Abstract
Background
The purpose of this study was to evaluate the angle between the long head of the biceps tendon (LHBT) and the glenoid during arthroscopic surgery and its correlation with biceps subluxation on magnetic resonance imaging (MRI). Furthermore, we evaluated the relationship of this angle with subscapularis tears and biceps pathologies.
Methods
MRI and arthroscopic images of 270 consecutive patients who had undergone arthroscopic surgery were retrospectively evaluated. On MRI, 60 shoulders with biceps subluxation and 210 shoulders without subluxation were identified. On the arthroscopic view from the posterior portal, the angle between the LHBT and the glenoid (biceps-glenoid angle) was measured. The biceps-glenoid angle, tears of the LHBT, degenerative superior labrum anterior to posterior (SLAP) lesions, and presence of a subscapularis tear were compared according to the presence of biceps subluxation on MRI.
Results
In the subluxation group, 51 (85%) had a subscapularis tendon tear and all shoulders showed biceps tendon pathologies. In the non-subluxation group, 116 (55.2%) had a subscapularis tendon tear, 125 (60%) had tears in the biceps tendon, and 191 (91%) had degenerative SLAP lesions. The incidences of subscapularis tears (p < 0.001) and biceps pathologies (p < 0.001) showed significant differences. The mean biceps-glenoid angle was 87.0° (standard deviation [SD], 11.4°) in the subluxation group and 90.0° (SD, 9.6°) in the non-subluxation group, showing a statistically significant difference (p = 0.037).
Conclusions
Shoulders with subluxation of the biceps tendon on the preoperative MRI revealed more pathologies in the subscapularis tendon and biceps tendon during arthroscopy. However, the arthroscopically measured biceps-glenoid angle did not have clinical relevance to the determination of subluxation of the LHBT from the bicipital groove.
The long head of the biceps tendon (LHBT) of the shoulder runs from the distal bicipital groove to the proximal end, crosses the glenoid cavity, and attaches to the supraglenoid tubercle.1) The stability of the LHBT is provided by the biceps pulley that consists of the transverse humeral ligament found at the bicipital groove, and the superior glenoid humeral ligament and coracohumeral ligament, which are found at the entry of the bicipital groove.2)
Medial subluxation or dislocation of the LHBT is commonly associated with lesions of the rotator cuff, especially those of the subscapularis tendon.345) Walch et al.5) reported that up to 60% of patients with rotator cuff pathologies presented with combined medial dislocation or subluxation of the LHBT. Shi et al.4) reported that medial subluxation of the LHBT is a predictor of subscapularis tendon tears. Only 2 cases of medial dislocation of the LHBT that had occurred in isolation and without rotator cuff pathologies were reported by Gambil et al.6) in their series, showing that such cases are rare.7)
Pathologies of the LHBT including tendinitis, tendinopathies, subluxation, and partial or complete tears are generally accompanied by rotator cuff pathologies. Detection of biceps pathologies other than complete ruptures based only on the symptoms, signs, or even magnetic resonance imaging (MRI) is difficult.8) Most of these biceps pathologies are easily confirmed by arthroscopic examination during surgery. However, subluxation of the LHBT is difficult to confirm even with arthroscopic examination. Moreover, there is no consensus regarding the arthroscopic findings of subluxation. Motley et al.9) used an arthroscopic ramp test to assess the stability of the LHBT and evaluate subluxation, but its application is not advised until additional research confirms its validity as an objective predictor.
The purpose of this study was to evaluate the angle between the LHBT and the glenoid (biceps-glenoid angle) during arthroscopic surgery and correlation of the angle with biceps subluxation on preoperative MRI. Furthermore, we evaluated the relationship of the arthroscopic biceps-glenoid angle with subscapularis tears.
Our null hypothesis was that the arthroscopic biceps-glenoid angle would not be different according to the presence of LHBT subluxation on preoperative MRI.
From January 2012 to August 2013, we enrolled a total of 270 patients who underwent arthroscopy of the shoulder in our retrospective study. Inclusion criteria were as follows: (1) subluxation of the LHBT that could be diagnosed by preoperative shoulder MRI and (2) patients in whom the angle between the LHBT and the labrum could be measured arthroscopically. We excluded patients showing the absence or definite dislocation of the biceps tendon. We categorized the patients into 2 groups based on the findings of preoperative MRI: those who had subluxation of the LHBT were in the subluxation group, and those who did not have subluxation of the LHBT were in the non-subluxation group.
