Abstract
Intramedullary (IM) nailing for humeral shaft fracture has provided excellent outcomes in terms of fracture biology and cosmetic appearance because of the relatively small incision involved. However, antegrade nailing causes issues such as iatrogenic rotator cuff injury. Retrograde nail fixation method could avoid cuff injury, but has shortcomings such as the need for the prone or lateral decubitus position during surgery. We report that the retrograde IM nail fixation technique performed in a supine position and some ancillary techniques for minimizing scars or complications can provide the advantages of both retrograde nailing and supine position during surgery.
Surgical options for humeral shaft fractures include external fixation, open reduction and internal fixation, and anterograde or retrograde intramedullary (IM) nailing. IM locked nails have provided excellent outcomes in terms of fracture biology and cosmetic appearance because of the relatively small incision involved.1) Occasionally, this method causes issues such as iatrogenic rotator cuff injury, and many shoulder specialists do not prefer the anterograde IM nail technique for this reason.123) Surgeons have attempted retrograde nail fixation in order to avoid this problem, but this method has shortcomings such as the need for patients to maintain the prone or lateral decubitus position during surgery. The authors report that performing retrograde IM nail fixation in the supine position provides the advantages of both retrograde nailing and supine position during surgery.
The surgery was performed under general anesthesia with the patient lying in the supine position. A radiolucent table was placed next to the operating table. The entire upper extremities were painted with antiseptic by the same method generally used in fracture surgeries. Draping was performed in a manner that exposed the distal half of the clavicle and the axilla. Blocks of linen were used to elevate the patient's elbow joint to the abdominal level. The arm was abducted to 0°, elevated forward about 20°, the elbow was flexed to 90°, and the forearm was lying on the abdomen. To avoid ulnar nerve damage on the medial area, the first line was drawn from the medial epicondyle to the lateral epicondyle, and a second line was drawn on just lateral to the centre of the first line. We made a 3 cm skin incision approximately 5–6 cm proximally from the olecranon on the second line (Fig. 1). We approached the distal humerus area by splitting the triceps brachii.
After confirming the location of the olecranon fossa, we confirmed both ends of the humerus shaft proximally from this area by using a small Hohmann retractor or freer. We made three small holes with Kirschner wire on the centre of the shaft at approximately 6–7 mm intervals. We then made a 1 cm wide, 2 cm long bony inlet with a high speed burr by using the above holes as landmarks. To prevent an iatrogenic fracture of the distal humerus, we trimmed the proximal near (posterior) cortex into a sloped or beveled shape (Fig. 2).
An approximately 1 cm incision was made on the olecranon tip. The skin and the triceps tendon were gathered by the scalpel which then reached the distal humerus (Fig. 1A). The unreamed humeral nail was inserted through this small incision and bony inlet into the medullary canal by tapping carefully. If difficulty was experienced while inserting the nail into the medullary canal, the bony inlet was trimmed using a burr. For the fracture site reduction phase of the surgery, the surgeon stood beside the patient's thigh. The patient's forearm was rotated upwardly and handle of the nail downwardly. The fracture site was reduced under C-arm monitoring and the nail was advanced proximally (Fig. 1B).
After reducing the fracture and locating the nail properly, the surgeon then moved beside the patient's arm and inserted the distal interlocking screws with the guide. The surgeon inserted screws divergently to maintain a small skin incision. Inserting an end cap is recommended.
For proximal interlocking screws, the incision was made along the axillary skin fold, taking a deltopectoral approach to expose the proximal humerus (Figs. 1C and 3). The surgeon's assistant realigned the fracture gap and the possible rotational distortion that may occur during the distal interlocking screw insertion and proximal soft tissue approach procedure by controlling the patient's forearm.4)
The surgeon inserted the proximal interlocking screw anteroposteriorly, using the C-arm around the exposed proximal humerus (Fig. 2). The upper arm was then rotated internally and an additional interlocking screw was inset. The screw head and the humerus could be touched by the surgeon, allowing the degree of the screw insertion to be checked (Fig. 2B). We also checked again if the reduction and fixation were satisfactory by using the C-arm or X-ray. Lastly, we sutured the soft tissue inlet of the distal area and closed the rest of the skin incision.
