Abstract
Background
Radius osteotomies showed favorable clinical outcome in Kienböck's disease. However, few articles have been published on the long-term outcome of lateral wedge osteotomy of the radius in patients with advanced stage Kienböck's disease.
Methods
Eleven patients with Lichtman stage IIIB/IV Kienböck's disease (group A; mean follow-up period, 86.1 months; range, 48 to 163 months) and 14 patients with Lichtman stage IIIA Kienböck's disease (group B; mean follow-up period, 85.1 months; range, 49 to 144 months) underwent radial wedge osteotomy between August 2004 and August 2012. Radiological changes of the lunate and radiocarpal joint were compared between two groups after osteotomy. The wrist flexion/extension angle, grip strength, and Disabilities of the Arm, Shoulder and Hand (DASH) scores were evaluated preoperatively and at the final follow-up. The Nakamura Scoring System (NSSK) was used for comprehensive understanding of radiological and clinical outcomes.
Results
Nine patients of group A and 11 patients of group B showed radiological improvement in the lunate regarding sclerosis, cystic changes, or fragmentation. No patients showed progression of arthritic changes in radiocarpal and midcarpal joints. The wrist flexion/extension angle, grip strength, and DASH score were significantly improved in both groups after operation, but intergroup difference was not statistically significant at the final follow-up (p = 0.149, p = 0.267, and p = 0.536, respectively). The mean NSSK was 21.6 (range, 15 to 27) in group A and 21.8 (range, 15 to 26) in group B.
Conclusions
Radial wedge osteotomy yielded excellent radiological and functional outcomes in advanced stages of Kienböck's disease and these results were comparable to those of Lichtman stage IIIA disease. This technique could be a useful alternative to salvage procedures in the treatment of Lichtman stage IIIB/IV Kienböck's disease without severe radiocarpal arthritis.
Kienböck's disease is a form of avascular necrosis of the lunate bone with an unknown etiology.123) The Lichtman classification, based on plain radiography and magnetic resonance imaging (MRI) of the wrist, is commonly used in determining treatment options.4) According to the existence of carpal malalignment and osteoarthritic changes, Kienböck's disease can be divided into early stages (Lichtman stage I, II, and IIIA) and advanced stages (Lichtman stage IIIB and IV).56) In advanced stages, salvage procedures, such as proximal row carpectomy, limited carpal fusion, and wrist arthrodesis, have been recommended.167) However, these procedures inevitably reduce range of motion (ROM) of the wrist joint, which is considered undesirable by many patients.38910)
Radius osteotomies have shown favorable clinical results in early stages of Kienböck's disease,71112131415) and some studies reported improvement of clinical symptoms in Lichtman stage IIIB and IV Kienböck's disease.616) Radial shortening osteotomy is known to reduce the actual stress across the radiolunate joint and shift the load to the ulnar side of the wrist joint.12171819) However, this joint leveling procedure is not a reasonable treatment option for patients with neutral or positive variance of the ulna. Instead, radial closed wedge osteotomy, which decreases the radial inclination, could be used regardless of ulnar variance.6) In addition, this procedure could be combined with radial shortening in patients with negative ulnar variance.15)
Only few articles have been published on the long-term outcome of radial wedge osteotomy in Kienböck's disease, particularly among patients in advanced stages. The purpose of this study was to evaluate the radiological and clinical outcomes of radial wedge osteotomy in patients with Lichtman stage IIIB and IV Kienböck's disease and compare the results with those in patients with Lichtman stage IIIA Kienböck's disease.
This study is a retrospective case series analysis of prospectively gathered data. A total of 11 patients with Lichtman stage IIIB and IV Kienböck's disease (group A) were treated by radial wedge osteotomy between August 2004 and August 2012 and followed for more than 3 years. Patients having severe arthritic changes at the radiocarpal joint with invisible joint space were excluded because they were considered candidates for salvage procedures.20) In the same period, fourteen consecutive patients with Lichtman stage IIIA Kienböck's disease (group B) were treated with the same procedure and followed for more than 3 years. The medical records, radiographs, and evaluation data of these patients were reviewed. Two of the authors (YHS and MJC) determined the preoperative Lichtman stage based on a review of simple radiographs and MRI scans. In cases that cause confusion between stage IIIA and IIIB, 60° of radioscaphoid angle was used as a criterion for differentiation. The demographics are described in Table 1. This study was approved by the Seoul National University College of Medicine/Seoul National University Hospital Institutional Review Board (No. H-1512-097-728).