Using a 3.0T system (Philips Achieva; Philips Medical Systems, Best, Netherlands), we performed preoperative MRI examinations with the patients lying down and the affected humerus in neutral position. We obtained the fat-suppressed T1-weighted fast spin-echo sequence in the axial view (repetition time/echo time [TR/TE], 565/19 ms; section thickness, 3 mm; field of view [FOV], 15 cm; matrix size, 248/247), coronal view (TR/TE, 562/21 ms; section thickness, 3 mm; FOV, 15 cm; matrix size, 264/262), and sagittal view (TR/TE, 561/18 ms; section thickness, 4 mm; FOV, 15 cm; matrix size, 264/262), and the T2-weighted fast spin-echo sequence in the axial view (TR/TE, 2,906/80 ms; section thickness, 3 mm; FOV, 15 cm; matrix size, 248/239), coronal view (TR/TE, 2,906/80 ms; section thickness, 3 mm; FOV, 15 cm; matrix size, 264/259), and sagittal view (TR/TE, 2,906/80 ms; section thickness, 4 mm; FOV, 15 cm; matrix size, 264/259). In addition, we used the fat-suppressed T1-weighted fast spin-echo sequence to determine whether there was subluxation, dislocation, or absence of the LHBT in the groove. We defined dislocation of the LHBT as when the tendon is positioned more medially within the bicipital groove than usual, and subluxation as when the tendon is positioned superior to the medial border rather than within the groove (Fig. 1).5) An experienced musculoskeletal radiologist evaluated all axial images.
Shoulder arthroscopy was performed with the patient in the lateral decubitus position. To observe the angle at the intersection of the LHBT and the labrum, we used the routine posterior portal made through the soft spot. Arthroscopic images of the rotator interval were taken with the humerus in neutral position. To ensure the arm was in neutral position, we took additional images with the arm in internal and external rotation. Thus, we took 3 serial arthroscopic images of the rotator interval with the arm in internal rotation, neutral, and external rotation.
We defined the biceps-glenoid angle as the angle between the LHBT and the superior half of the anterior glenoid (Fig. 2). The angle was measured twice by an independent orthopedic surgeon who was not involved in the assessment of the MRI findings and the surgery. We assessed the intraobserver agreement for the angles that were measured with an inverval of at least 1 week between each measurement.
The exclusion criteria for the study recruitment were as follows: (1) a preoperative MRI showing a dislocated LHBT; (2) deformity of the bicipital groove that prevented determination of subluxation of the LHBT; (3) shoulder infection that required surgical debridement, fractures, traumatic dislocations; (4) a previous history of shoulder arthroscopy; (5) absence of arthroscopic images of the rotator interval in at least 1 position of the humerus (internal rotation, neutral rotation, or external rotation); (6) an insufficient arthroscopic window/frame that prevented measurement of the biceps-glenoid angle; (7) a partial tendon tear so severe that the direction of the tendon was difficult to determine; (8) complete tendon tears; and (9) an hourglass-pattern LHBT, for which the direction of the tendon was anatomically difficult to discern.
Based on preoperative MRI, we divided patients into subluxation and non-subluxation groups. We compared the arthroscopic diagnosis of pathologies in the LHBT, their treatment, and the biceps-glenoid angle between groups. We also investigated whether the 2 groups differed in the incidence of tears in the subscapularis tendon10) concomitant with LHBT pathologies. For continuous variables with normal distribution, we used the Wilcoxon Mann-Whitney U-test or the 2 sample t-test to test for significance. For categorical variables, Fisher exact test or the Cochran-Armitage trend test was used for comparisons. Statistical analyses were performed with SAS ver. 9.1.3 (SAS Institute, Cary, NC, USA). The significance level was set at 0.05 for all analyses.
We assessed the intraobserver reliability for the angle measurements. A single observer made 2 measurements of the angle on separate occasions, allowing at least 1 week of interval between each measurement. Analysis was made using Pearson linear correlation coefficients, and the p-value was calculated.
The 270 patients included 125 males (46.3%) and 145 females (53.7%), with a mean age of 57.1 years (range, 19 to 86 years), a mean height of 162.7 cm, and a mean weight of 67.1 kg. There were 194 right shoulders (71.8%) and 76 left shoulders (28.2%). The dominant arm was involved in 199 patients (73.7%), and the nondominant arm in 71 (33.8%). The initial diagnoses at the time of operation were rotator cuff tears in 241 (89.2%), anterior instability in 4 (1.5%), and other in 25 (9.3%). Preoperative MRI showed subluxation of the LHBT in 60 patients (22.2%, subluxation group) and no subluxation in the other 210 patients (77.8%, non-subluxation group).
In the subluxation group, 58 patients (96.8%) had rotator cuff tears and 2 (3.2%) had other pathologies. In the non-subluxation group, 183 patients (87.1%) had rotator cuff tears, 4 (1.8%) had instability, and 23 (11.0%) had other pathologies (Table 1).
