METHODS
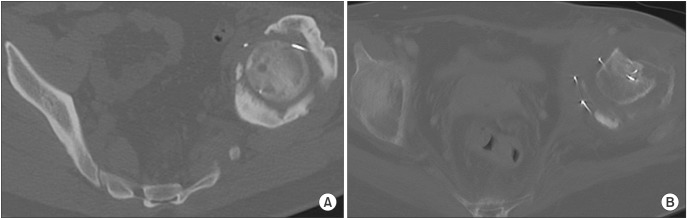 | Fig. 1(A) The axial pelvic computed tomography (CT) shows complete bony neo-acetabulum formation 9 months postoperatively. (B) The axial CT shows partial bony neo-acetabulum formation (less than 1/2 of the femoral head circumference). |
Table 1
Demographic Data of 24 Patients with Resection Hip Arthroplasty
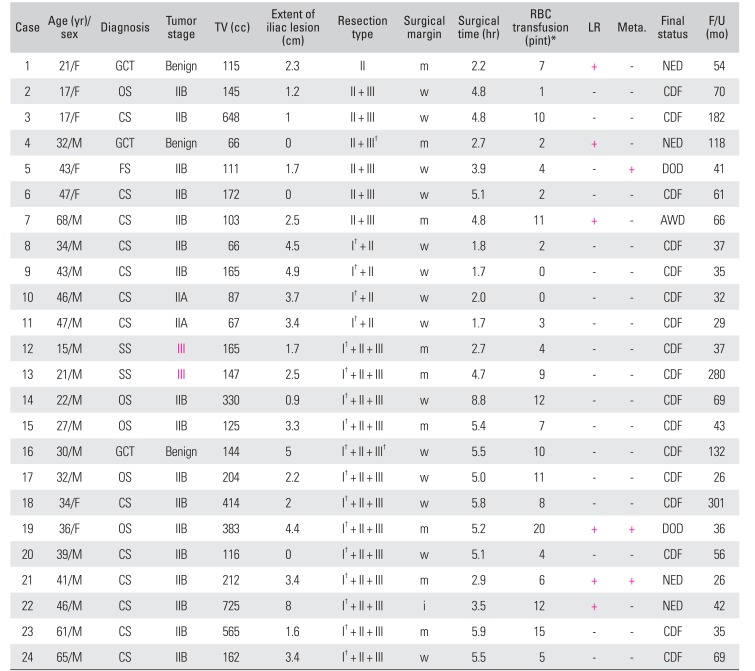
TV: tumor volume, iliac lesion: measured from the top of the femoral head, RBC: red blood cell, LR: local recurrence, Meta.: metastasis, GCT: giant cell tumor, m: marginal, +: local recurrence confirmed, NED: no evidence of disease, OS: osteosarcoma, w: wide, CDF: continuous disease-free, CS: chondrosarcoma, FS: fibrosarcoma, DOD: died of disease, AWD: alive with disease, SS: synovial sarcoma, i: intralesional.
*RBC 1 pint: 400 cc. †Partial resection of involved bone.
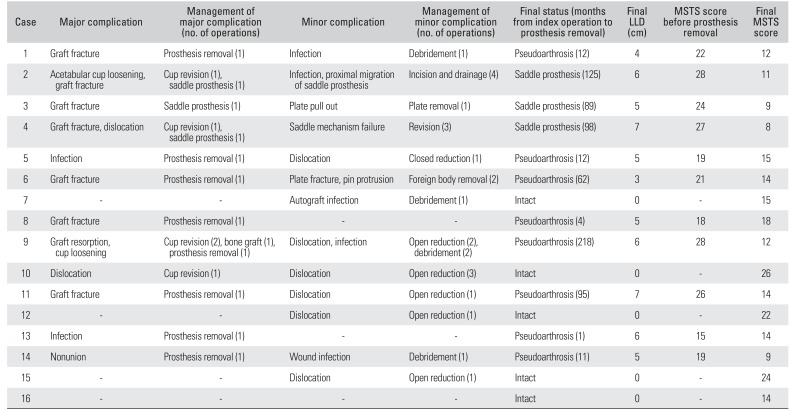
Table 2
Demographic Data of 16 Patients with Pasteurized Autograft-Prosthesis Composite Reconstruction
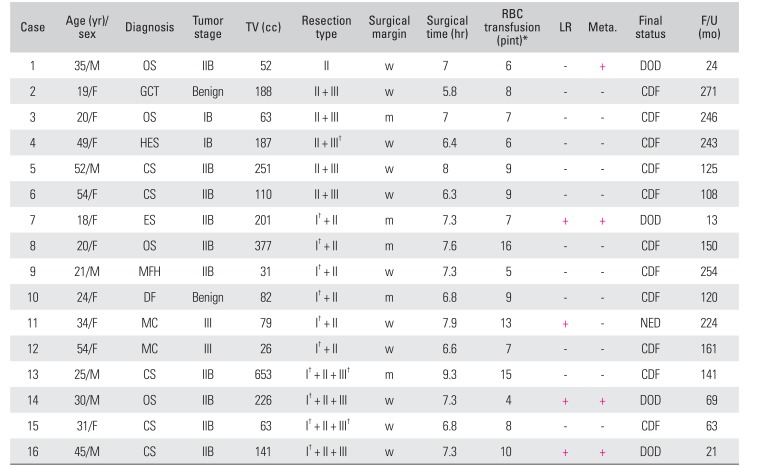
TV: tumor volume, RBC: red blood cell, LR: local recurrence, Meta.: metastasis, OS: osteosarcoma, w: wide, +: local recurrence confirmed, DOD: died of disease, GCT: giant cell tumor, CDF: continuous disease-free, m: marginal, HES: hemangioendothelioma, CS: chondrosarcoma, ES: Ewing sarcoma, MFH: malignant fibrous histiocytoma, DF: desmoplastic fibrosarcoma, MC: metastatic carcinoma, NED: no evidence of disease.
*RBC 1 pint: 400 cc. †Partial resection of involved bone.
