Abstract
Background
In a previous study, we reported clinical and radiographic results of our modified Salter innominate osteotomy technique in 16 hips affected by Legg-Calvé-Perthes disease (LCPD) with an average follow-up of 31.8 months. In this study, we present the long-term results of the osteotomy in LCPD patients followed until physeal closure.
Methods
Thirty hips of 29 patients were followed until skeletal maturation after modified Salter innominate osteotomy. The mean follow-up duration was 12.9 years (range, 9.1 to 16.0 years). Eleven hips (36.7%) were classified as Catterall group III and 19 (63.3%) as Catterall group VI. Stable interposition of a bone block was achieved using one biodegradable screw in nine hips and without any fixation device in 21 hips by simply changing the direction of osteotomy. The Harris Hip Score (HHS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, and hip function were evaluated at the last follow-up. Radiological outcomes were evaluated using Wiberg's center-edge angle, the Mose method, and Stulberg classification, and osteoarthritic changes were evaluated using the Tonnis classification.
Results
Mean HHS and WOMAC score were 80.2 points and 54 points, respectively, preoperatively and these were improved to 96.2 points and 28 points, respectively, at the last follow-up. Clinical results, according to Robinson's criteria, were good in 18, fair in seven, and poor in five hips. Radiological results assessed using the Mose method were good in 18, fair in six, and poor in six hips, and according to the Stulberg classification, nine hips were class I, nine were class II, eight were class III, and four were class IV. The mean center-edge angle improved from 19.7° preoperatively to 29.6° at the final follow-up. According the Tonnis classification, three hips were grade 2, five were grade 1, and 22 were grade 0. Of the three grade 2 hips, two underwent Chiari osteotomy 12.1 and 8.8 years postoperatively, and the other underwent total hip arthroplasty 12.9 years postoperatively.
Legg-Calvé-Perthes disease (LCPD) is caused by an insidious circulation problem of the femoral head that usually results in collapse of the femoral head followed by secondary degenerative changes. LCPD usually results in pain and range of motion (ROM) limitations. In 1957, Salter first performed the innominate osteotomy to reduce congenital dislocation or subluxation of the hip. In 1962, based on his experimental investigations on a porcine model of LCPD, he began to apply the principle of innominate osteotomy to the subluxation associated with more severe forms of the disease.1) Salter innominate osteotomy (SIO) was used in special LCPD cases, for example, for lengthening or shortening extremities.234) However, its usage was limited because of technical difficulties as compared with the original SIO. SIO forms a horizontal line from the sciatic notch to the anterior inferior iliac spine at a right angle to the vertical axis of the ilium. Then, fixation of an inserted full-thickness triangular bone fragment is necessary. In 2003, we reported our modified SIO technique. Instead of performing an osteotomy from the sciatic notch to the anterior inferior iliac spine in one straight line, we made two plane osteotomy lines. The posterior half of the ilium from the sciatic notch was cut in the same manner as in SIO, but the anterior half was osteotomized using a reciprocal saw at 45° oblique to the coronal plane and 30° to 40° posteroinferior to the sagittal plane. It allows for tight and stable insertion of a triangular fragment without additional fixation.
In a previous study, we had evaluated the clinical and radiographic results of our modified SIO technique in 16 LCPD hips.5) The present study was undertaken to evaluate the long-term results of this modified SIO technique in LCPD patients followed until physeal closure.
Between February 1998 and September 2001, we used the modified SIO in 33 hips of 32 patients of Catterall2) group III or IV.5) Three of the 32 patients were not able to be followed until skeletal maturation and thus were excluded from this study. Therefore, the study group consisted of 30 hips of 29 patients (24 males and five females). Their mean age at the time of surgery was 7.1 years (range, 4.3 to 11.0 years) and the mean follow-up was 12.9 years (range, 9.1 to 16.0 years). The indications for the modified SIO were involvement of more than half of the femoral head (Catterall groups III and IV) and loss of containment of the femoral head. A bioscrew was used to fixate the bone fragment after modified SIO in nine hips, but 21 hips received no additional fixation. Iliopsoas tenotomy was performed in 25 hips for flexion contractures of more than 30° and adductor tenotomy was performed in two hips with hip abduction of less than 30°. Catterall2) and Herring6) classifications were used to assess the extent of femoral head involvement in all hips. Eleven hips (36.7%) were classified as Catterall group III, and 19 (63.3%) as group IV. Four hips (13.3%) were classified as Herring group A, 10 (33.3%) as group B, and 16 (53.3%) as group C (Table 1).