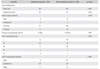
During arthroscopic examination of the subluxation group, we found that all 60 patients had tears of the biceps tendon and all 60 had degenerative superior labrum anterior to posterior (SLAP) lesions. In the non-subluxation group, 125 patients had biceps tears and 191 had degenerative SLAP lesions. The incidence of biceps pathologies showed statistically significant differences between the 2 groups (p < 0.001 and p = 0.010, respectively). In the subluxation group, we performed no procedure in 9 (15%), tenotomy in 37 (62%), and tenodesis in 14 patients (23%). In the non-subluxation group, we performed observation only in 73 (34.8%), debridement in 2 (1%), tenotomy in 100 (48%), and tenodesis in 35 patients (17%). There was a statistically significant difference between the 2 groups in terms of treatment (p = 0.014).
There were tears of the subscapularis tendon in 167 of 270 patients. Of these, 117 (70.1%) underwent debridement and 32 (19.2%) underwent repair. In the other 18 (10.8%), only observation was conducted. A tear of the subscapularis was found in 51 of 60 patients (85%) in the subluxation group and in 116 of 210 (55.2%) in the non-subluxation group, showing a significant difference (p = 0.001) (Table 2). In the subluxation group, observation only was done in 9 (15.0%), debridement in 34 (56.7%), and repair in 17 patients (28.3%). In the non-subluxation group, we did observation only in 112 (53.3%), debridement in 83 (39.5%), and repair in 15 patients (7.1%).
The average biceps-glenoid angle was 87.0° (range, 52.1° to 111.8°; standard deviation [SD], 11.4°) in the subluxation group and 90.0° (range, 67.7° to 129.0°; SD, 9.6°) in the non-subluxation group. There was a statistically significant difference in the biceps-glenoid angle (p = 0.037). The intraobserver reliability for the angle measurement was 0.988, showing a statistically significant correlation (p < 0.001). The intraobserver error was 1 ± 0.5.
In this study, we investigated whether the angle that forms at the intersection of the LHBT and the anterior glenoid can be used as a diagnostic predictor of subluxation of the LHBT. We found that the biceps-glenoid angle was significantly smaller in those with subluxation of the LHBT, but the extent of difference was not large enough to have a statistical significance.
Since the symptoms caused by lesions of the LHBT are inconspicuous, early diagnosis of this pathology through physical examination is difficult in most cases.11) Several tests can be used for the physical examination of the LHBT, such as Yergason's test and Speed's test. However, Holtby and Razmjou12) reported that their sensitivity is low and their specificity is intermediate, limiting their reliability as diagnostic tools.
As a result, it is more common to diagnose lesions of the LHBT as those found concomitantly with other pathologies, rather than as independent entities. A significant number of biceps pathologies are found incidentally through MRI conducted for detection of rotator cuff pathologies. Walch et al.5) found that in 445 patients with rotator cuff tears, 71 (16%) showed subluxation or dislocation of the LHBT. Similarly, Chen et al.8) reported that subluxation of the LHBT was found in 30 of 31 patients (97%) with rotator cuff tears and subscapularis tendon lesions. In addition, Warren13) reported that instability of the LHBT cannot occur without lesions of the subscapularis or of the lesser tuberosity. It is generally agreed that lesions of the LHBT are strongly associated with rotator cuff tears, especially of the subscapularis tendon.
Foad and Wijdicks14) retrospectively evaluated the preoperative MRI of 40 patients who underwent arthroscopic repair of a subscapularis tendon tear and found that 25 patients (62.5%) with a tear were not correctly diagnosed on the preoperative MRI. Subscapularis tendons should be carefully investigated during arthroscopy, since the detection of a subscapularis tendon lesion using preoperative MRI can be difficult. The LHBT should be examined carefully for any lesions during the arthroscopic procedure, along with signs of tendinitis, partial or complete tears, and dislocation. However, it is difficult to discern with certainty during arthroscopy whether the tendon has been displaced from the medial ridge of the bicipital groove in cases of subluxation of the LHBT. Motley et al.9) introduced a ramp test that checks for dislocation of the LHBT by pulling the tendon medio-inferiorly with an arthroscopic probe. The sensitivity and specificity of the ramp test have yet to be determined. Other methods used to determine subluxation or dislocation of the LHBT include an indirect method evaluating the supraglenoid humeral ligament and the coracohumeral ligament, which creates the biceps pulley at the glenoid cavity. However, this approach seems to have many flaws.151617) In our study, the subluxation group on preoperative MRI showed a higher incidence of subscapularis tears, and led to more treatment. Therefore, if subluxation of the biceps is observed on preoperative MRI, one must consider an intraoperative assessment and reparative measures for potential lesions of the subscapularis tendon, in addition to treatment of the biceps tendon. Likewise, when subscapularis tendon tears are observed, the presence of subluxation of the biceps should not be ruled out.