RESULTS
Table 3
Comparison of Tumor Characteristics and Surgical Outcome between Resection Hip Arthroplasty (n = 24) and Pasteurized Autograft-Prosthesis Composite Reconstruction (n = 16)
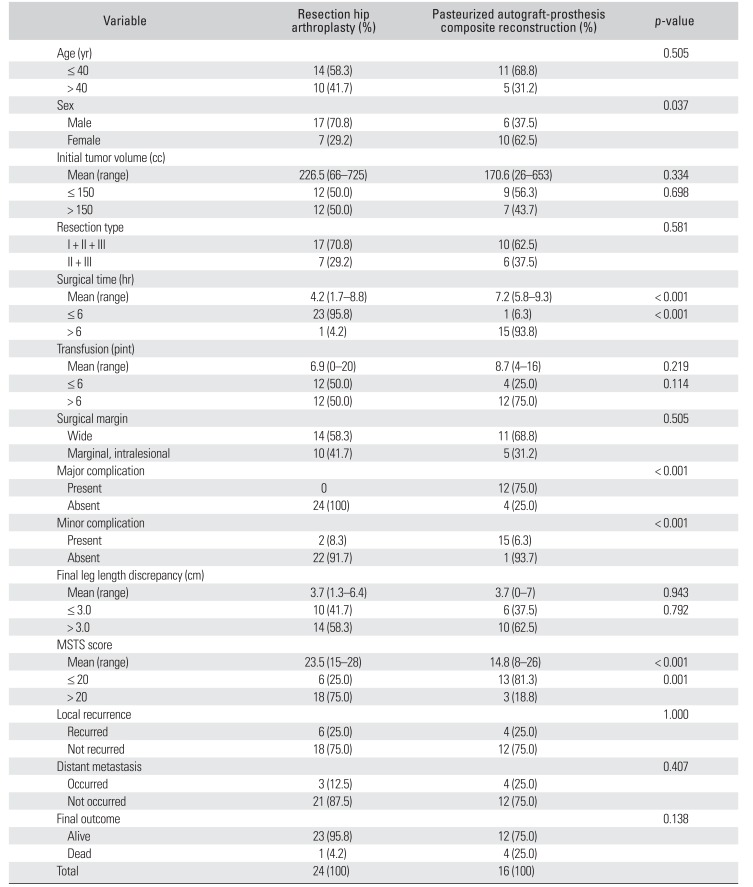
Table 4
Postoperative Course and Functional Outcome of 16 Patients with Pasteurized Autograft-Prosthesis Composite Reconstruction
 | Fig. 2(A) The preoperative plain radiograph shows a mixed osteolytic and sclerotic lesion in the right ilium and acetabulum in a 34-year-old male patient with chondrosarcoma (case 8). (B) The postoperative plain radiograph shows Enneking type II + I (partial) resection and repositioning of the previously detached iliac bone block-muscle complex with wire. (C) The follow-up plain radiograph shows complete neo-hip joint formation; the patient is fully active with shortening by 3 cm. |
 | Fig. 3(A) The plain radiograph shows an osteolytic lesion in the right acetabulum in a 41-year-old patient with chondrosarcoma (case 21). (B) The postoperative radiograph demonstrates Enneking type I (partial) + II + III (partial) resection and the femoral head fixed to the remaining iliac wing with a single wire. (C) At 6 months postoperatively, because of the high iliac osteotomy level, only partial bony neo-acetabulum had formed. The patient had no pain and could walk with one cane. |
Table 5
Postoperative Course and Functional Outcome of 24 Patients with Resection Hip Arthroplasty
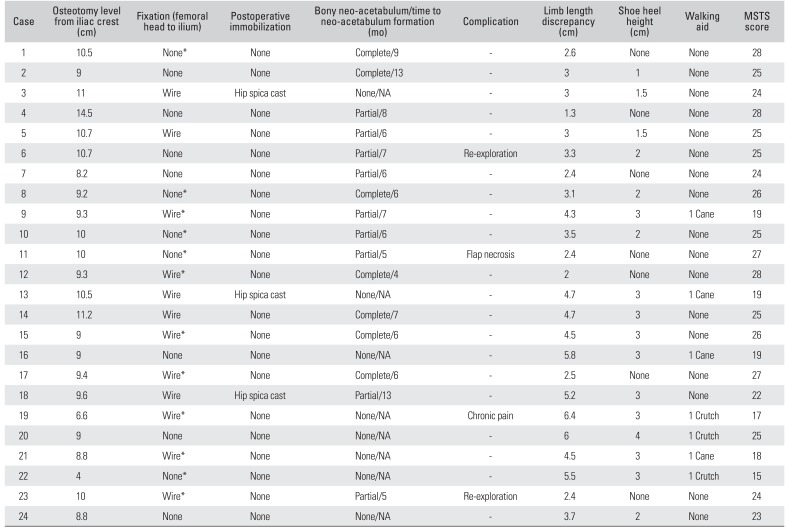
