Abstract
Background
Access to early knee osteoarthritis treatment in low and middle income nations is often believed to be limited. We conducted a cross-sectional study in India to assess prior access to treatment among patients presenting with knee pain to specialist orthopaedic clinics.
Methods
The multi-centre, cross-sectional study included patients presenting with knee pain at 3 hospitals in India. Patients who met the inclusion criteria and provided informed consent completed a questionnaire designed to assess patient demographics, socioeconomic status, knee pain, treatment method, and patient's knowledge on osteoarthritis (OA). Their orthopaedic surgeons also completed a questionnaire on the severity of patient's OA and their recommended treatments. The impact of demographic characteristics on the prescription of treatment options was analyzed using logistic regression.
Results
A total of 714 patients met the eligibility criteria and participated in this study. The majority of patients had been experiencing pain for less than 1 year (64.8%) and had previously been prescribed medications (91.6%), supplements (68.6%), and nonpharmacological (81.9%) treatments to manage their knee OA. Current treatment recommendations included oral medications (83.3%), intra-articular injections (29.8%), and surgical intervention (12.7%). Prescription of oral medications was related to younger age, lack of deformities, and lower Kellgren-Lawrence grades (p < 0.01). Patients treated in private hospital settings were more likely to have been previously treated with medications (range, 84.3% to 92.6%; p < 0.01) and physical treatments (range, 61.8% to 84.8%; p < 0.01) than patients treated at government hospitals.
Osteoarthritis (OA) is one of the most common forms of musculoskeletal diseases worldwide.1) It is estimated that 3.8% of the world's population suffer from symptomatic knee OA,2) which equates to approximately 277 million people living with knee OA worldwide.3) The prevalence of OA is similar across the globe2) and it is expected to increase dramatically as the population ages, especially in low and-middle income nations.45) The prevalence of knee OA in rural and urban India is estimated to be 3.9% and 5.5%, respectively.26)
OA is a progressive, irreversible disease for which there is no cure. Treatment of OA in North America generally focuses on symptom management, with a hope of improving knee function, which eventually requires knee replacement surgery as the disease progresses.5) Treatment typically includes a combination of pharmaceutical interventions (i.e., analgesics and anti-inflammatories), natural supplements, and intra-articular injections of corticosteroids or hyaluronic acid (HA) in addition to active treatment (i.e., physical therapy, exercises, orthotics, or manual therapy aimed at improving strength and mobility).5) As knee OA advances and conservative treatments are no longer effective for alleviating symptoms, surgical procedures become necessary.
In low and middle income nations, such as India, access to appropriate treatment is often limited and depends upon accessibility of healthcare services, insurance, availability of different treatment options, and the ability of the patient to pay for health care.7) Little is known about access to treatment of OA in India and the factors associated with presenting to specialist care for consideration of surgical management. We, therefore, conducted a national cross-sectional study across three clinical sites in India to assess prior access to treatments among patients presenting with knee pain at specialist orthopaedic clinics. We examined the characteristics of patients, severity of OA, and treatment recommendations and explored predictors of accessing various treatments and the impact of private and public hospital system on access to care. We hypothesized that patients presenting with knee pain would have had limited access to care, have a higher severity of disease, be recommended nonsurgical care, and there would be numerous factors that predict access to treatment, including being treated in a private hospital.
We conducted a multi-centre, cross-sectional study that included patients presenting with knee pain at three hospitals in India. Patients who met the inclusion criteria and provided informed consent completed a questionnaire designed to assess patient demographics, socioeconomic status, knee pain and treatment method, and their knowledge about OA. Their orthopaedic surgeons completed a questionnaire on the severity of patient's OA and their recommended treatments. Prior to initiation of the study, approval was obtained for the overall study from the Institutional Review Board Services and the Research Ethics Board at each participating hospital. Informed consent was received from all participants prior to participation in the study. This study was performed in accordance with the Declaration of Helsinki.
The questionnaire was developed by the authors for the purpose of this study by using the current literature and input from content experts. The questionnaire was reviewed by 10 orthopaedic surgeons and research methodologists for face and content validity. In addition, 10 Indian orthopedic surgeons reviewed the questionnaire for cultural sensitivities and identified any questions that they believed would cause a problem for the patient, the attending physician, and/or the research coordinator. This approach helped to ensure that all questions were worded adequately and were culturally relevant and appropriate.