Clinical assessment at the final follow-up was conducted using the Harris Hip Score (HHS)7) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score.8) In addition, the ability to perform other hip positions common assumed among Asians, such as squatting and sitting on the floor, and the Buddhist position, were also evaluated. We also assessed results using the criteria suggested by Robinson et al.,9) according to which a result is considered good when the hip demonstrates a normal ROM and the patient is symptom-free, fair when hip movement (especially internal rotation) is slightly limited and the patient has no symptoms, or poor when hip movement is significantly limited and pain is experienced at rest or after physical activity. A limited ROM of the hip was defined as < 20° in abduction and internal rotation or < 100° in flexion and a side-to-side difference of ≥ 10° in abduction or ≥ 30° in flexion.10)
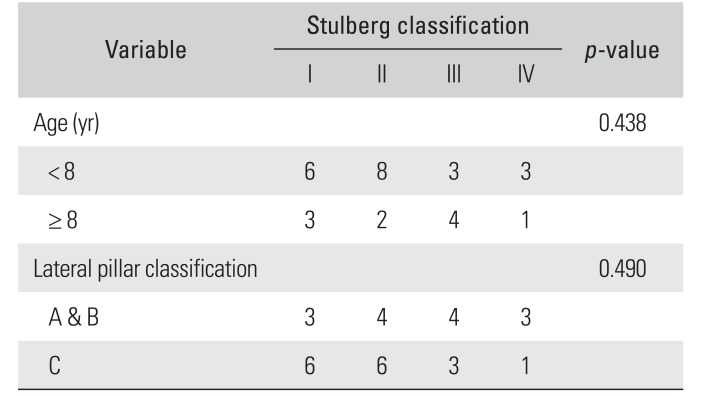
Preoperative and final radiographs were assessed by two orthopedic surgeons (SHL and HYY) using Wiberg's center-edge angle,11) the Mose method,12) and Stulberg classification.13) Osteoarthritic changes were evaluated using the Tonnis classification.14) Also, we analyze the relation of Stulberg classification with age and Herring's lateral pillar grade, which are established prognostic factors.
The independent t-test and chi-square test were used to determine the significances of differences between means and to analyze the influence of the prognostic factors, respectively. IBM SPSS ver. 19.0 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses, and p-values of < 0.05 were considered statistically significant.
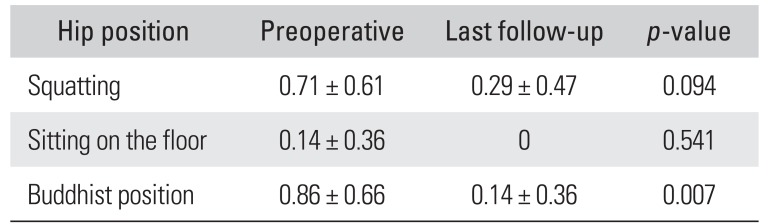
The mean HHS was 80.2 points (range, 70 to 92 points) prior to surgery and 96.2 points (range, 93 to 100 points) at the final follow-up (p = 0.001). The mean WOMAC score improved from 5 points (range, 1 to 11 points) preoperatively to 0.06 points (range, 0 to 1 points) at the final follow-up (p = 0.001) (Table 2). Improvement in the Buddhist position was also statistically significant at the final follow-up (p = 0.007) (Table 3). According to the criteria of Robinson et al.,9) 18 hips (60.0%) were good; seven (23.3%) were fair; and five (16.7%) were poor at the last follow-up. Twenty-four hips had decreased ROM compared to the preoperative value and six hips had restricted movement at the final follow-up. At the last follow-up, three hips were Tonnis classification grade 2; five hips were grade 1; and 22 hips were grade 0. Of the three hips with grade 2, two hips underwent Chiari osteotomy 12.1 and 8.8 years postoperatively, and the other hip underwent total hip arthroplasty 12.9 years postoperatively. With the exception of these two hips that underwent Chiari osteotomy, no other hip was painful, and patients with limited ROM did not experience any difficulty with the activities of daily living (Fig. 1).
