Abstract
Background
The purpose of this study was to evaluate factors associated with the risk of articular surface perforation during anchor placement for arthroscopic acetabular labral repair using follow-up computed tomographic arthrography (CTA).
Methods
Forty-six patients (29 males and 17 females) underwent arthroscopic labral repair using 142 suture anchors (55 large anchors and 87 small anchors). The patients were followed with CTA 1 year postoperatively. Anchor position was assessed by the insertion angle and the distance of the suture anchor tip from the articular cartilage. The incidence of malposition of suture anchors was assessed in follow-up CTA. The location and incidence of malposition were compared between two groups divided according to the diameter of suture anchor.
Results
The mean insertion angle and distance were significantly different between the groups. Of the 142 anchors, 15 (11%) were placed in the cartilage-bone transitional zone. Articular involvement was most common at the 3 o'clock position of the suture anchor (six out of 33 anchors, 18.2%). Both the insertion angle and distance showed small values in the articular involvement group.
Hip arthroscopy is a growing field in sports medicine, with femoroacetabular impingement and labral tears being common indications for surgery. Excellent clinical results have been reported in the literature for both labral debridement and repair. However, superior functional outcomes have been shown with labral repair.1234) The acetabular labrum in a normal hip joint comprises 22% of the surface area and 33% of the total volume. It provides a seal that helps maintain synovial fluid pressure, which contributes to joint stability, lubrication, and protection of the cartilage.56) Accordingly, hip arthroscopy for repair of the labrum is gaining popularity.
Several techniques for labral repair have been described in the literature, including loop fixation techniques and labral base techniques.789) Both techniques involve placement of a suture anchor in the acetabular rim to provide an anatomic fixation. One technical error associated with anchor placement is inadvertent articular cartilage penetration with a drill or an anchor during labral repair.10) Several anatomical studies have attempted to identify the safe angle for anchor placement in different regions of the acetabulum or to modify the portals to create a better angle for anchor placement.11121314)
The purpose of this study was to evaluate factors associated with the risk of articular surface perforation during anchor placement for arthroscopic acetabular labral repair using follow-up computed tomographic arthrography (CTA).
The design and protocol of this retrospective study were approved by the Institutional Review Board of Chung-Ang University Hospital (IRB No. C2016133-1876) and performed in accordance with the principles of the Declaration of Helsinki. Informed consent was waived. We performed arthroscopic labral repair on 200 patients between January 2011 and December 2014. Of those, 46 patients (29 males and 17 females) who underwent 1-year follow-up CTA were enrolled in our study.
Arthroscopic labral repair was performed using 142 anchor sutures in the 46 patients. The patients were divided into two (a large anchor group and a small anchor group) according to the diameter of the suture anchor used. Fifty-five anchors (larger than 2.3 mm) were used in the large anchor group and 87 anchors (smaller than 1.4 mm) were used in the small anchor group. After conducting a radiological analysis of postoperative CTA results, the patients were also subdivided into an articular involvement group and a non-involvement group.
One senior surgeon (YCH) repaired 46 acetabular labral tears in 46 hips with femoroplasty in 21 hips and acetabuloplasty in 18 hips. Hip arthroscopy was performed with the patient positioned in the supine position on a standard fracture table. Traction was applied with slight extension and adduction of the hip joint using sufficient force to open the joint approximately 1 cm. Two or three portals (anterolateral, anterior, and/or posterolateral) were placed for treatment of femoroacetabular impingement including arthroscopic labral repair. After assessing the amount of bone overhang, the pincer lesion was resected, or rim trimming was accomplished using a 5.5-mm round burr. The amount of bone resected depended on the extent of overhang. After resecting the pincer lesion, the single loop technique was used in a small labrum (less than 6 mm in height). In a large labrum (more than 6 mm in height), the