All operations were performed by a single orthopedic surgeon (GHB) with use of volar Henry approach on the distal radius. Radial wedge osteotomy was performed by making a transverse cut and an oblique cut on the metadiaphyseal junction of the distal radius, considering the thickness of the saw blade. In patients with positive and neutral ulnar variance, only the wedge osteotomy was done, whereas in patients with negative ulnar variance, radial shortening was combined with the wedge osteotomy. In all patients, the goal of corrected inclination angle was between 5° and 10°.15) In patients with negative ulnar variance, the goal of radial shortening was to obtain a final variance of neutral to 2 mm positive18) while limiting radial length alteration to ≤ 3 mm regardless of ulnar variance.17) Two patients in group B, who had positive ulnar variance of more than 5 mm, had ulnar shortening osteotomy simultaneously. All osteotomies were fixed with a plate and screws system: a five- or six-hole small dynamic compression plate (Stryker Orthopedics, Mahwah, NJ, USA) in the earlier patients and a locking compression plate for the distal radius (Synthes, Oberdorf, Switzerland) in the later patients.
Postoperatively, the patients were managed for the first 2 weeks with a sugar tong splint that was then converted to a removable short arm splint worn for an additional period of four to 8 weeks. Standard posteroanterior and lateral radiographs were taken immediately postoperatively and during the follow-up assessments at 2, 6, 9, and 12 weeks and 6 and 12 months postoperatively. Patients were then followed up annually.
Radiological changes of the lunate and radiocarpal joint were assessed with preoperative and final follow-up radiographs. Changes in lunate morphology and Lichtman stage and the presence or deterioration of degenerative changes at the radiocarpal and midcarpal joints were evaluated by two of the authors (YHS and MJC). In addition, radiological measurements, including ulnar variance,21) radial inclination angle,13) radioscaphoid angle,5) carpal height ratio,22) and Stahl index23) were performed with preoperative and final follow-up radiographs. The images were assessed on a 21.3-inch liquid crystal display monitor (MDNG-6121; Barco, Kortrijk, Belgium) in portrait mode using picture archiving and communication system (PACS) software. These measurements were performed by two of the authors (YHS and MJC) and the mean value of the 2 measurements was used for analysis.
The flexion/extension angle of both wrists, grip strength of both hands, and score of Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire (scale of 0–100, with higher scores indicating greater disability) were assessed preoperatively and final follow-up to evaluate the clinical outcomes of radial wedge osteotomy. The ROM of the affected wrist and the contralateral side was measured using a goniometer. Grip strength was measured using the Jamar dynamometer (Asimow Engineering, Los Angeles, CA, USA) with the elbow flexed at 90° and the forearm in neutral position. The extent of wrist pain in activities of daily living was assessed using the visual analogue scale (VAS; 0 = no pain, 10 = severe pain) at the final follow-up. The Nakamura Scoring System (NSSK) for Kienbőck's disease was used for comprehensive assessment of the clinical and radiological changes at the final follow-up.11) This scoring system consists of clinical assessments including pain, grip strength, change of flexion/extension angle and radiological assessments including change of the lunate shape, carpal height ratio, and Stahl index. The NSSK score ranges from 0 to 30, with higher scores indicating more improvement after osteotomy: excellent, 24–30; good, 18–23; fair, 12–17; and poor, 0–11.
All of the statistical analyses were performed with IBM SPSS ver. 22.0 (IBM Co., Armonk, NY, USA), and p-value < 0.05 was determined as the level of statistical significance. The Mann-Whitney U-test or Fisher exact test were used to compare the demographics, preoperative status and final follow-up outcomes of the two groups. Pre- and postoperative data were compared with use of the Wilcoxon signed-rank test within each group. Interobserver reliability of radiologic measurement was assessed with intraclass correlation coefficients (ICCs) derived from a two-way random effect model.24)
The preoperative radiological and clinical evaluations and corrective osteotomy planning are described in Table 2. Ulnar variance, radial inclination angle, and carpal height ratio were not significantly different between two groups. Ulnar variance was positive in 1, neutral in 2, and negative in 8 patients of group A and positive in 2, neutral in 2, and negative in 10 patients of group B. Radioscaphoid angle and Stahl index were significantly different between two groups (p < 0.001, respectively). Clinical evaluations including the mean angle of wrist flexion/extension, grip strength, and DASH score were not significantly different between two groups. In addition, the planned correction of ulnar variance and radial inclination were not significantly different between two groups (p = 0.727 and p = 0.085, respectively).