The mean center-edge angle of the affected side increased from 19.7° (range, 5° to 30°) preoperatively to 29.6° (range, 19.6° to 38°) at the final follow-up. According to the Mose method, 18 hips (60.0%) were good; six (20.0%) were fair; and six (20.0%) were poor. According to the Stulberg method, nine hips (30.0%) were class I (good prognosis); nine hips (30.0%) were class II; eight hips (26.7%) were class III; and four hips (13.3%) were class IV (Table 4).
On the analysis of the influence of the established poor prognostic factors on Stulberg classification, which are age over 8 years and lateral pillar classification C, no statistically significant relationship was noted (Table 5).
It is difficult to determine the best treatment for LCPD diagnosed by clinical symptoms and abnormal radiological findings because the cause, pathology, and natural course have not yet been completely elucidated. Nonetheless, the general principle of treatment is “containment.” If a femoral head is well-contained in the cartilage mold, even in the case of collapse and deformation, it tends to be remodelled to a spherical shape, and when the femoral head finally reossifies, it becomes congruent with the acetabulum. 1516)
Olney and Asher17) reported that the treatment choice depends on the physician's preference, patient's choice, and level of activity. Of the surgical techniques designed to prevent deformity of the femoral head, the innominate osteotomy and femoral osteotomy have been most commonly used. Moreover, despite the lack of uniform clinical assessment for patients with LCPD treated by SIO,9151819) the reported incidence of physical impairment is low. Furthermore, several long-term follow-up studies have shown that patients with even marked deformities may have only mild symptoms for a long period.1213)
Our modified SIO5) differs from the original technique4) mainly in terms of the oblique osteotomy. The interposition of a triangular bone fragment facilitates achievement of required stability without internal fixation, producing the same limb lengthening effect as the Salter's osteotomy (about 1 cm). In SIO, the osteotomized bone fragment is fixed with a Steinmann pin, a hip spica cast is applied for 6 weeks, and weight-bearing is started 4 to 6 weeks after removal of the hip spica cast. On the other hand, our modified SIO requires no internal fixation or biodegradable screw fixation. However, a double splint should be applied postoperatively and intermittent active and assisted motion needs to be initiated the following day.
Salter4) reported one case of superficial wound infection and one case of osteonecrosis of the femoral head after osteotomies performed on 25 hips. Canale et al.18) reported two cases of pin tract infection and three cases of graft slippage after SIO performed on 120 patients. We have experienced no operative complications, but care should be taken to retain the subperiosteal plane throughout the modified SIO procedure because of the proximity of the sciatic nerve and the superior gluteal artery when periosteum of the inner surface of the ilium is stripped off to expose the sciatic notch.
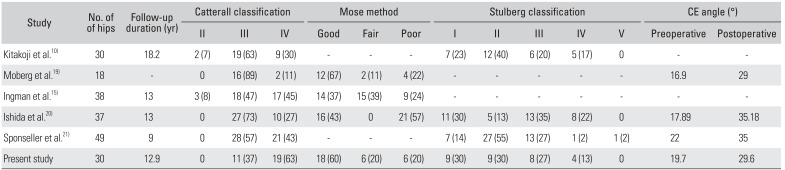
Several studies have reported on the results of SIO (Table 6). Salter16) reported 77% good, 17% fair, and 6% poor results according to the Mose method12) 50 months postoperatively. Ishida et al.20) reported clinical and radiographic results of 37 hips at skeletal maturity. Clinical results showed no correlation between sex, age, evolutionary stage and the Catterall2) and Mose12) classifications. Plain radiography at the final follow-up showed good results in 43.3% and poor results in 56.7%.
Kitakoji et al.10) reported that five of 30 hips with no preoperative restriction of motion were restricted after the Salter osteotomy. Moberg et al.19) reported that four hips in a femoral osteotomy group (16 patients) and four in an innominate osteotomy group (18 patients) had limited passive internal rotation. Ingman et al.15) compared 38 LCPD hips treated by innominate osteotomy with 33 hips, which were matched for age and severity and treated by recumbency in plaster hip spicas. Results were similar in the two groups although radiological results in the innominate osteotomy group were marginally worse. Sponseller et al.21) compared 49 innominate osteotomies with 42 femoral osteotomies and reported no difference in clinical results although the center-edge angles, neck-shaft angles, limb lengths, abduction ranges, and total ROM were closer to normal after the innominate osteotomy (Table 6).