We hypothesized that the presence of subluxation of the LHBT may be predicted by the angle between the LHBT and the glenoid. In an unaffected shoulder, the LHBT runs along the tunnel formed by the bicipital groove and the transverse humeral ligament. It then enters the joint and exits from the proximal bicipital groove, where it changes directions abruptly. However, in a shoulder with subluxation of the LHBT, the transverse humeral ligament becomes injured, and the LHBT shifts medially, leading to a wider turn and a more gradual change in direction as the tendon exits the proximal bicipital groove. We therefore hypothesized that the tendon will connect to the attachment site of the supraglenoid tuberosity with a steeper slope (Fig. 3). As hypothesized, we found that the subluxation group had a mean angle of 87.0° and the non-subluxation group had a mean angle of 90.0°, showing that the angle of tendon attachment to the labrum was indeed smaller. However, the difference in the angle was only 3°, and was deemed clinically insignificant. Therefore, diagnosing subluxation of the LHBT with this angle as a diagnostic marker seems unfeasible. Since subluxation or dislocation in LHBT shows dynamic instability in many cases, it would not be easy to detect during arthroscopic examination even with the biceps-glenoid angle as in our study. Furthermore, the angle measured on the arthroscopic view could have limited value because of variability in the location of a posterior viewing portal and distortion in the visual field or direction of an arthroscopic view. However, if the angle between the LHBT and the glenoid has decreased to less than 90° during subsequent arthroscopic examination, the possibility of subluxation of the LHBT should be kept in mind, especially if the patient already had an injury to the subscapularis tendon.
There are a few limitations to this study, in addition to the inherent weakness of a retrospective design. First, there can be anatomic variations of the biceps anchor in the superior labrum among individuals. Variable tilting and depth of the glenoid fossa may lead to inconsistency in the measurements of the biceps-glenoid angle, and may be problematic if this parameter is used as a marker for LHBT subluxation.
Second, the position and direction of the traction device and the extent of abduction and flexion, which may differ between operations, can influence the biceps-glenoid angle. The resultant changes in the angle that forms between the LHBT and the glenoid will be unavoidable, and will compromise the validity of the marker. In addition, because of the 3-dimensional structure of the LHBT and the glenoid fossa, the angle seen on arthroscopy may differ according to the position of the posterior portal and direction of the arthroscopic view. The issue of reproducibility of the biceps-glenoid angle may place the validity of this marker in question.
Third, even though preoperative MRI was consistently performed with the humerus in neutral rotation, dynamic subluxation or dislocation of the tendon may have occurred. Subsequent ultrasonography to assess mobility of the subluxation is required, and reclassification of the patient groups according to these additional variables may be necessary.18)
Lastly, we could not measure interobserver reliability because only one observer participated in measuring the angles.
In shoulders with subluxation of the biceps tendon on preoperative MRI, more injuries of the subscapularis tendon and biceps pathologies were observed during arthroscopy. However, the arthroscopically-measured biceps-glenoid angle does not have clinical relevance in the determination of subluxation of the LHBT from the bicipital groove.
Figures and Tables
Fig. 1
T1 axial magnetic resonance imaging scans of a 57-year-old female patient without subluxation of the long head of the biceps tendon (A) and a 50-year-old male patient with subluxation (B).
Fig. 2
(A and B) Measurements of the biceps-glenoid angle (red angle) on the arthroscopic view from the posterior portal in the right shoulder without any biceps pathology. The arrows indicate the line connecting superior half of the anterior glenoid. Arthroscopic images of a 63-year-old female patient with subluxation of the long head of the biceps tendon (C) and a 52-year-old female patient without subluxation (D).
Fig. 3
Schematic images of a normal long head of the biceps tendon (A) and subluxated long head of the biceps tendon (B). The biceps-glenoid angle (arrow) in a shoulder with subluxation of the long head of the biceps tendon is steeper than that in a shoulder without subluxation.