The questionnaire included 5 sections and 31 items. The first section included 10 demographic questions. The second section asked the patient about their affected knee and included questions on their diagnosis, level of pain, and functional limitations. The questionnaire also included a section that asks the patient how their knee OA was managed in the past (i.e., medications, supplements, braces, physiotherapy, etc.). Their surgeon completed the remaining 2 sections which included questions on the severity of OA (6 questions) as well as their recommended treatments (3 questions). Prior to initiating the study, the questionnaire was reviewed by 10 orthopaedic surgeons and research methodologists for face and content validity, and then was reviewed by 10 Indian orthopedic surgeons for cultural sensitivities. This approach helped to ensure that all questions were worded adequately and were culturally relevant and appropriate.
Three hospitals in India were selected to participate in the study based upon patient volume, research infrastructure, and interest in the study. The clinical sites included 1 government and 2 private hospitals.
The study had minimal exclusion criteria. The inclusion criteria were: (1) at least 18 years of age; (2) presence of knee pain; (3) patient's ability to understand and complete the questionnaire; and (4) patient's agreement to participate in the study. The exclusion criteria included: (1) a history of total knee arthroplasty (TKA); (2) an open wound or evidence of recent surgery in the affected knee; (3) a current or history of tumour in the affected knee or proximal skeletal structure; and (4) a current or history of fracture in the tibial plateau, femoral condyle, or patella.
After providing informed consent, study participants completed the questionnaire under research coordinator's supervision. The questionnaire took approximately 10 minutes to complete. The participant's surgeon then completed their section of the questionnaire. The research coordinator at the clinical site then checked each questionnaire for completeness and entered the questionnaire into the study's electronic data capture system.
Descriptive statistics for continuous variables are presented as means with standard deviations, and categorical variables are presented as proportions. The primary outcome was the recommended treatment reported as a categorical variable. The impact of demographic characteristics on the prescription of treatment options was analyzed using logistic regression.
A total of 807 patients were screened for participation in this study across the hospitals, of which 93 were deemed ineligible to participate in the study. The reasons for ineligibility included previous history of TKA in the affected knee (91 patients) and a fracture of the tibial plateau, femoral condyle, or patella (2 patients). Ultimately, 714 patients met the eligibility criteria and participated in this study.
The mean age of the included patients was 55.6 years (Table 1). The majority of patients were female (63.9%) and lived in urban locations (89.2%). The mean body mass index (BMI) was 25.6 kg/m2. Most patients made less than Rs300,000 (approximately $4,660) annually (62.2%) and did not have health insurance (69.3%). Approximately half of the patients had a comorbid disease at the time of the assessment (54.2%). Common comorbidities included hypertension (40.8%), diabetes (24.4%), and osteoporosis (11.8%) Table 1. Demographics were similar between the government and private hospitals; however, government hospitals had more rural patients and patients with lower incomes (p < 0.01).
The majority of patients presenting with knee pain had been experiencing pain for less than 1 year (64.8%) (Table 2). Two-thirds of the study participants had bilateral knee pain (66.0%). Over half of the patients (62.3%) had been previously diagnosed with knee OA by a clinician, and most had received this diagnosis within the past year (62.2%). Kellgren-Lawrence (K-L) grades 1 and 2 were most common with 35.0% and 31.1% of patients falling in these categories, respectively. Approximately one third of the patients had deformities of the knee (33%), with 32.2% of all patients having a varus deformity. Patients presenting to government hospitals were 2.3 times more likely to have suffered from knee pain for more than 6 years than patients presenting to a private hospital (p < 0.01).
The majority of patients had previously been prescribed medications (91.6%), supplements (68.6%), and nonpharmacological (81.9%) treatments to manage their knee OA (Table 2). The most commonly used medical treatments were nonsteroidal anti-inflammatory drugs (69.0%) and topical agents (59.2%). Commonly used supplements included vitamins (35.6%), glucosamine (26.2%), and chondroitin (14.8%). Over half of the patients had previously received treatment from physiotherapists (55.2%). There were multiple differences in the previous management of knee OA between the patients treated at a private hospital and those at a government hospital (Table 2). For example, patients at private hospitals were more likely than patients at government hospitals to have been previously treated with medications (range, 84.3% to 92.6%; p < 0.01) and physical treatments (range, 61.8% to 84.8%; p < 0.01). Table 3 summarizes the reported levels of knee pain and functional limitations between patients presenting to government and public hospitals.