In the present study, only five of 21 hips with a limited ROM preoperatively had a limited ROM postoperatively. In other words, unlike in previous reports,10151921) limited ROM was improved postoperatively in the majority of patients in our study. We attribute this to (1) iliopsoas tenotomy and adductor tenotomy that were performed in cases with flexion contracture or limitation of abduction and (2) passive movement exercises that were started shortly after surgery with the aim of increasing hip joint ROM.
Femoroacetabular impingement (FAI) after innominate osteotomy has been reported in some studies. Castaneda et al.22) reported the incidence as 12% (18 of 154 hips) among patients who had undergone Pemberton osteotomy and Salter osteotomy. FAI after innominate osteotomy was not common but the incidence was related to the angle of overcorrection in the study. Robb et al.23) reported 12% of acetabular retroversion after SIO without any sign of FAI. In our study, no patient complained of impingement symptoms at the last follow-up.
Several long-term follow-up studies have been conducted on the surgical treatment of LCPD. Nakashima et al.24) reported good 12-year results of trochanteric rotational osteotomy for late onset LCPD: 36% of the hips achieved a spherical, congruent status and 50%, a congruent status. Wenger and Pandya25) reported the results of two advanced surgical methods, combined SIO and triple pelvic osteotomy. They concluded that the triple innominate osteotomy might be a more attractive option because it allows relatively complete coverage of the femoral head (unlike SIO) while avoiding the risks of varus osteotomy of the femur.
Our study is limited by its retrospective design and the relatively small number of cases. In addition, most of the patients underwent the surgery before the indication of containment surgery was generally established and a consensus was made. However, it was a long-term follow-up study and the follow-up rate was high at 91% because most of the patients were male, and they had to undergo a check-up before being conscripted for obligatory military service.
In summary, our modified SIO technique requires less operative skill and can achieve stability without internal fixation due to the interposition of a bone fragment. Since the results of radiological and clinical evaluations of the modified SIO are comparable with those of SIO after physeal closure, we conclude that this simple and effective surgical modality maintains normal containment and sphericity of the femoral head.
ACKNOWLEDGEMENTS
The authors are grateful to Dr. Sun Ho Lee (Chonnam National University Hwasun Hospital, Hwasun, Korea).
References
1. Salter RB. Treatment by innominate osteotomy. Instr Course Lect. 1973; 22:309–316.
2. Catterall A. The natural history of Perthes' disease. J Bone Joint Surg Br. 1971; 53(1):37–53. PMID: 5578764.

3. Millis MB, Hall JE. Transiliac lengthening of the lower extremity: a modified innominate osteotomy for the treatment of postural imbalance. J Bone Joint Surg Am. 1979; 61(8):1182–1194. PMID: 389929.

4. Salter RB. Role of innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip in the older child. J Bone Joint Surg Am. 1966; 48(7):1413–1439. PMID: 5921797.

5. Yoon TR, Rowe SM, Chung JY, Song EK, Mulyadi D, Anwar IB. A new innominate osteotomy in Perthes' disease. J Pediatr Orthop. 2003; 23(3):363–367. PMID: 12724601.

6. Herring JA, Neustadt JB, Williams JJ, Early JS, Browne RH. The lateral pillar classification of Legg-Calve-Perthes disease. J Pediatr Orthop. 1992; 12(2):143–150. PMID: 1552014.

7. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51(4):737–755. PMID: 5783851.
8. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988; 15(12):1833–1840. PMID: 3068365.
9. Robinson HJ Jr, Putter H, Sigmond MB, O'Connor S, Murray KR. Innominate osteotomy in Perthes disease. J Pediatr Orthop. 1988; 8(4):426–435. PMID: 3392195.

10. Kitakoji T, Hattori T, Kitoh H, Katoh M, Ishiguro N. Which is a better method for Perthes' disease: femoral varus or Salter osteotomy? Clin Orthop Relat Res. 2005; (430):163–170.
11. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939; 83(Suppl 58):53–68.
12. Mose K. Methods of measuring in Legg-Calve-Perthes disease with special regard to the prognosis. Clin Orthop Relat Res. 1980; (150):103–109. PMID: 7428206.
13. Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981; 63(7):1095–1108. PMID: 7276045.
14. Tonnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976; (119):39–47.
15. Ingman AM, Paterson DC, Sutherland AD. A comparison between innominate osteotomy and hip spica in the treatment of Legg-Perthes' disease. Clin Orthop Relat Res. 1982; (163):141–147.

16. Salter RB. The present status of surgical treatment for Legg-Perthes disease. J Bone Joint Surg Am. 1984; 66(6):961–966. PMID: 6736099.

17. Olney BW, Asher MA. Combined innominate and femoral osteotomy for the treatment of severe Legg-Calve-Perthes disease. J Pediatr Orthop. 1985; 5(6):645–651. PMID: 4066935.
18. Canale ST, D'Anca AF, Cotler JM, Snedden HE. Innominate osteotomy in Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1972; 54(1):25–40. PMID: 4559945.
19. Moberg A, Hansson G, Kaniklides C. Results after femoral and innominate osteotomy in Legg-Calve-Perthes disease. Clin Orthop Relat Res. 1997; (334):257–264.
20. Ishida A, Kuwajima SS, Laredo Filho J, Milani C. Salter innominate osteotomy in the treatment of severe Legg-Calve-Perthes disease: clinical and radiographic results in 32 patients (37 hips) at skeletal maturity. J Pediatr Orthop. 2004; 24(3):257–264. PMID: 15105719.
21. Sponseller PD, Desai SS, Millis MB. Comparison of femoral and innominate osteotomies for the treatment of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1988; 70(8):1131–1139. PMID: 3417698.
22. Castaneda P, Vidal-Ruiz C, Mendez A, Salazar DP, Torres A. How often does femoroacetabular impingement occur after an innominate osteotomy for acetabular dysplasia? Clin Orthop Relat Res. 2016; 474(5):1209–1215. PMID: 26822844.
23. Robb CA, Datta A, Nayeemuddin M, Bache CE. Assessment of acetabular retroversion following long term review of Salter's osteotomy. Hip Int. 2009; 19(1):8–12. PMID: 19455495.

24. Nakashima Y, Kubota H, Yamamoto T, Mawatari T, Motomura G, Iwamoto Y. Transtrochanteric rotational osteotomy for late-onset Legg-Calve-Perthes disease. J Pediatr Orthop. 2011; 31(2 Suppl):S223–S228. PMID: 21857443.

25. Wenger DR, Pandya NK. Advanced containment methods for the treatment of Perthes disease: Salter plus varus osteotomy and triple pelvic osteotomy. J Pediatr Orthop. 2011; 31(2 Suppl):S198–S205. PMID: 21857439.
Fig. 1
Case number 22. (A) Preoperative radiograph of an 8.5-year-old male showing Legg-Calvé-Perthes disease with a Wiberg's center-edge angle of 14°. (B) Radiograph taken immediately after surgery. (C) Radiograph taken 2 years after surgery. (D) Radiograph taken 15.9 years after surgery, showing good remodeling of the acetabular osteotomy site and good femoral head sphericity.