The osteotomy site union was achieved in all patients. There were no complications such as nonunion or infection. Nine patients of group A and 11 patients of group B showed radiological improvement in the lunate regarding sclerosis, cystic changes, or fragmentation after operation: sclerosis in 7, cystic changes in 5, and fragmentation in 8 patients of group A; and sclerosis in 10, cystic changes in 6, and fragmentation in 8 patients of group B. No progression of the Lichtman stage was found in any patients, and no cases showed development and progression of arthritic changes of the radiocarpal and midcarpal joints at the final follow-up.
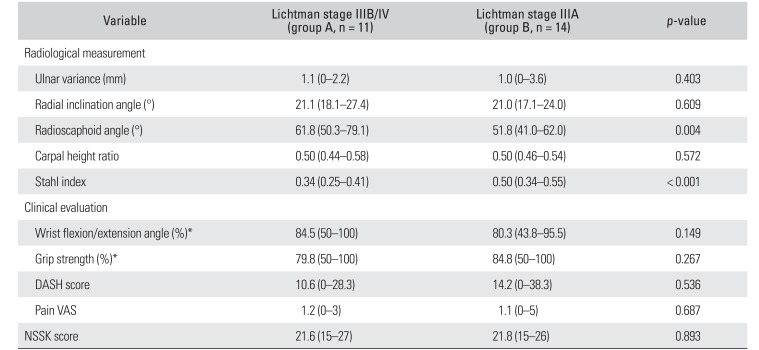
The radiological measurements and clinical evaluations at the final follow up are described in Table 3. The relationships between radiological parameters and preoperative Lichtman stage were similar to those preoperatively observed. Ulnar variance and radial inclination angle were changed significantly after operation, but no significant differences were observed in the radioscaphoid angle, carpal height ratio, and Stahl index between preoperative and final follow-up measurements both groups. The interobserver reproducibility of radiological measurements was excellent with an ICC of 0.951 for the ulnar variance, 0.868 for the radial inclination angle, 0.804 for the radioscaphoid angle, 0.978 for the carpal height ratio, and 0.988 for the Stahl index.
The mean angle of wrist flexion/extension, grip strength, and DASH score were significantly improved in both groups, but no significant difference was noted between two groups at the final follow up (p = 0.149, p = 0.267 and p = 0.536, respectively). The mean pain VAS score during activities of daily living at the final follow-up was 1.2 (range, 0 to 3) in group A and 1.1 (range, 0 to 5) in group B. Four wrists in group A and 7 wrists in group B were asymptomatic. The mean NSSK was 21.6 (range, 15 to 27) in group A and 21.8 (range, 15 to 26) in group B at the final follow-up, showing no statistically significant difference between groups (p = 0.893): 3 were rated excellent, 7 good, and 1 fair in group A; and 4 were rated excellent, 9 good, and 1 fair in group B (Figs. 1 and 2).
Radial wedge osteotomy that decreases the radial inclination is known to reduce the pressure on the lunate by increasing the contact area between the diseased lunate and radius, shifting the load to the radial side of the wrist joint.611) The present study shows that radial wedge osteotomy yielded excellent radiological and functional outcomes in the treatment of advanced stages of Kienböck's disease and these results were comparable to those of stage IIIA Kienböck's disease.
Radial osteotomies have shown favorable clinical results in the treatment of Kienböck's disease, but these procedures could not restore the morphology of the collapsed lunate and the changed carpal alignment.71112131415) Thus, the efficacy of radial osteotomies in advanced stages of Kienböck's disease has been controversial and salvage procedures have been recommended in these stages.810) However, salvage procedures, such as proximal row carpectomy, limited carpal fusion, and wrist arthrodesis reduce the wrist ROM.38910) In addition, these salvage procedures could not halt the secondary arthritic changes in the radiocarpal and other joints around the wrist, despite symptomatic relief.9102526) Radial osteotomy is a relatively simple extra-articular procedure, and surgery itself does not influence the flexion/extension of the wrist joint. In addition, other procedures involving articular structures could be attempted later period of the disease without concern for previous operation's scar adhesion.1327)
Several studies have reported on the role of radial osteotomy in the treatment of advanced stage Kienböck's disease. Iwasaki et al.6) compared the results between radial shortening osteotomy and radial wedge osteotomy in Lichtman stage IIIB and IV Kienböck's disease patients. All patients showed good or excellent clinical results regardless of procedures and 25% of patients (5 of 20 patients) showed radiological improvement of the lunate. However, they evaluated patients with a modified form of NSSK that excluded the radiological evaluation, and the average follow-up period was rather short (29 months). Matsui et al.18) reported the results of radial shortening osteotomy and Soejima et al.16) reported the results of radial wedge osteotomy in advanced stages. Despite achievement of satisfactory clinical results in all patients, they denied the role of radial osteotomy for radiographic improvement of the lunate. Mozaffarian et al.8) reported poor results of radial shortening osteotomy in patients with advanced stage Kienböck's disease (stage IV), but they did not evaluate the morphologic changes of the lunate.