labral base refixation technique was used. Arthro-Pierce (Smith & Nephew, Andover, MA, USA) was used to pierce the labrum, and a stiff, nonabsorbable suture was passed through the base of the labrum. PEEK standard anchors (2.3-mm Bioraptor or 2.9-mm Bioraptor knotless suture anchor; Smith & Nephew) or all-suture type soft anchors (1.3-mm Y-Knot [ConMed Linvatec, Largo, FL, USA] or 1.4-mm JuggerKnot [BIOMET, Warsaw, IN, USA] suture anchors) were placed on the capsular side (Fig. 1). These were secured with a straight drill guide. Then, using a suture passer, a suture limb was passed through a small portion of the labral substance. An arthroscopic sliding knot was made and passed down through the cannula to secure the repair. Two to four anchors were placed at the superior (12 o'clock), anterosuperior (1–2 o'clock), and anterior (3 o'clock) positions. Anchors fixed in other locations were excluded from this study.
Next, traction was released and the hip was flexed 45°, allowing passage of the camera along the femoral head-neck junction into the peripheral space. The femoral head-neck junction and lateral epiphyseal vessels were visualized during this maneuver. Instruments were placed into the peripheral compartment through the anterolateral or distal lateral accessory portal. After confirming a cam lesion, which was defined by local abnormalities and dynamic examination, bumpectomy was performed to restore the femoral head-neck offset by transforming the convex lesion into a concave surface.15) The operation was completed with joint lavage and injection of a local anesthetic.
Standardized CTA was performed preoperatively in all patients, and follow-up CTA was recommended 1 year after surgery. All measurements were performed with a picture archiving and communication system (M view; Infinitt, Seoul, Korea).
Coronal, axial, and sagittal reconstruction was created (Fig. 2A). Two musculoskeletal radiologists independently measured the radiographic parameters. The interobserver reliability showed a high level of agreement (0.87) on separate measurements of the lateral center edge angle (LCEA) and the calculated correlation. LCEA values were measured on coronal images (Fig. 2B). Using sagittal images, we classified anchor locations as superior (12 o'clock), anterosuperior (1–2 o'clock), or anterior (3 o'clock). The location of each anchor was determined on the coronal and axial computed tomography (CT) scout images (Fig. 2C).
The insertion angle was measured by extending a line 15 mm from the insertion point to the acetabular cartilage as described by Lertwanich et al.12) and drawing another line from the insertion point through the anchor (Fig. 3A). The minimum distance between the anchor/drill hole and the articular surface of the acetabulum was then measured (Fig. 3B). The angle of anchor insertion was measured at the superior and anterosuperior positions on the coronal images, and the distance between the anchor/drill hole and the articular surface of the acetabulum for the superior and anterosuperior anchors was also measured. Anchors in the anterior position had the same measurements taken on the axial images. The articular surface was considered to be involved in cases in which the suture anchor was located in the cartilage-bone transitional zone on sagittal images (white arrow in Fig. 3C), and such cases were assigned to the articular involvement group (Fig. 3C).
Both musculoskeletal radiologists evaluated the CTA findings and consensus was achieved for any discrepancies. We assessed inter- and intraobserver reliability of the measured parameters, including the LCEA, insertion angle, and distance using Kappa coefficients. Reliability was classified as follows: 0, poor; 0–0.20, slight; 0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, substantial; and greater than 0.80, almost perfect agreement.16)
The Student t-test was used to detect any differences in the insertion angle and distance between the articular involvement group and the non-involvement group. The chi-square test was used to compare categorical variables such as gender and suture anchor type.
IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA) was used for all analyses and a significant difference was defined as p < 0.05. All data is presented as the mean and standard deviation.
The study subjects included 29 males and 17 females with a mean age of 32.7 ± 9.5 years and a mean body mass index of 23.0 ± 4.2 kg/m2. The mean LCEA angle was 29.6° ± 5.3°. Of a total of 142 anchors, 55 were PEEK standard anchors and 87 were all-suture anchors. Twenty-eight anchors were located at the 12 o'clock position, 81 at the 1–2 o'clock positions, and 33 at the 3 o'clock position. Fifteen anchors (10.6%) were placed in the cartilage-bone transitional zone (Table 1).