Table 1
Demographic Characteristics of the Patients
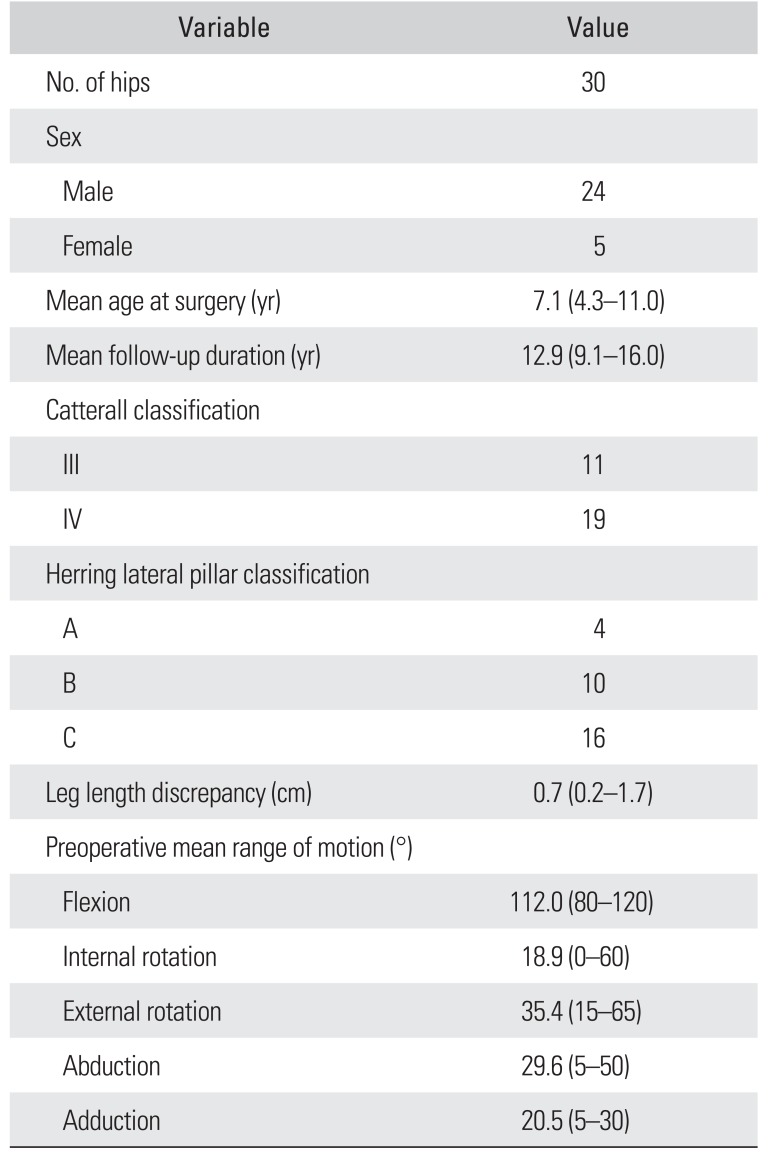
Table 2
Functional Results (HHS and WOMAC Score)
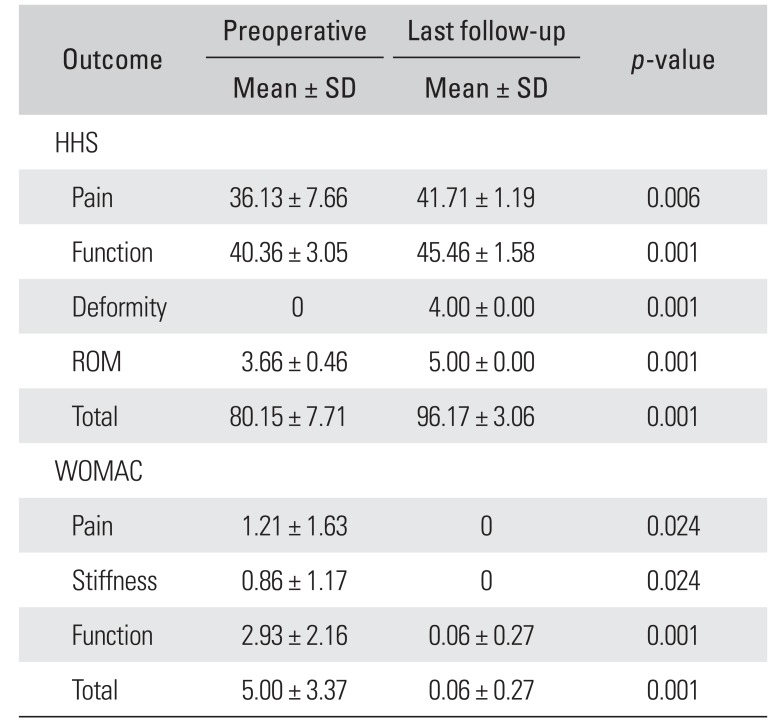
Table 3
Results of Other Common Hip Positions in Asian People
| Hip position | Preoperative | Last follow-up | p-value |
|---|---|---|---|
| Squatting | 0.71 ± 0.61 | 0.29 ± 0.47 | 0.094 |
| Sitting on the floor | 0.14 ± 0.36 | 0 | 0.541 |
| Buddhist position | 0.86 ± 0.66 | 0.14 ± 0.36 | 0.007 |
Table 4
Radiologic Results and Outcome
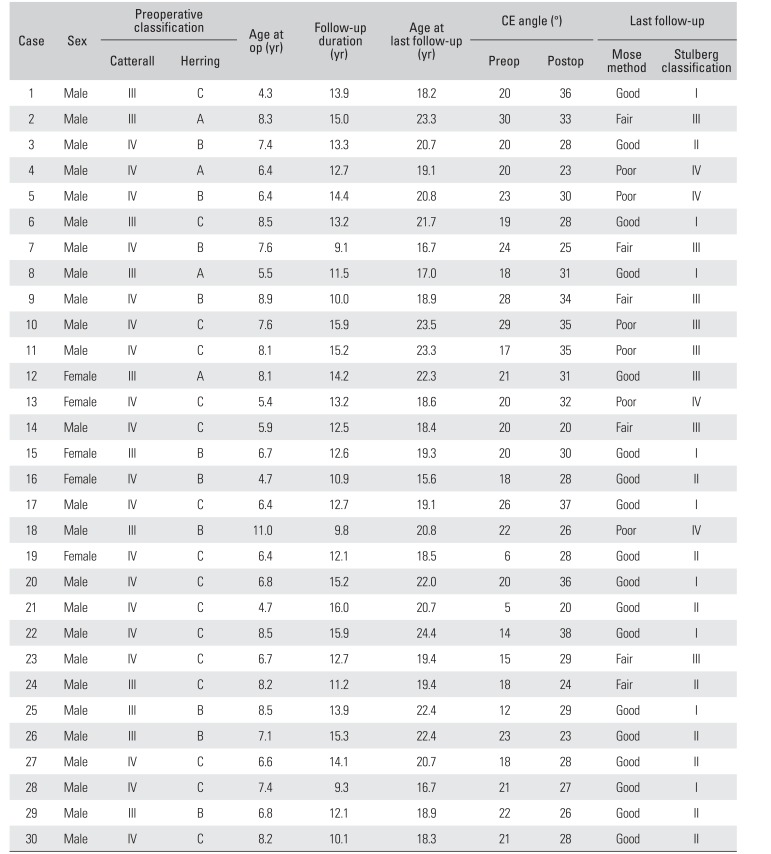
Table 5
Analysis of Stulberg Classification According to Age and Lateral Pillar Classification
| Variable | Stulberg classification | p-value | |||
|---|---|---|---|---|---|
| I | II | III | IV | ||
| Age (yr) | 0.438 | ||||
| < 8 | 6 | 8 | 3 | 3 | |
| ≥ 8 | 3 | 2 | 4 | 1 | |
| Lateral pillar classification | 0.490 | ||||
| A & B | 3 | 4 | 4 | 3 | |
| C | 6 | 6 | 3 | 1 | |
Table 6
Other Authors' Results of Salter Innominate Osteotomy for Legg-Calvé-Perthes Disease
