Abstract
Background
The purpose of this study was to compare the clinical and radiological results of 2 different tibial fixations performed using bioabsorbable screws with added hydroxyapatite (HA) and pure poly-L-lactic acid (PLLA) screws in anterior cruciate ligament (ACL) reconstruction.
Methods
A total of 394 patients who underwent arthroscopic ACL reconstruction between March 2009 and June 2012 were retrospectively reviewed. Of those, 172 patients who took the radiological and clinical evaluations at more than 2 years after surgery were enrolled and divided into 2 groups: PLLA group (n = 86) and PLLA-HA group (n = 86). Both groups were assessed by means of the Lysholm score, International Knee Documentation Committee (IKDC) subjective knee score, and Tegner activity score. Stability was evaluated using the KT-2000 arthrometer. Magnetic resonance imaging was performed to evaluate tibial tunnel widening, screw resorption, osteoingeration, and foreign body reactions.
Results
The PLLA-HA group showed significant reduction in the extent of tibial tunnel widening and foreign body reactions and significant increase in screw resorption compared to the pure PLLA group (p < 0.001 for both). In contrast, postoperative Lysholm score, Tegner activity score, IKDC score, and side-to-side difference on the KT-2000 arthrometer showed no significant differences between groups (p = 0.478, p = 0.906, p = 0.362, and p = 0.078, respectively). The PLLA group showed more significant widening in the proximal tibial tunnel than the PLLA-HA group (p = 0.001). In the correlation analysis, proximal tibial tunnel widening revealed a positive correlation with knee laxity (r = 0.866) and a negative correlation with Lysholm score (r = −0.753) (p < 0.01 for both).
Conclusions
The HA added PLLA screws would be advantageous for tibial graft fixation by reducing tibial tunnel widening, improving osteointegration, and lowering foreign body reactions. Even though no clinically significant differences were noted between the pure PLLA group and PLLA-HA group, widening of the proximal area of the tibial tunnel showed a tendency to increase knee laxity measured using the KT-2000 arthrometer.
In arthroscopic anterior cruciate ligament (ACL) reconstruction, it is important to make tibial and femoral tunnel entrances in the anatomic locations. While much focus has been placed on the femoral tunnel position, considerably less attention has been given to the tibial tunnel position.1) Bedi et al.2) reported that more anterior placement of the tibial tunnel from the posterolateral bundle to the anteromedial bundle significantly reduced anterior tibial translation and rotational instability. More anterior placement of the tibial tunnel than the conventional may increase the risk of shallow tunnel creation below the tibial cortex.3) Especially in the transtibial technique, formation of the femoral tunnel in the anatomical position requires the tibial tunnel entrance to be moved near medial and articular surface, which leads to a mismatch between the graft and the tunnel due to reduction of the tibial tunnel length, damage to the medial collateral ligament and pes anserinus, and insufficient spare bone stock due to the shallow tunnel in the tibial plateau.4) If tibial tunnel widening occurs due to conditions such as osteolysis, the tibial bone becomes vulnerable to physical stress, which leads to graft fixation failure and increased possibility of reoperation.5) Therefore, in order to reduce these risks and minimize tibial tunnel widening, selecting a proper graft fixation device is important.1)
Recently, the use of bioabsorbable interference screws is increasing in graft fixation, since they are easier to remove than metallic interference screws and show lower diffraction rates during magnetic resonance imaging (MRI).67) Early bioabsorbable interference screws consisted only of a polymer such as poly-L-lactic acid (PLLA) or polyglycolic acid. They were vulnerable to dangers such as failure to convert to bone substitution after disintegration, increase of delayed inflammation reactivity due to delayed disintegration and absorption within the body, and emergence of a bone cyst lesion due to oxides.8) In order to increase absorption rates of bioabsorbable screws, enhance osteogenesis after absorption, and reduce oxidation, bioabsorbable screws with added calcium phosphate, such as hydroxyapatite (HA), β-tricalcium phosphate (β-TCP), or calcium carbonate have been developed.910) Bioabsorbable screws with added calcium phosphate have been considered more advantageous than other composite materials as well as pure PLLA screws, since they speed graft incorporation, show abundant conversion to cancellous bone, and decrease acidity while acting as a buffer for PLLA decomposition product.91011) Yet there have been few articles that comprehensively analyze the difference of clinical results and the extent of tunnel widening between pure PLLA screws and PLLA/HA blend (PLLA-HA) screws, especially in ACL reconstruction performed using the same surgical technique at a single institution.