At the current clinic visit, almost all patients received a treatment recommendation for their knee OA (97.8%) (Table 4). Physicians frequently prescribed oral medications (83.3%) whereas intra-articular injections of either HA or corticosteroids were recommended less frequently (29.8%). Surgical management was recommended to 13.2% of patients, which included TKA (98.9% of recommended surgeries) and unicompartmental knee arthroplasty (1.1% of recommended surgeries). The most common reasons for not recommending surgery were that the patient's OA was too mild (44.4%) and that the clinician prescribed medications or physiotherapy instead (32.1%). Overall, approximately 10% of patients lacked resources to pay for arthroplasty: 8.8% of patients at private hospitals lacked the resources to pay for surgery compared to 18.8% of patients at government hospitals (p < 0.01). Surgeons were also asked if they would consider an implantable joint-unloading prosthesis as an alternative treatment, and approximately half (49.2%) of surgeons felt it would be an acceptable alternative. At the time of their clinic visit, over half of the surgeons (56.2%) indicated that they would also consider other surgical options such as knee realignment surgery.
Prescription of oral medications was related to younger age, lack of deformities, and lower K-L grades (p < 0.01) (Table 5). Intra-articular injection prescription was associated with the patient having health insurance (p < 0.01). The recommendation of surgical interventions (realignment surgery) and TKA was related to higher K-L grades (p < 0.01). Increased prescription of oral medications in government hospitals approached statistical significance (p = 0.0232), whereas the increased likelihood of a surgeon to prescribe surgery in private hospitals approached statistical significance (p = 0.0171).
Our findings suggest early knee OA care in India is similar to that in North America. Interesting similarities and differences are evident when we compare the treatment recommendation data in India collected for the current study with that published in a recent study of 537 patients who presented with knee OA to an orthopaedic service in the United States.8) In the present study, 83.3% of patients in India were prescribed oral medications, which is highly comparable to 82.1% using any form of pain medication for the treatment of knee OA in the US.8) When comparing intra-articular injections, 55.4% of US patients had received injections while in the present study only 29.8% of patients in India were prescribed knee injections.8) In the current study, surgeons recommended that 12.7% of patients receive surgical management of their knee OA, which is comparable to patients presenting with consistent knee pain in the US, where 8.8% received TKA.9)
The majority of patients included in this large cross-sectional study had been experiencing knee pain for less than a year and had a K-L grade of 1 or 2. Almost all patients had previously been treated with medications (91.6%) and/or some form of nonpharmacological treatment (81.9%). Over two-thirds (69.3%) of the patients did not have medical insurance. This suggests that patients in India are being seen by a specialist and are receiving medical care in the early stages of OA, which goes against the common perception that patients in India do not receive medical treatment for early stage OA and thus eventually present with advanced stages of OA.
Several important differences were found between private and government hospitals. As expected, government hospitals saw more rural patients and patients with lower incomes (p < 0.01). Patients presenting to government hospitals were 2.3 times more likely to have suffered from knee pain for more than 6 years than patients presenting to a private hospital (p < 0.01). At private hospitals, 8.8% of patients lacked the resources to pay for surgery compared to 18.8% of patients at government hospitals (p < 0.01). The prescription of oral medications and surgical intervention both approached statistical significance when compared between 2 hospital types: patients at government hospitals were more likely to be prescribed oral medications and patients at private hospitals were more likely to be recommended for surgical management. Patients at private hospitals were more likely to be recommended for surgery despite knee pain that lasted for a shorter period of time, which may suggest a disparity in the management of OA between private and public hospitals. When exploring relationships between demographic variables and prescribed treatments for patients, several associations were identified. Firstly, the prescription of oral medications was associated with younger age, the absence of deformities, and lower K-L grades, which is consistent with current treatment recommendations.10) Secondly, the prescription of intra-articular injections was related to patients having insurance coverage as opposed to no coverage. The higher prescription rate of intra-articular injections to patients with health insurance is likely be related to the high cost of injections, and clinicians may be less willing to prescribe the intervention to patients who are paying for the treatment themselves.11) Thirdly, the prescription of surgical interventions was associated with higher K-L grades, which is also consistent with treatment guidelines and signifies that surgical intervention is not considered as an option unless severe OA is present.10)
This study is limited by the context of the study design. The present study is a cross-sectional evaluation of patient demographics and treatment decisions, which is useful for identifying relationships between variables but not for determining outcomes or causality.12) The utilization of a cohort study to examine outcomes of treatment options based on demographic information may be valuable for examination in future research. Also, the results of this study are limited to patients with OA in India, and may not be generalizable to other low and middle income nations. The results are further limited by the inclusion of patients only presenting with knee pain, and may not be generalizable to patients with other knee-related injuries. Moreover, another possible limitation was the inclusion of 5 participants with a K-L grade of 0, as knee pain in these participants may have been due to another pathology including anterior knee pain syndrome or a meniscus tear. However, in all 5 cases, the attending surgeon diagnosed low grade OA despite minimal radiological changes. Lastly, we used a nonvalidated questionnaire with our own criteria to assess levels of pain and functional limitations. Additionally, weight reduction was not included as a nonpharmacological intervention in the questionnaire. However, this study is strengthened by the large sample size, inclusion of the three clinical sites in India, rigorous development of the study questionnaire, and high quality data collection.