We think that the excellent radiological and functional outcomes of our patients could be explained by the high proportion of patients receiving combined radial shortening and lateral closed wedge osteotomy. More than two third of patients in each group received combined osteotomy as all of them showed negative ulnar variance. It is known that combined radial osteotomy could provide the benefits of 2 procedures simultaneously15) and prevent the complications related to each radial osteotomy. Concerns about overcorrection of bony morphology of the radiocarpal and distal radioulnar joints could be reduced by use of this technique. By controlling the shortening length of the radius under 3 mm, development of incongruence of the distal radioulnar joint and iatrogenic ulnar impaction syndrome could be avoided. By reducing the extent of correction of the radial inclination angle under ten degrees, several known complications of radial wedge osteotomy, such as secondary radioscaphoid arthritic changes due to excessive load redistribution,6) compensatory excessive ulnar deviation of the wrist,15) and development of limitation of forearm rotation,11) could be avoided.
The Lichtman classification system is based on radiological findings and does not reflect the clinical situations.5) We think that the similar preoperative clinical presentation between group A and B could be associated with this limitation of the staging system. In addition, the preoperative Lichtman stage did not have any influence on the clinical and radiological outcomes of the operation in this study. The radioscaphoid angle of the wrist and preexisting arthritic changes of the radiocarpal joint were not improved significantly after radial wedge osteotomy despite clinical improvement of symptoms. This can be interpreted that carpal malalignment including scaphoid malrotation did not change after surgery. Our findings are compatible with those of previous studies on radial osteotomy reporting poor correlation between radiologic parameters and clinical outcomes.3712)
Our study has several limitations. First, the number of patients was small. Second, 2 kinds of different plate and screw systems were used for osteotomy site fixation. Thus, there is a need for larger prospective multi-center studies, incorporating objective measures for radial wedge osteotomy with other procedures.
In conclusion, radial wedge osteotomy yielded excellent radiological and functional outcomes in the treatment of advanced stage Kienböck's disease and these results were comparable to those of stage IIIA Kienböck's disease. This procedure would be a useful alternative to the salvage procedures in the treatment of Lichtman stage IIIB and IV Kienböck's disease without severe radiocarpal arthritis.
ACKNOWLEDGEMENTS
We thank Joo Hyun Oh for her consultation for statistical analysis and English proofreading.
References
1. Schuind F, Eslami S, Ledoux P. Kienbock's disease. J Bone Joint Surg Br. 2008; 90(2):133–139. PMID: 18256076.
2. Danoff JR, Cuellar DO, O J, Strauch RJ. The management of Kienbock disease: a survey of the ASSH membership. J Wrist Surg. 2015; 4(1):43–48. PMID: 25709878.
3. Innes L, Strauch RJ. Systematic review of the treatment of Kienbock's disease in its early and late stages. J Hand Surg Am. 2010; 35(5):713–717. 713.e1–717.e4. PMID: 20438990.
4. Lichtman DM, Mack GR, MacDonald RI, Gunther SF, Wilson JN. Kienbock's disease: the role of silicone replacement arthroplasty. J Bone Joint Surg Am. 1977; 59(7):899–908. PMID: 908720.
5. Goldfarb CA, Hsu J, Gelberman RH, Boyer MI. The Lichtman classification for Kienbock's disease: an assessment of reliability. J Hand Surg Am. 2003; 28(1):74–80. PMID: 12563641.
6. Iwasaki N, Minami A, Oizumi N, Suenaga N, Kato H, Minami M. Radial osteotomy for late-stage Kienbock's disease: wedge osteotomy versus radial shortening. J Bone Joint Surg Br. 2002; 84(5):673–677. PMID: 12188482.
