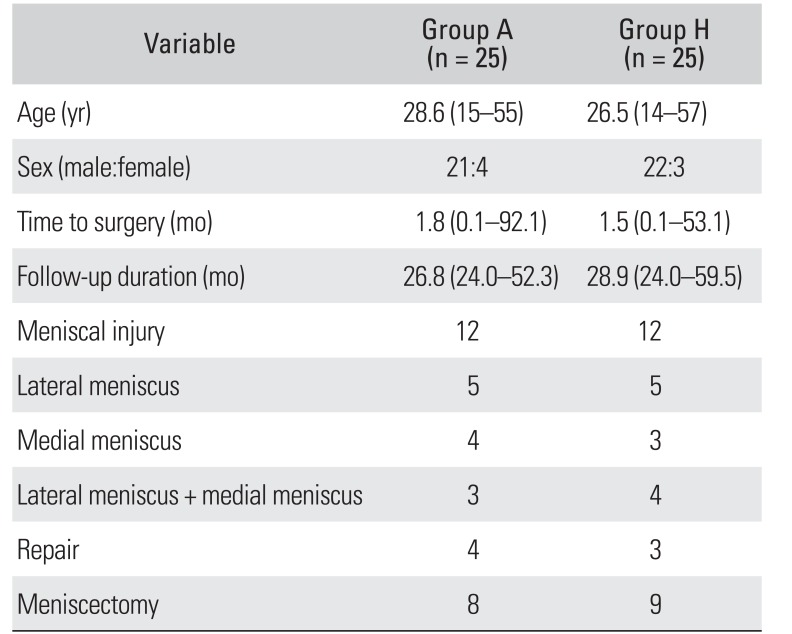
Table 2
Comparison of Clinical Outcomes between Two Groups




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download