| Study | No. of of hips | Follow-up duration (yr) | Catterall classification | Mose method | Stulberg classification | CE angle (°) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| II | III | IV | Good | Fair | Poor | I | II | III | IV | V | Preoperative | Postoperative | |||
| Kitakoji et al.10) | 30 | 18.2 | 2 (7) | 19 (63) | 9 (30) | - | - | - | 7 (23) | 12 (40) | 6 (20) | 5 (17) | 0 | - | - |
| Moberg et al.19) | 18 | - | 0 | 16 (89) | 2 (11) | 12 (67) | 2 (11) | 4 (22) | - | - | - | - | - | 16.9 | 29 |
| Ingman et al.15) | 38 | 13 | 3 (8) | 18 (47) | 17 (45) | 14 (37) | 15 (39) | 9 (24) | - | - | - | - | - | - | - |
| Ishida et al.20) | 37 | 13 | 0 | 27 (73) | 10 (27) | 16 (43) | 0 | 21 (57) | 11 (30) | 5 (13) | 13 (35) | 8 (22) | 0 | 17.89 | 35.18 |
| Sponseller et al.21) | 49 | 9 | 0 | 28 (57) | 21 (43) | - | - | - | 7 (14) | 27 (55) | 13 (27) | 1 (2) | 1 (2) | 22 | 35 |
| Present study | 30 | 12.9 | 0 | 11 (37) | 19 (63) | 18 (60) | 6 (20) | 6 (20) | 9 (30) | 9 (30) | 8 (27) | 4 (13) | 0 | 19.7 | 29.6 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download