The purpose of this study was to compare the clinical and radiological results of ACL reconstruction performed using HA added bioabsorbable screws and pure PLLA screws for tibial graft fixation. We hypothesized that the PLLA-HA screws would result in less tibial tunnel widening, improved osteointegration, and better clinical results.
Medical records of 394 patients who underwent primary ACL reconstruction performed using the same technique by a single surgeon (JGK) in the same hospital from March 2009 to June 2012 were obtained. The inclusion criteria for this study were primary ACL reconstruction, unilateral ACL reconstruction, a minimum 2-year follow-up, and availability for MRI at 24 months postoperatively. Patients were excluded if they had ipsilateral fractures, multiple ligament injuries, infection, reoperation due to complications, chondral lesions requiring treatment, contralateral injuries, and any previous knee surgery. Based on these selection criteria, a total of 172 patients were included in the study (Fig. 1): 86 patients underwent ACL reconstruction using PLLA bioabsorbable interference screws (BioRCI, Smith and Nephew, Andover, MA, USA; PLLA group) and the other 86 patients underwent the same procedure using the PLLA-HA screws (BioRCI-HA, Smith and Nephew; PLLA-HA group). The patients in the PLLA-HA group were matched for age, sex, and preoperative sports activity level with those in the PLLA group (Table 1). The study protocol was approved by Inje University Seoul Paik Hospital Institutional Review Board (No. IIT-2012-187).
All reconstructions were performed with a modified transtibial technique using a quadruple hamstring tendon autograft.12) Through the anteromedial portal, a microfracture awl was placed just behind the bifurcate ridge to make the center of the anatomical femoral tunnel. The triangular, funnel-shaped bony trough was employed to slip the eccentrically positioned guide into the anticipated anatomic center, which is part of the modified transtibial technique.12) An ACL guide (Linvatec, Largo, FL, USA) was used to make the tibial tunnel at an angle of 47.5°, and the tunnel was positioned in the center of the remnant ACL stump. The tibial tunnel was made to have the same thickness as the graft using an expansion reamer. The guide pin was inserted into the tibial tunnel towards the preformed funnel-shaped bone trough with a free-hand technique. The femoral tunnel was made to have the same thickness as the graft using an expansion reamer. After the graft passage, femoral fixation was done with Endobutton (Endobutton; Smith and Nephew). Tibial fixation was performed with a bioabsorbable interference screw and an additional cortical bone screw with washer at 15° of knee flexion. The diameter of the bioabsorbable screw was the same size as the graft. A pure PLLA screw (BIORCI; Smith and Nephew) was used in the PLLA group and a HA-added PLLA screw (BIORCI-HA; Smith and Nephew) in the PLLA-HA group.
The same postoperative rehabilitation was conducted in both groups. Patients were permitted to bear weight with an ACL support device and to start range of motion exercises as tolerated immediately after surgery based on our accelerated rehabilitation program. In knees with meniscus repair, partial weight bearing with crutch was performed for 6 weeks. Sports activities were allowed 6 months after surgery after completion of home-based rehabilitation.
Lysholm score, International Knee Documentation Committee (IKDC) subjective knee score, Tegner activity score, and KT-2000 (MEDmetric, San Diego, CA, USA) side-to-side difference were assessed preoperatively, 3, 6, and 12 months after surgery, and once a year thereafter.