MSTS: Musculoskeletal Tumor Society, NA: not assessed, Re-exploration: during follow-up, exploration of a lesion suspicious of local recurrence on magnetic resonance imaging turned out to be a new bone in neo-acetabulum formation.
*During surgery, 2 or 3 iliac wing osteotomies were carried out to preserve the iliac crest-hip flexor or abductor muscle continuity.
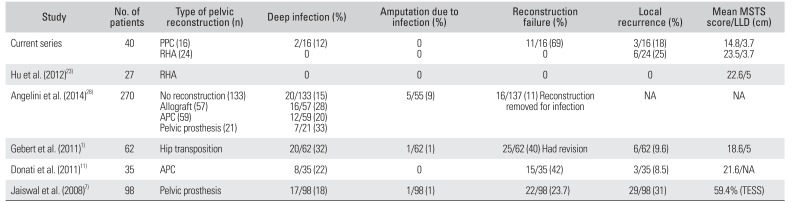
DISCUSSION
Table 6
Comparison with Previous Studies
| Study | No. of patients | Type of pelvic reconstruction (n) | Deep infection (%) | Amputation due to infection (%) | Reconstruction failure (%) | Local recurrence (%) | Mean MSTS score/LLD (cm) |
|---|---|---|---|---|---|---|---|
| Current series | 40 |
PPC (16) RHA (24) |
2/16 (12) 0 |
0 0 |
11/16 (69) 0 |
3/16 (18) 6/24 (25) |
14.8/3.7 23.5/3.7 |
| Hu et al. (2012)23) | 27 | RHA | 0 | 0 | 0 | 0 | 22.6/5 |
| Angelini et al. (2014)28) | 270 |
No reconstruction (133) Allograft (57) APC (59) Pelvic prosthesis (21) |
20/133 (15) 16/57 (28) 12/59 (20) 7/21 (33) |
5/55 (9) | 16/137 (11) Reconstruction removed for infection | NA | NA |
| Gebert et al. (2011)1) | 62 | Hip transposition | 20/62 (32) | 1/62 (1) | 25/62 (40) Had revision | 6/62 (9.6) | 18.6/5 |
| Donati et al. (2011)11) | 35 | APC | 8/35 (22) | 0 | 15/35 (42) | 3/35 (8.5) | 21.6/NA |
| Jaiswal et al. (2008)7) | 98 | Pelvic prosthesis | 17/98 (18) | 1/98 (1) | 22/98 (23.7) | 29/98 (31) | 59.4% (TESS) |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download