On the radiological analysis of the 142 anchors, the mean LCEA angles of the PEEK standard anchor group (large anchor group) and the all-suture anchor group (small anchor group) were 29.1° ± 6.8° and 29.9° ± 4.0°, respectively (p = 0.372). The mean insertion angles of the PEEK standard anchor group and all-suture anchor group at the 12 o'clock position were 20.7° ± 2.8° and 25.0° ± 5.6°, respectively (p = 0.022). The mean angle of insertion at the 3 o'clock position was 17.6° ± 4.6° for the PEEK standard anchor group and 26.2° ± 7.4° for the all-suture anchor group (p = 0.002). There was no significant difference in the insertion angle at the 1–2 o'clock positions between the two groups (p = 0.757) (Table 2). The mean distance to the articular cartilage at the 12 o'clock position was 5.8 ± 1.1 mm for the PEEK standard anchor group and 6.9 ± 1.8 mm for the all-suture anchor group (p = 0.029). The mean distance to articular cartilage at the 1–2 o'clock position was 5.9 ± 1.8 mm for the PEEK standard anchor group and 6.6 ± 1.9 mm for the all-suture anchor group (p = 0.038). However, the distance between the two groups at the 3 o'clock position was not statistically significantly different (p = 0.158) (Table 3).
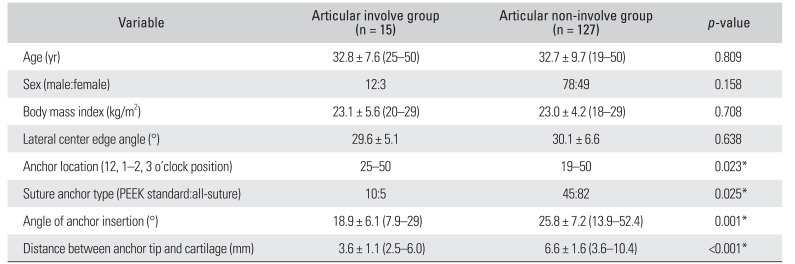
On the subgroup analysis of the articular involvement group and non-involvement group, there was no notable difference in age (p = 0.809), sex (p = 0.158), body mass index (p = 0.708), and LCEA (p = 0.638). However, the anchor location (p = 0.023), anchor type (p = 0.025), insertion angle (p = 0.001), and distance (p < 0.001) were significantly different between the two groups.
Articular involvement was noted in six out of 33 anchors (18.2%) located at the 3 o'clock position and in nine out of 81 anchors (11.1%) located at the 1–2 o'clock position. However, articular involvement was not observed for 28 anchors located at the 12 o'clock position. The incidence of articular involvement was higher in the PEEK standard anchor group (10 out of 55, 18.2%) than in the all-suture anchor group (5 out of 87, 5.7%). Both insertion angle and distance showed small values in the articular involvement group (Table 4).
Intraobserver reliability for each observer was moderate (kappa, 0.763 and 0.722, respectively). Interobserver correlation of CTA findings was also moderate (kappa, 0.702).
The goal of any successful acetabular labral repair procedure is stable fixation without complications. Several anatomic and cadaver studies have attempted to suggest safe angles for acetabular labral repair.11) However, there has been no report regarding the prevalence of malposition of anchors during labral repair. In this study, using CTA, we observed that 15 of 142 anchors (11%) were placed in the cartilage-bone transitional zone. Anchors placed at the 3 o'clock position were more frequently located in the cartilage-bone transitional zone. Larger-diameter (≥ 2.3 mm) PEEK standard anchors were more frequently located in the cartilage-bone transitional zone than were smallerdiameter (≤ 1.4 mm) all-suture anchors.
Several anatomic studies have reported different safety angles according to acetabular location. In particular, the 3 o'clock position in the acetabulum has been described as a high-risk area for cartilage damage. In this study, suture anchors at the 3 o'clock position had the highest likelihood of being located in the cartilage-bone transitional zone (18.2%, 6/33 anchors).
Hernandez and McGrath11) performed an anatomic study of safe suture angle with three different suture anchor systems using nine human cadavers. They found that the maximal angle of insertion at the anterior rim location was the narrowest among three acetabular locations studied. Foster et al.17) reported similar findings in a study on six cadavers. They found a smaller distance from the articular surface when using a more anterior position, and showed a very small distance at 4 o'clock. Our findings correspond well with their results. We found that suture anchors at the anterior (3 o'clock) position had a significantly lower insertion angle compared with those at the superior (12 o'clock) and anterosuperior (1–2 o'clock) positions. Therefore, when placing anchors at the 3 o'clock position, care should be taken to avoid articular injury during arthroscopic procedures.