At least 24 months after surgery, MRI was performed using a 1.5-T MRI scanner (Intera Achieva; Philips, Eindhoven, The Netherlands) to obtain cross-sectional images perpendicular to the long axis of the tibial tunnel, on which the cross-sectional area (CSA) of the tunnel was measured.1314) Using Picture Archiving and Communication System (Maroview ver. 5.4; MAROTECH Inc., Seoul, Korea), boundaries of the tunnel were traced and the automatically calculated CSA was used for assessment (Fig. 2).14) The tibial tunnel was measured in the proximal (0.5 cm below the articular surface), middle, and distal (0.5 cm from the distal tibial tunnel entrance) parts.1315) The original CSA was calculated with the diameter of the bioabsorbable screw used during surgery. The increase in CSA was calculated by subtracting the original CSA from the CSA at follow-up and dividing it by the original CSA. The value was presented in percentage.1314) Two orthopedic surgeons (DWL and JHP) measured the values every 2 weeks and calculated the average values.
In addition to the tunnel widening value, degradation and osteointegration of the bioabsorbable screw and foreign body reactions within the tunnel were checked.1116171819) The resorption rate of the bioabsorbable screw was calculated with the following formula:16)
The signal quality of the bone tunnel-screw-graft system was evaluated to estimate the degree of osteointegration of the screw on T2-weighted images,1119) and was classified as good (no signal change at the bone/screw interface), partial (a signal change in < 33% of the interface), some (incomplete integration with a signal change in 33% to 67%), and little (no osteointegration with a signal change in > 67%) (Fig. 3).1820) The foreign body reactions were classified as no reaction, edema (high signal in the bone surrounding the tibial tunnel), or cyst (sac-like structure) formation on T2-weighted images (Fig. 4).21)
All statistical analysis was done using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA), and p < 0.05 was considered statistically significant. The independent t-test was used to compare Lysholm score, IKDC score, side-to-side difference on the KT-2000 arthrometer, and other numerical data between the 2 groups. The Mann-Whitney U-test was used to compare Tegner activity score and other non-parametric variables. The paired t-test and Wilcoxon signed-rank test were used to compare preoperative and postoperative data between the groups. Either the chi-square test or Fisher exact test was used to compare categorical data. The Spearman correlation coefficient was used to analyze the relationship of screw resorption, osteointegration, foreign body reaction, and tibial tunnel widening. The Pearson correlation coefficient was used to characterize the relationship of tibial tunnel widening and joint laxity evaluated by the KT-2000 arthrometer. Intraclass correlation coefficients (ICCs) were calculated to determine intraobserver and interobserver reliability of the measurement of tibial tunnel widening on MRI. Power analyses were based on the following estimation of standard deviation: 20% for tibial tunnel widening and 30 points for Lysholm score. These enabled us to detect a difference of 10% or greater for tunnel widening and 15 points or greater for Lysholm score with a power of 90.64% between the 2 groups including 86 patients each.
Preoperative characteristics of the patients are presented in Table 1.