7. Weiss AP, Weiland AJ, Moore JR, Wilgis EF. Radial shortening for Kienbock disease. J Bone Joint Surg Am. 1991; 73(3):384–391. PMID: 2002076.
8. Mozaffarian K, Namazi H, Namdari A. Radial shortening osteotomy in advanced stages of Kienbock disease. Tech Hand Up Extrem Surg. 2012; 16(4):242–246. PMID: 23160560.

9. Rhee PC, Lin IC, Moran SL, Bishop AT, Shin AY. Scaphocapitate arthrodesis for Kienbock disease. J Hand Surg Am. 2015; 40(4):745–751. PMID: 25701486.
10. Nakamura R, Horii E, Watanabe K, Nakao E, Kato H, Tsunoda K. Proximal row carpectomy versus limited wrist arthrodesis for advanced Kienbock's disease. J Hand Surg Br. 1998; 23(6):741–745. PMID: 9888672.
11. Nakamura R, Tsuge S, Watanabe K, Tsunoda K. Radial wedge osteotomy for Kienbock disease. J Bone Joint Surg Am. 1991; 73(9):1391–1396. PMID: 1918122.
12. Rodrigues-Pinto R, Freitas D, Costa LD, et al. Clinical and radiological results following radial osteotomy in patients with Kienbock's disease: four- to 18-year follow-up. J Bone Joint Surg Br. 2012; 94(2):222–226. PMID: 22323690.
13. Wada A, Miura H, Kubota H, Iwamoto Y, Uchida Y, Kojima T. Radial closing wedge osteotomy for Kienbock's disease: an over 10 year clinical and radiographic follow-up. J Hand Surg Br. 2002; 27(2):175–179. PMID: 12027496.
14. Watanabe T, Takahara M, Tsuchida H, Yamahara S, Kikuchi N, Ogino T. Long-term follow-up of radial shortening osteotomy for Kienbock disease. J Bone Joint Surg Am. 2008; 90(8):1705–1711. PMID: 18676901.
15. Garcia-Elias M, An KN, Cooney WP, Linscheid RL. Lateral closing wedge osteotomy for treatment of Kienbock's disease: a clinical and biomechanical study of the optimum correcting angle. Chir Main. 1998; 17(4):283–290. PMID: 10855296.
16. Soejima O, Iida H, Komine S, Kikuta T, Naito M. Lateral closing wedge osteotomy of the distal radius for advanced stages of Kienbock's disease. J Hand Surg Am. 2002; 27(1):31–36. PMID: 11810611.
17. Trumble T, Glisson RR, Seaber AV, Urbaniak JR. A biomechanical comparison of the methods for treating Kienbock's disease. J Hand Surg Am. 1986; 11(1):88–93. PMID: 3944452.
18. Matsui Y, Funakoshi T, Motomiya M, Urita A, Minami M, Iwasaki N. Radial shortening osteotomy for Kienbock disease: minimum 10-year follow-up. J Hand Surg Am. 2014; 39(4):679–685. PMID: 24612833.
19. Muramatsu K, Ihara K, Kawai S, Doi K. Ulnar variance and the role of joint levelling procedure for Kienbock's disease. Int Orthop. 2003; 27(4):240–243. PMID: 12827300.
20. Gong HS, Chung MS, Lee YH, Lee S, Lee JO, Baek GH. Arthroplasty for advanced Kienbock's disease using a radial bone flap with a vascularised wrapping of pronator quadratus. J Bone Joint Surg Br. 2006; 88(5):623–628. PMID: 16645108.
21. Gelberman RH, Salamon PB, Jurist JM, Posch JL. Ulnar variance in Kienbock's disease. J Bone Joint Surg Am. 1975; 57(5):674–676. PMID: 1150712.

22. Youm Y, McMurthy RY, Flatt AE, Gillespie TE. Kinematics of the wrist: I. an experimental study of radial-ulnar deviation and flexion-extension. J Bone Joint Surg Am. 1978; 60(4):423–431. PMID: 670263.

23. Stahl F. On lunatomalacia (Kienboock's disease) a clinical and roentgenological study, especially on its pathogenesis and the late results of immobilization treatment. Lund, Sweden: H. Ohlsson;1947. p. 133.
24. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979; 86(2):420–428. PMID: 18839484.

25. Luegmair M, Saffar P. Scaphocapitate arthrodesis for treatment of late stage Kienbock disease. J Hand Surg Eur Vol. 2014; 39(4):416–422. PMID: 23824220.