In conclusions, this large cross-sectional study found that most patients in India are receiving early medical management of OA despite not having insurance and that the treatment patterns are similar to those seen in the US. In addition, key differences were identified between treatment in government and private hospitals, which may lead to a discrepancy in care.
References
1. Wieland HA, Michaelis M, Kirschbaum BJ, Rudolphi KA. Osteoarthritis: an untreatable disease? Nat Rev Drug Discov. 2005; 4(4):331–344. PMID: 15803196.
2. Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014; 73(7):1323–1330. PMID: 24553908.

3. U.S. Census Bureau. International data base [Internet]. Washington, DC: U.S. Census Bureau;2016. cited 2015 Sep 3. Available from: http://www.census.gov/population/international/data/idb/region.php?N=%20Results%20&T=13&A=both&RT=0&Y=2015&R=1&C=.
4. Population Foundation of India. Population Reference Bureau. The future population of India: a long-range demographic view [Internet]. Delhi, India: Ajanta Offset & Packagings Ltd.;2007. cited 2015 Sep 3. Available from: http://www.prb.org/pdf07/futurepopulationofindia.pdf.
5. Das SK, Farooqi A. Osteoarthritis. Best Pract Res Clin Rheumatol. 2008; 22(4):657–675. PMID: 18783743.

6. Haq SA, Davatchi F. Osteoarthritis of the knees in the COPCORD world. Int J Rheum Dis. 2011; 14(2):122–129. PMID: 21518310.

7. Dutta S, Lahiri K. Is provision of healthcare sufficient to ensure better access? An exploration of the scope for publicprivate partnership in India. Int J Health Policy Manag. 2015; 4(7):467–474. PMID: 26188811.
8. Allen KD, Bosworth HB, Chatterjee R, et al. Clinic variation in recruitment metrics, patient characteristics and treatment use in a randomized clinical trial of osteoarthritis management. BMC Musculoskelet Disord. 2014; 15:413. PMID: 25481809.

9. Wise BL, Felson DT, Clancy M, et al. Consistency of knee pain and risk of knee replacement: the Multicenter Osteoarthritis Study. J Rheumatol. 2011; 38(7):1390–1395. PMID: 21498481.

10. Sinusas K. Osteoarthritis: diagnosis and treatment. Am Fam Physician. 2012; 85(1):49–56. PMID: 22230308.
11. Wen DY. Intra-articular hyaluronic acid injections for knee osteoarthritis. Am Fam Physician. 2000; 62(3):565–572. PMID: 10950213.
12. Mann CJ. Observational research methods: research design II: cohort, cross sectional, and case-control studies. Emerg Med J. 2003; 20(1):54–60. PMID: 12533370.