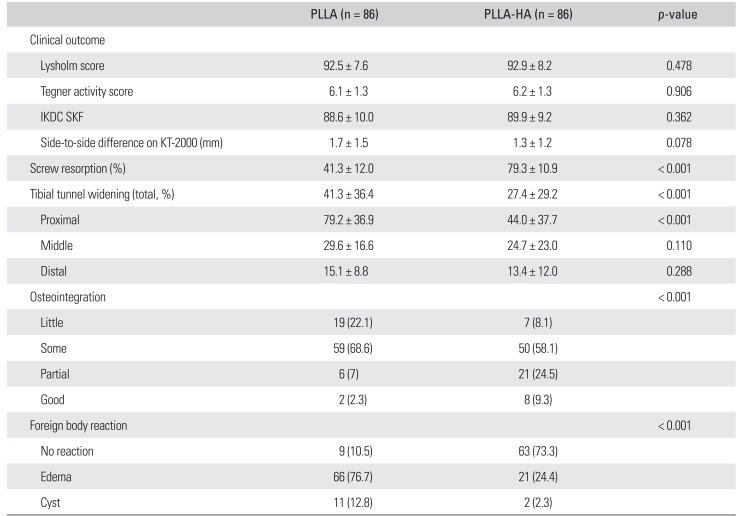
The mean follow-up period for clinical and MRI evaluations was 32.5 and 27.2 months, respectively, for the PLLA group and 31.0 and 26.8 months, respectively, for the PLLA-HA group (p = 0.123 and p = 0.519). Both groups showed significant improvement in the clinical outcomes (p < 0.001) (Tables 2 and 3). The side-to-side difference on KT-2000 arthrometer was significantly improved in both groups (p < 0.001) (Tables 2 and 3). There were no statistically significant differences in postoperative Lysholm score, Tegner activity score, IKDC SKF, and side-to-side difference on the KT-2000 testing between 2 groups (p = 0.478, p = 0.906, p = 0.362, and p = 0.078, respectively).
The mean increase in the tibial tunnel CSA on the follow-up MRI was 27.4% in the PLLA-HA group, and 41.3% in the PLLA group. There was a statistically significant intergroup difference in the CSA increase in the proximal area of the tibial tunnel (p < 0.001) (Table 2). The intraobserver ICC for tibial tunnel widening on MRI was 0.972 (95% confidence interval [CI], 0.928 to 0.991), and the interobserver ICC was 0.994 (95% CI, 0.982 to 0.998). The screw resorption rate was about 38% higher in the PLLA-HA group (p < 0.001). The PLLA-HA group showed better osteointegration (Table 2). Foreign body reactions including edema or cyst formation were observed on MRI in 89.5% of the patient in the PLLA and in 26.7% in PLLA-HA (p < 0.001) (Table 2).
We analyzed the correlation of tibial tunnel widening on MRI with knee laxity evaluated by the KT-2000 arthrometer, and Lysholm score. Although, there were no statistically significant differences in the KT-2000 arthrometer and Lysholm scores between 2 groups, the PLLA group showed more significant widening in the proximal area of the tibial tunnel than the PLLA-HA group. Sixty-nine (80%) patients in the PLLA group showed tibial tunnel widening more than 50% (Fig. 5), their mean Lyshom score was 87.1 ± 9.2, and postoperative KT-2000 side-to-side difference was 2.5 ± 1.6 mm. The Lysholm score and postoperative KT-2000 side-to-side difference were 96.3 ± 5.3 and 0.6 ± 0.3 mm, respectively, in patients in the PLLA group with tibial tunnel widening less than 50%, which were statistically significantly different from patients with tibial tunnel widening more than 50% in the same group (p < 0.001). Thirty-two (37%) patients in the PLLA-HA group showed more than 50% increase in the tibial tunnel. Their mean Lyshom score was 90.7 ± 7.1 and postoperative KT-2000 side-to-side difference was 2.0 ± 1.7 mm. The Lysholm score and postoperative KT-2000 side-to-side difference were 97.5 ± 2.0 and 0.4 ± 0.3 mm, respectively, in patients with tunnel widening less than 50% in the same group, showing statistically significant differences from patients with tibial tunnel widening more than 50% in the same group (p < 0.001). Among all patients, 101 patients (59%) showed tibial tunnel widening more than 50%. Their mean Lyshom score was 90.8 ± 7.8 and postoperative KT-2000 side-to-side difference was 2.2 ± 1.6 mm. The Lysholm score and postoperative KT-2000 side-to-side difference were 94.6 ± 5.3 and 0.5 ± 0.3 mm, respectively, in the other patients with tibial tunnel widening less than 50%, showing statistically significant difference from those with tibial tunnel widening more than 50% (p < 0.001).