26. Croog AS, Stern PJ. Proximal row carpectomy for advanced Kienbock's disease: average 10-year follow-up. J Hand Surg Am. 2008; 33(7):1122–1130. PMID: 18762108.
27. Kakinoki R, Yamakawa T, Nakayama K, Morimoto Y, Nakamura T. Treatment of progressive necrosis of the lunate bone (Kienbock disease) after unsuccessful radial osteotomy. Scand J Plast Reconstr Surg Hand Surg. 2007; 41(5):267–271. PMID: 17886131.
Fig. 1
The preoperative T1-weighted magnetic resonance imaging (A) and posteroanterior (PA) radiograph (B) of a 51-year-old woman show stage IIIA Kienböck's disease in the left wrist. (C) The 5-year postoperative PA radiograph shows a decreased sclerotic lesion in the lunate. (D) The PA radiograph taken at the last visit at postoperative 11 years shows that the morphology of the lunate became nearly normalized. The bony trabecular pattern inside the lunate was similar to surrounding carpal bones. No progression of arthritic changes was visible in the radiocarpal and midcarpal joints.

Fig. 2
The preoperative posteroanterior (PA) radiograph (A) and lateral radiograph (B) of a 15-year-old man show stage IIIB Kienböck's disease in the left wrist. Six-year postoperative PA radiograph (C) and lateral radiograph (D). Radiological improvement and height restoration were observed in the diseased lunate. No development of arthritic changes was visible in the radiocarpal and midcarpal joints. The photographs of the wrist in active volar flexion (E) and in active dorsiflexion (F) show a similar range of motion of the wrist joint compared to the contralateral side.
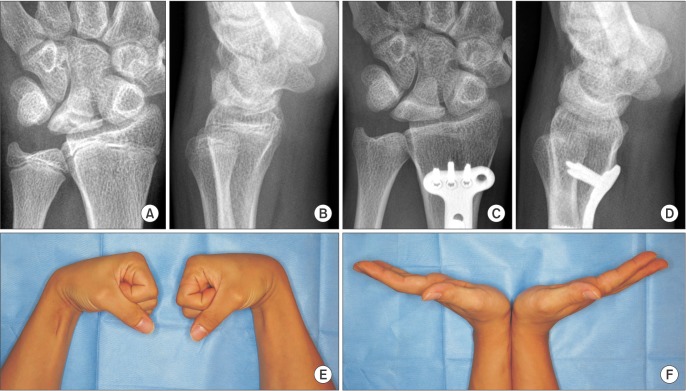
Table 1
Demographics of Enrolled Patients
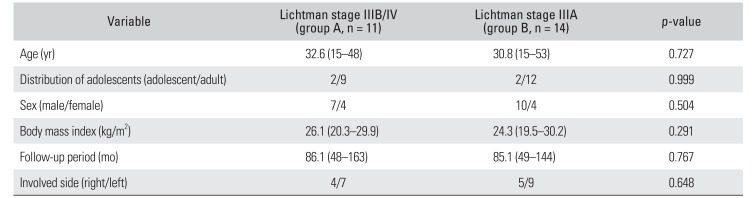
Table 2
Preoperative Evaluation and Corrective Osteotomy Planning in Two Groups
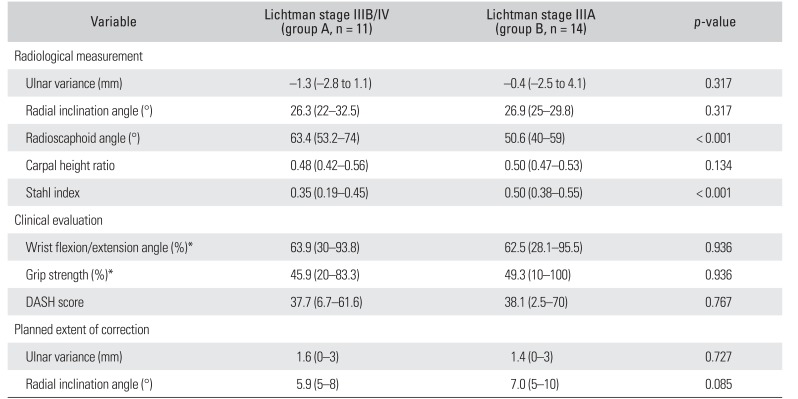
Table 3
Radiological and Clinical Evaluations at Final Follow-up




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download