Theoretically, large-diameter suture anchors are more prone to penetrate the cartilage or the cartilage-bone transitional zone. We found that larger-diameter (≥ 2.3 mm) PEEK standard anchors were indeed more frequently located in the cartilage-bone transitional zone than were smaller-diameter (≤ 1.4 mm) sutures. Hernandez and McGrath11) reported similar findings. They found that 2.4-mm anchors were inserted at a significantly greater maximal angle than were 3.0-mm anchors (p = 0.04). They also noted especially small widths at the level of the labral insertion (less than 3 mm) at the anterior location, and suggested using drills of < 3.0 mm for anchor insertion if the labral attachment was used as the starting point. They suggested that using an anchor larger than 3.0 mm would be more likely to cause articular damage.
To prevent articular damage during placement of suture anchors, several methods can be considered. First, small-diameter suture anchors could be used to minimize cartilage damage. Second, a change in portal placement can increase safety. Stanton and Banffy18) evaluated the distance from the articular surface according to portal placement using six cadavers. They analyzed the three common portals: distal anterolateral accessory (DALA), mid-anterior (MA), and anterolateral (AL) portals, and reported that the DALA portal produced a larger distance from the articular surface and was safer than were the other portals. At a depth of 15 mm, the average distance from the articular surface in the anterior position (MA portal), the superior position (AL portal), and the anterior position (DALA portal) was 5.26, 3.41, and 8.01 mm, respectively. Third, trimming of the acetabular rim can produce a safer angle. Hernandez and McGrath11) measured the width of the acetabular bone at the point of labral insertion as well as at depths of 5, 10, 15, and 20 mm from the labral insertion point at the 12 o'clock, 1:30, and 3 o'clock positions in nine human cadavers. They found the 3 o'clock position to be significantly wider at deeper (15 and 20 mm) points. Suture anchor placement done at the 3 o'clock position is associated with a narrow insertion angle and small articular distance. We recommend widening of the safety angle with trimming of the acetabular rim and use of an accessory portal such as the DALA portal, especially for suture anchor placement done at the 3 o'clock position. In all-suture type anchors, the use of a curved guide, flexible drill, and flexible suture anchor inserter may provide more precise placement in the acetabular rim at the 3 o'clock position. Nho et al.13) performed a cadaver study that compared suture anchor placement in the acetabular rim using straight versus curved drill guides, and measured the insertion angle and distance of the suture anchor during labral refixation. The curved suture anchor guide significantly increased the insertion angle (p = 0.009) and the distance from the articular cartilage to the anchor (p = 0.003). In addition, the use of a curved guide, flexible drill, and flexible suture anchor inserter could allow for placement of suture anchors without changing anchor placement position in the acetabular rim.1317)
This study had several limitations. First, it was a retrospective small case series. Second, we did not analyze the clinical results and complications according to anchor type. All-suture type anchors have a lower probability of articular involvement and a wider margin of safety angle. However, there are doubts about their strength and durability. Therefore, further research on the clinical and imaging results according to anchor type is necessary. Finally, there is a concern about radiation dose in studies using CT. However, in our study, the radiation dose ranged from 2.55 to 7.75 mSv, which is not higher than that given during acute abdominal CT (usually from 5 to 8 mSv) and is lower than that used for obstetric-gynecological pelvic CT (10 to 16 mSv).192021)
The radiographic analysis of the placement of suture anchors after arthroscopic labral refixation using follow-up CTA demonstrates that articular involvement is related to the location on the acetabular rim (clock position) and diameter of the suture anchor.
References
1. Haddad B, Konan S, Haddad FS. Debridement versus re-attachment of acetabular labral tears: a review of the literature and quantitative analysis. Bone Joint J. 2014; 96-B(1):24–30. PMID: 24395306.
2. Krych AJ, Kuzma SA, Kovachevich R, Hudgens JL, Stuart MJ, Levy BA. Modest mid-term outcomes after isolated arthroscopic debridement of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc. 2014; 22(4):763–767. PMID: 24493256.

3. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009; 25(4):369–376. PMID: 19341923.

4. Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009; 91(1):16–23. PMID: 19091999.
5. Crawford MJ, Dy CJ, Alexander JW, et al. The 2007 Frank Stinchfield Award: the biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007; 465:16–22. PMID: 17906586.

6. Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003; 36(2):171–178. PMID: 12547354.

7. Jackson TJ, Hammarstedt JE, Vemula SP, Domb BG. Acetabular labral base repair versus circumferential suture repair: a matched-paired comparison of clinical outcomes. Arthroscopy. 2015; 31(9):1716–1721. PMID: 25911393.

8. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005; 21(12):1496–1504. PMID: 16376242.

9. Philippon MJ, Schroder e Souza BG, Briggs KK. Labrum: resection, repair and reconstruction sports medicine and arthroscopy review. Sports Med Arthrosc. 2010; 18(2):76–82. PMID: 20473125.

10. Matsuda DK, Bharam S, White BJ, Matsuda NA, Safran M. Anchor-induced chondral damage in the hip. J Hip Preserv Surg. 2015; 2(1):56–64. PMID: 27011815.

11. Hernandez JD, McGrath BE. Safe angle for suture anchor insertion during acetabular labral repair. Arthroscopy. 2008; 24(12):1390–1394. PMID: 19038710.

12. Lertwanich P, Ejnisman L, Torry MR, Giphart JE, Philippon MJ. Defining a safety margin for labral suture anchor insertion using the acetabular rim angle. Am J Sports Med. 2011; 39(Suppl):111S–116S. PMID: 21709040.

13. Nho SJ, Freedman RL, Federer AE, et al. Computed tomographic analysis of curved and straight guides for placement of suture anchors for acetabular labral refixation. Arthroscopy. 2013; 29(10):1623–1627. PMID: 24075612.

14. Thomas Byrd JW. Modified anterior portal for hip arthroscopy. Arthrosc Tech. 2013; 2(4):e337–e339. PMID: 24400178.

15. Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007; 35(9):1571–1580. PMID: 17420508.
16. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33(1):159–174. PMID: 843571.

17. Foster AD, Ryan J, Ellis T, Flom J. Safe suture anchor insertion for anterior and posterior hip labral repair. J Hip Preserv Surg. 2015; 2(2):170–174. PMID: 27011835.

18. Stanton M, Banffy M. Safe angle of anchor insertion for labral repair during hip arthroscopy. Arthroscopy. 2016; 32(9):1793–1797. PMID: 27132777.

19. Ha YC, Choi JA, Lee YK, et al. The diagnostic value of direct CT arthrography using MDCT in the evaluation of acetabular labral tear: with arthroscopic correlation. Skeletal Radiol. 2013; 42(5):681–688. PMID: 23073899.

20. Jung JY, Kim GU, Lee HJ, Jang EC, Song IS, Ha YC. Diagnostic value of ultrasound and computed tomographic arthrography in diagnosing anterosuperior acetabular labral tears. Arthroscopy. 2013; 29(11):1769–1776. PMID: 24071389.
21. Yoo JI, Ha YC, Lee YK, Lee GY, Yoo MJ, Koo KH. Morphologic changes and outcomes after arthroscopic acetabular labral repair evaluated using postoperative computed tomography arthrography. Arthroscopy. 2017; 33(2):337–345. PMID: 27876489.