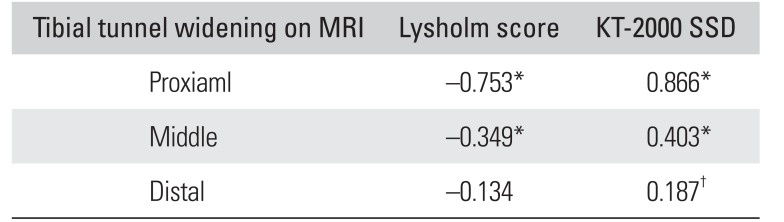
On the correlation analysis, widening of the proximal tibial tunnel was found to be significantly correlated with screw resorption, osteointegration, and foreign body reactions (Table 3).
In the overall trend analysis, the increase in the proximal area of the tibial tunnel revealed a positive correlation with knee laxity, and a negative correlation with Lysholm score (p < 0.01) (Table 4).
The results of the current study demonstrated that hydroxyapatite-containing bioabsorbable screws significantly reduce the extent of tibial tunnel widening and foreign body reactions and increase screw resorption compared to pure PLLA screws.
Since hydroxyapatite particles have a structure similar to that of bone minerals, they have been assumed to be conducive to osteogenesis. Increased osteogenesis is advantageous since it decreases micromotion between the graft and a screw during rehabilitation, enhances osteogenesis around the screw, and conserves bone stock for reoperation.11) In animal experiments using rats, HA-added screws showed statistically significantly enhanced osteogenesis than pure PLLA screws and significantly lower inflammation reaction rates in histological examination.22) Tamai et al.23) reported that HA has a reinforcing effect on the mechanical properties of the matrix due to its high modulus of elasticity and compressive strength. It has also been suggested that bioabsorbable screws with added calcium phosphate are more effective in terms of postoperative stability, osteogenesis, and biocompatibility.
Moisala et al.18) demonstrated that compared to metal screws, bioabsorbable screws made of PLLA without calcium phosphate components resulted in a significantly high level of anteroposterior expansion of the tibial tunnel on MRI and knee laxity. This is because even though the two screws had biomechanically similar traits, bioabsorbable screws contributed more to tunnel widening since their components, such as PLLA, were absorbed and reacted differently from those of metal screws. Lind et al.20) reported that compared to metal screws, HA-added bioabsorbable screws showed significantly less tibial tunnel widening on X-rays although no differences were observed in clinical results; however, they stated that the results were obtained 1 year after operation, limiting the validity of their findings. Robinson et al.14) reported that computed tomography (CT) scans showed the HA-added bioabsorbable screws resulted in less tunnel widening and 50% less cortication around screws than pure PLLA screws. However, these studies had common limitations: the small comparison group and the lack of clinical evaluation. Results of the current study were congruent with previous studies: MRI at minimum 2 years after surgery showed HA-added PLLA screws resulted in less tibial tunnel widening than pure PLLA screws. Although clinical outcomes at minimum 2 years after the surgery showed no significant differences between the 2 groups, large tunnel widening in the area close to the joint line showed a correlation with joint instability. Moisala et al.18) showed that the anteroposterior diameter of the tibial tunnel on MRI was correlated with the knee laxity testing. We assumed that the most important factor in graft fixation is the aperture of tunnel, which has more influence on the laxity of the graft than the midsection, even though there was no statistically significant correlation established between the extent of tunnel widening and the clinical results.24) In addition, since large tunnel widening can cause significant problems during revision surgery, we should not overlook its importance. Previous studies revealed that tibial tunnel widening was frequently maximal in the mid-zone of the tibial tunnel and occurred in the plane of movement of the knee joint.2526) On the other hand, Frosch et al.16) reported 85.2% of enlargement of the proximal third of the tibial tunnel although the mean value of the whole tibial tunnel was decreased on MRI at 12 postoperative months. They postulated that despite bone ingrowth, tunnel widening was not avoided in the aperture area, even though the screw was placed close to the joint line. In our study, the extent of tunnel enlargement was the most in the aperture area similar as in the study of Frosch et al.16) Weber et al.15) also revealed that CSA at the aperture and midsection of the tibial tunnel generally increased to the 24th postoperative week, with progressive tunnel narrowing thereafter. They suggested that tunnel expansion at time points greater than 6 months may result in poor graft/bone healing, which may lead to increased instability over time. The etiology remains uncertain, but it might be multifactorial related to both biological and mechanical factors.