Table 1
Demographic Data
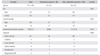
Table 2
Comparison of Intraoperative Findings and Mode of Treatment in the Two Groups
References
1. Hitchcock HH, Bechtol CO. Painful shoulder; observations on the role of the tendon of the long head of the biceps brachii in its causation. J Bone Joint Surg Am. 1948; 30A(2):263–273.
2. Gerber C, Sebesta A. Impingement of the deep surface of the subscapularis tendon and the reflection pulley on the anterosuperior glenoid rim: a preliminary report. J Shoulder Elbow Surg. 2000; 9(6):483–490.

3. Kim YK, Kim DW, Lee JH. Long head of the biceps tendon lesion associated with rotator cuff tear. J Korean Shoulder Elbow Soc. 2010; 13(1):64–71.

4. Shi LL, Mullen MG, Freehill MT, Lin A, Warner JJ, Higgins LD. Accuracy of long head of the biceps subluxation as a predictor for subscapularis tears. Arthroscopy. 2015; 31(4):615–619.

5. Walch G, Nove-Josserand L, Boileau P, Levigne C. Subluxations and dislocations of the tendon of the long head of the biceps. J Shoulder Elbow Surg. 1998; 7(2):100–108.

6. Gambill ML, Mologne TS, Provencher MT. Dislocation of the long head of the biceps tendon with intact subscapularis and supraspinatus tendons. J Shoulder Elbow Surg. 2006; 15(6):e20–e22.

7. Cho CH, Lee KJ, Bae KC. Isolated medial dislocation of the long head of the biceps without rotator cuff tear: a case report. J Korean Orthop Assoc. 2008; 43(5):655–658.

8. Chen CH, Hsu KY, Chen WJ, Shih CH. Incidence and severity of biceps long head tendon lesion in patients with complete rotator cuff tears. J Trauma. 2005; 58(6):1189–1193.

9. Motley GS, Osbahr DC, Holovacs TF, Speer KP. An arthroscopic technique for confirming intra-articular subluxation of the long head of the biceps tendon: the ramp test. Arthroscopy. 2002; 18(9):E46.

10. Yoo JC, Rhee YG, Shin SJ, et al. Subscapularis tendon tear classification based on 3-dimensional anatomic footprint: a cadaveric and prospective clinical observational study. Arthroscopy. 2015; 31(1):19–28.

11. Murthi AM, Vosburgh CL, Neviaser TJ. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. 2000; 9(5):382–385.

12. Holtby R, Razmjou H. Accuracy of the Speed's and Yergason's tests in detecting biceps pathology and SLAP lesions: comparison with arthroscopic findings. Arthroscopy. 2004; 20(3):231–236.

13. Warren RF. Lesions of the long head of the biceps tendon. Instr Course Lect. 1985; 34:204–209.
14. Foad A, Wijdicks CA. The accuracy of magnetic resonance imaging and magnetic resonance arthrogram versus arthroscopy in the diagnosis of subscapularis tendon injury. Arthroscopy. 2012; 28(5):636–641.

15. Baumann B, Genning K, Bohm D, Rolf O, Gohlke F. Arthroscopic prevalence of pulley lesions in 1007 consecutive patients. J Shoulder Elbow Surg. 2008; 17(1):14–20.

16. Bennett WF. Arthroscopic bicipital sheath repair: two-year follow-up with pulley lesions. Arthroscopy. 2004; 20(9):964–973.

17. Werner A, Ilg A, Schmitz H, Gohlke F. Tendinitis of the long head of biceps tendon associated with lesions of the “biceps reflection pulley”. Sportverletz Sportschaden. 2003; 17(2):75–79.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download