Fig. 1
PEEK standard anchors: 2.3-mm Bioraptor suture anchor (Smith & Nephew, Andover, MA, USA) (A) and 2.9-mm Bioraptor knotless suture anchor (Smith & Nephew) (B). All-suture type soft anchors: 1.3-mm Y-Knot (ConMed Linvatec, Largo, FL, USA) (C) and 1.4-mm JuggerKnot (BIOMET, Warsaw, IN, USA) (D).
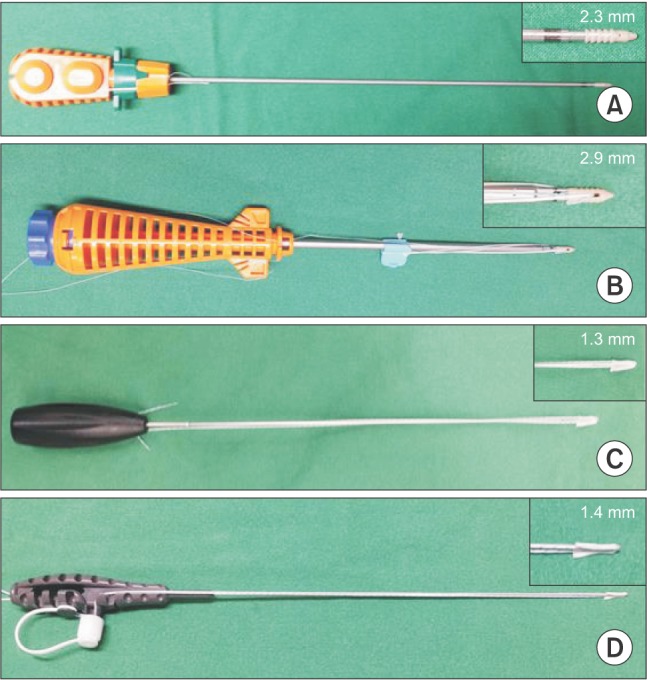
Fig. 2
Radiological measurements. (A) Coronal, axial, and sagittal computed tomographic arthrography reconstruction. (B) Lateral center edge angle (LCEA: the angle formed by a vertical line and a line connecting the center of the femoral head with the lateral edge of the acetabulum). (C) Location of each anchor according to the clock position.