Table 1
Patient Characteristics
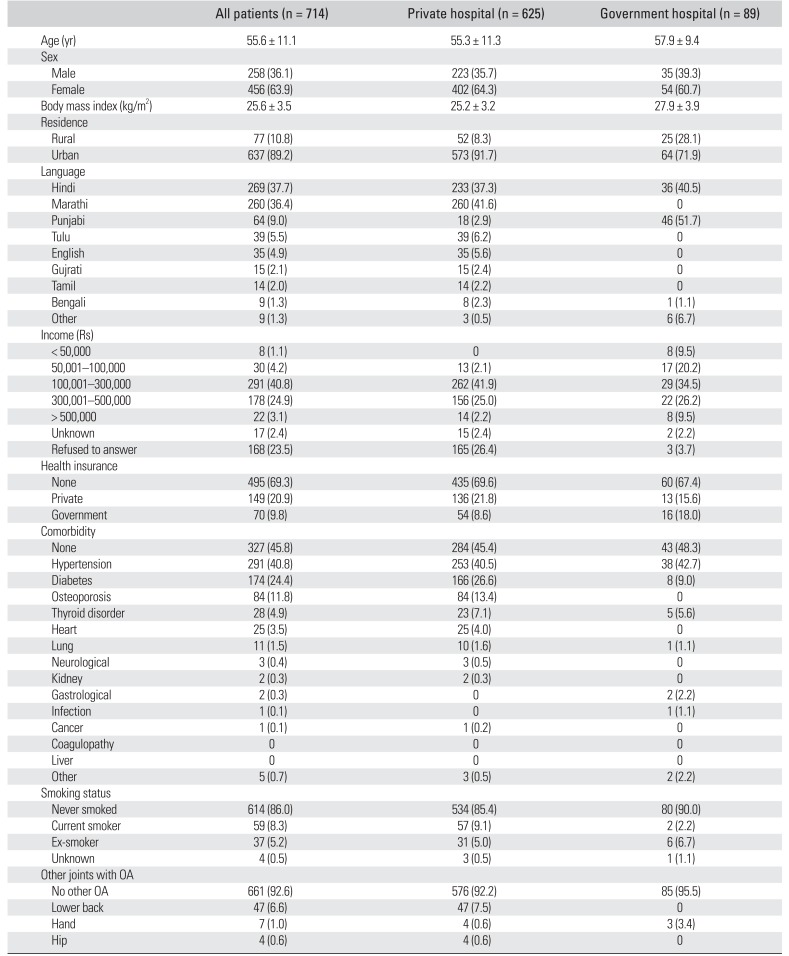
Table 2
Disease Characteristics
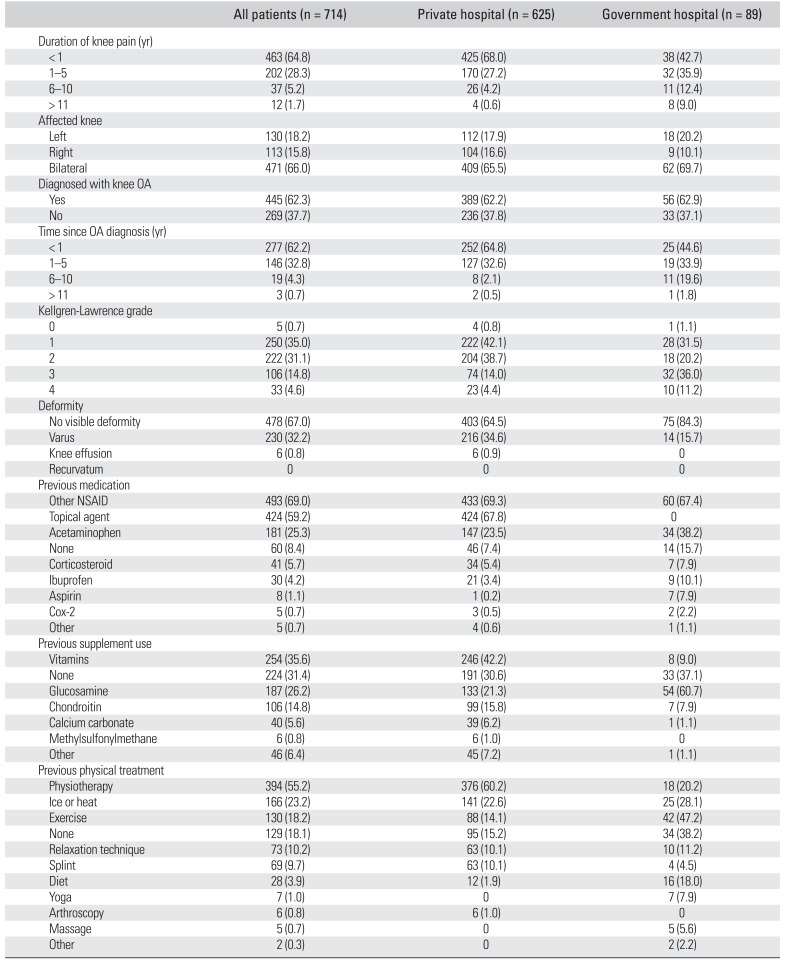
Table 3
Level of Pain and Functional Limitation
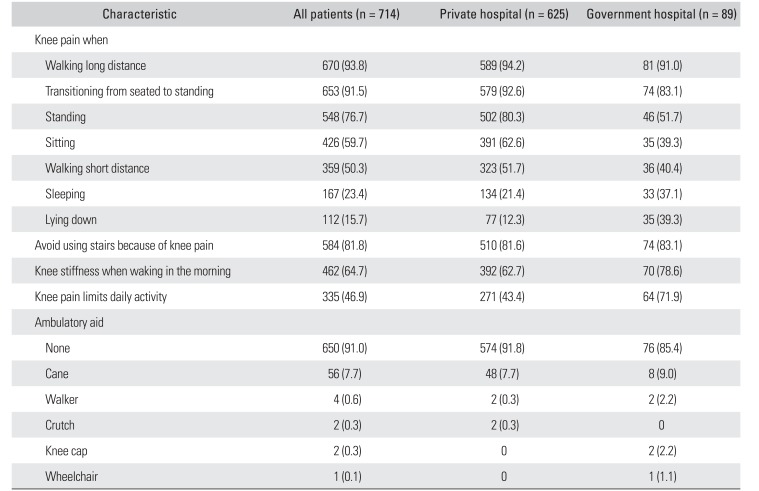
Table 4
Prescribed Treatment
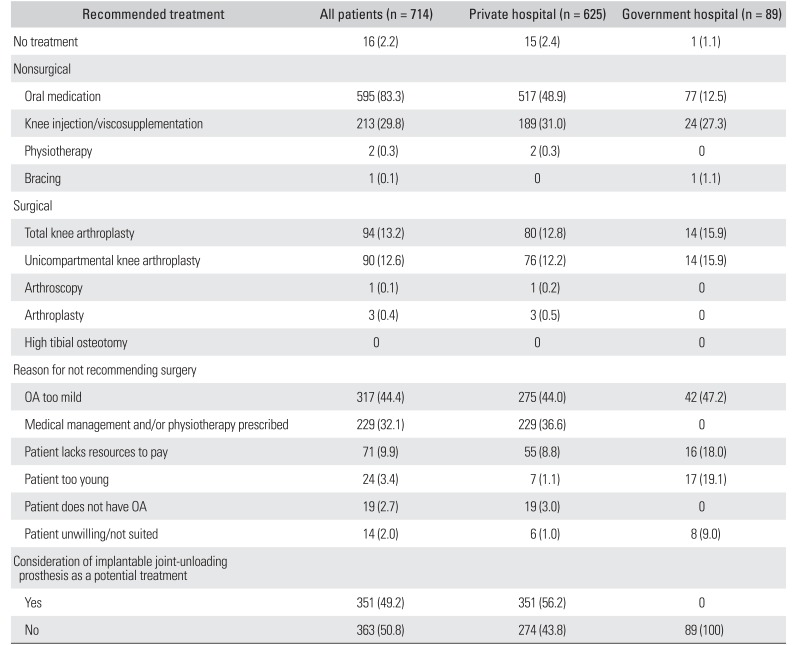
Table 5
Treatment Decisions and Related Variables
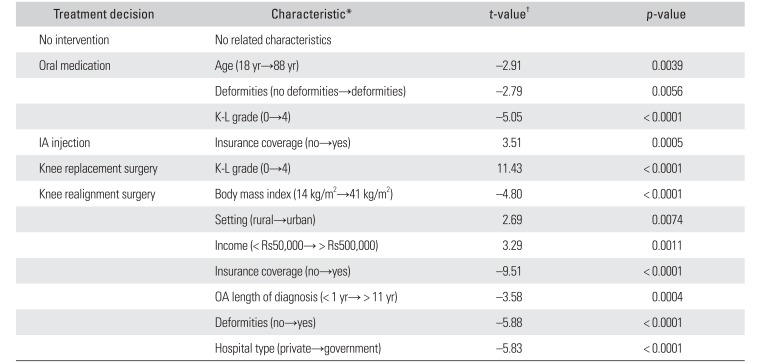
IA: intra-articular, K-L: Kellgren-Lawrence.
*Only significant characteristics are shown for each treatment decision. †Positive t-value indicates increased likelihood of prescription of treatment along the respective characteristic. Negative t-value indicates decreased likelihood of prescription of treatment along the respective characteristic.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download