Retrograde IM nailing in humerus shaft fractures has the advantage of avoiding an iatrogenic rotator cuff tear.23) For the conventional retrograde IM nailing, the patient should be positioned in the prone or lateral decubitus position. These positions may not be possible in patients with a head or facial bone injury, thoracic injury, spine injury, or multiple traumas. Surgeons can carry out the retrograde IM nailing without worsening the existing damage in a patient with multiple traumas by performing the surgery with the patient in a supine position rather than in a prone or lateral position. Draping and using the C-arm when the patient in the prone or lateral decubitus position has limitations, and many surgeons are unfamiliar with performing surgery with patients in these positions. Our technique has advantages because it is performed with the patient in a supine position.
Even in the case of a conversion to another surgery such as an open reduction, the supine position is much easier for the surgeon than the prone or lateral decubitus position. The conventional method of proximal interlocking screw insertion is from the rear to the front, which approaches blindly and may cause axillary nerve injury.5) Removal is difficult as well. Our method rarely causes axillary injury and soft tissue damages, as the surgeon can remove the implant without radiation exposure because it is possible to expose the humerus and the screw head by taking a deltopectoral approach. In the case of distal interlocking screws, it is much easier because there is an interlocking screw guide. Therefore, it is possible to remove all the internal fixtures while minimizing radiation exposure.
Iatrogenic crack or fracture of the distal cortex is representative complication of the retrograde IM nailing.4) Authors used the following methods to prevent complications. The cortex of the insertion hole was trimmed into a sloped or beveled shape. We stopped inserting the nail as soon as the most proximal screw hole of the nail was hidden behind the proximal cortex of the insertion hole.
Our method is aesthetically excellent with smaller visible scars (Fig. 3). The proximal skin incision is made through the axillary fold so the scars are hardly visible (Fig. 3D). The distal incision is separated by 2 small incisions to minimize scarring and prevent other complication such as skin-tendon adhesion (Fig. 3B). We recommend that beginners use one larger incision here due to the smaller operative visual field (Fig. 3A).
According to many reports, the result of the plate fixation is similar or slightly superior to that of the IM nail technique for a humerus fracture,1) but the retrograde IM nail technique is needed occasionally depending on the patient's condition. In such a case, our method would be very useful.
Figures and Tables
 | Fig. 1(A) The surgeon gathers the skin and triceps together to create a soft tissue inlet for the intramedullary nail. (B) For fracture reduction, the surgeon handles the patient's forearm and the nail assembly. (C) Proximal interlocking screw insertion. Skin is incised along the axillary fold and the surgeon approaches through the deltopectoral interval. The surgeon makes holes for interlocking screws without axillary nerve injury by retracting the deltoid muscle laterally. |
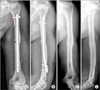 | Fig. 2Postoperative radiography shows a well-reduced fracture. (A) The red dotted line indicates skin incision. (B) The head of the proximal interlocking screw is in the anterior and lateral position. Distal posterior cortex is trimmed into a sloped or beveled shape. (C and D) One year after operation. |
 | Fig. 3Complication of large skin incision (skin-tendon adhesion). (A) The proximal part of the scar moved proximally with the triceps tendon (multiple skin wrinkles). (B) Two small separate skin incisions decreased the skin-tendon adhesion. (C) No skin wrinkles developed in triceps contraction. (D) Proximal incision for interlocking screw insertion. |
References
1. Kumar R, Singh P, Chaudhary LJ, Singh S. Humeral shaft fracture management, a prospective study; nailing or plating. J Clin Orthop Trauma. 2012; 3(1):37–42.

2. Strohm PC, Reising K, Hammer T, Sudkamp NP, Jaeger M, Schmal H. Humerus shaft fractures: where are we today? Acta Chir Orthop Traumatol Cech. 2011; 78(3):185–189.
3. Verdano MA, Pellegrini A, Schiavi P, Somenzi L, Concari G, Ceccarelli F. Humeral shaft fractures treated with antegrade intramedullary nailing: what are the consequences for the rotator cuff? Int Orthop. 2013; 37(10):2001–2007.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download