Fig. 3
Parameters assessed using computed tomographic arthrography. (A) Insertion angle of the suture anchor (yellow arrow). It was measured by extending a line 15 mm from the insertion point to the acetabular cartilage and drawing a second line through the anchor. (B) Distance from the tip of the suture anchor (yellow arrow). It was measured as the minimum distance between the anchor/drill hole and the articular surface of the acetabulum. (C) Malposition of suture anchors at the cartilage-bone transitional zone (white arrow).
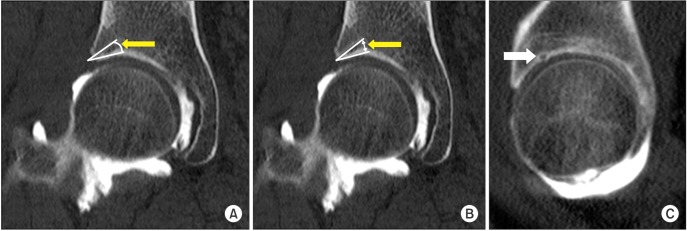
Table 1
Patient Demographic Data
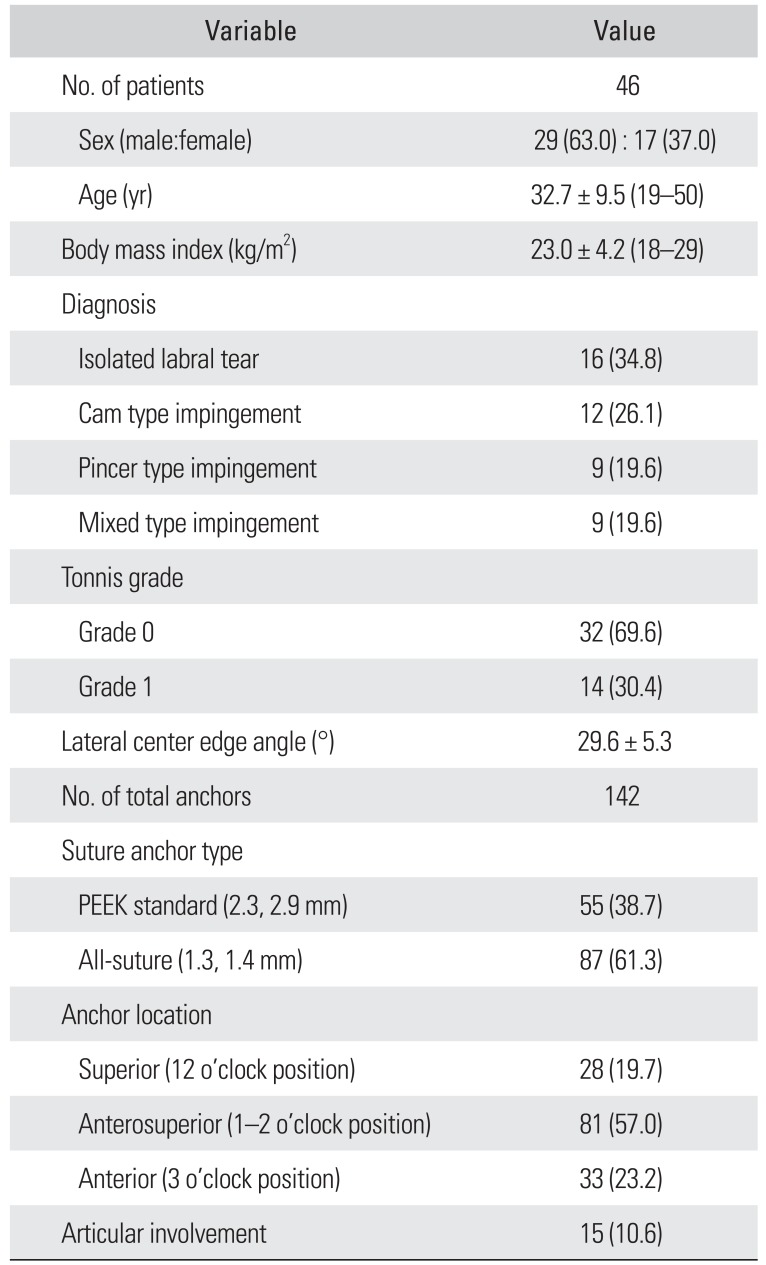
Table 2
Angle of Anchor Insertion
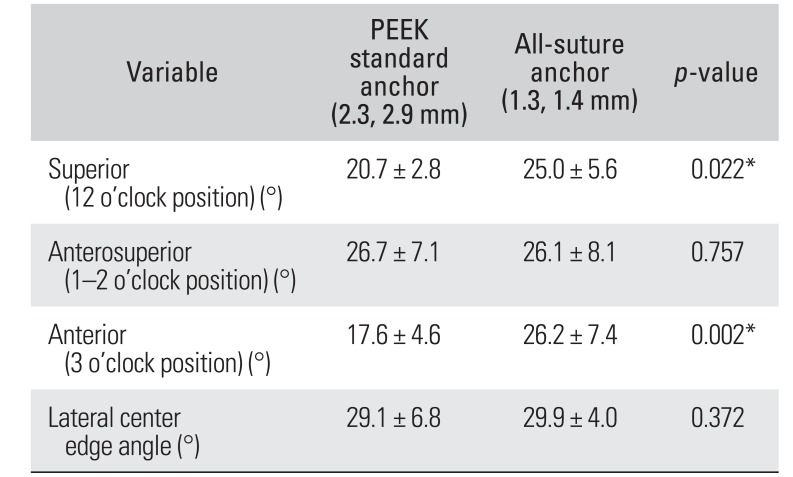
Table 3
Distance between Anchor Tip and Articular Cartilage
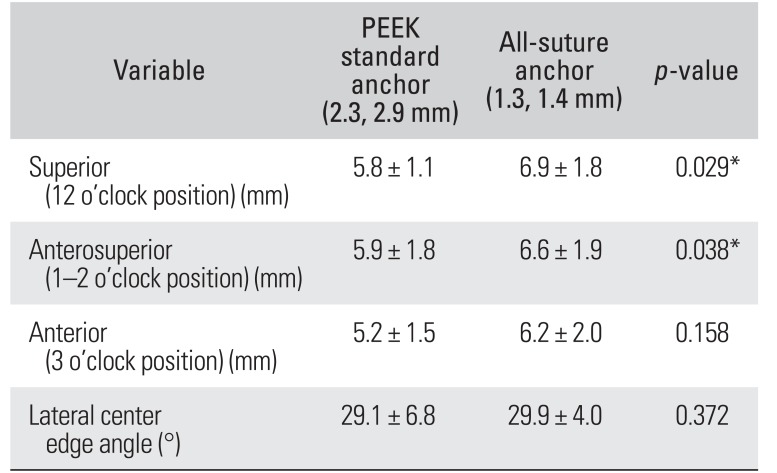
Table 4
Comparisons of Variables According to the Presence of Articular Involvement




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download