Many studies reported that bone tunnel widening did not directly affect graft laxity or reconstruction failure.1527) Theoretically, however, a decrease in the space between the graft and bone facilitates graft incorporation and allows better knee joint stability, so further clinical research is required.28) We postulated that an amorphous loose connective tissue, which was enveloped by the graft/bone interface, could provide either a temporary or permanent anchorage; however, such change was more hampered in the pure PLLA group due to more foreign body reactions.
Unlike β-TCP, HA is a natural mineral material that shows affinity to bone and contains high biocompatibility, since it is similar to mineral component which consists of teeth and bones of mammals.23)
Limitations of this study were as follows: first, this study was retrospective, thus there may have been bias in group selection. In addition, the 2 different tibial fixations were not performed in same period. Second, bone replacement scale could not be precisely examined because CT scans were not used in evaluating the extent of tunnel widening. However, MRI can provide sufficient information on the status of bioabsorbable screws and bone tunnel16) and is superior to CT in evaluating the graft and foreign body reactions. Also we did not want to impose additional cost and cause radiation exposure to the patients. Third, we did not evaluate the femoral tunnel because there were no different variables related to the femoral tunnel between 2 groups. Finally, the minimum 2-year follow-up was relatively short to conclude on the extent of tunnel widening and clinical results. Further follow-up studies and research on the results of treatment are required.
The significance of this study is that, the resorption rate of bioabsorbable screws, the extent of tunnel widening on MRI, and clinical functions were evaluated in 172 patients with a minimum 2-year follow-up after ACL reconstruction performed at the same institution.
In conclusions, the HA added PLLA screws would be more advantageous for tibial graft fixation by reducing tibial tunnel widening, improving osteointegration, and reducing foreign body reactions than pure PLLA screws. Even though there were no notable clinical differences between the pure PLLA group and the PLLA-HA group, tibial tunnel widening in the proximal area showed a tendency to increase knee laxity measured using the KT-2000 arthrometer.
References
1. Vaishya R, Agarwal AK, Ingole S, Vijay V. Current trends in anterior cruciate ligament reconstruction: a review. Cureus. 2015; 7(11):e378. PMID: 26697280.

2. Bedi A, Maak T, Musahl V, et al. Effect of tibial tunnel position on stability of the knee after anterior cruciate ligament reconstruction: is the tibial tunnel position most important? Am J Sports Med. 2011; 39(2):366–373. PMID: 21173195.
3. Van der Bracht H, Verhelst L, Stuyts B, Page B, Bellemans J, Verdonk P. Anatomic single-bundle ACL surgery: consequences of tibial tunnel diameter and drill-guide angle on tibial footprint coverage. Knee Surg Sports Traumatol Arthrosc. 2014; 22(5):1030–1039. PMID: 23370987.

4. Bedi A, Musahl V, Steuber V, et al. Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy. 2011; 27(3):380–390. PMID: 21035990.

5. Coats AC, Johnson DL. Two-stage revision anterior cruciate ligament reconstruction: indications, review, and technique demonstration. Orthopedics. 2012; 35(11):958–960. PMID: 23127442.

6. Athanasiou KA, Agrawal CM, Barber FA, Burkhart SS. Orthopaedic applications for PLA-PGA biodegradable polymers. Arthroscopy. 1998; 14(7):726–737. PMID: 9788368.

7. Macarini L, Murrone M, Marini S, Mocci A, Ettorre GC. MRI in ACL reconstructive surgery with PDLLA bioabsorbable interference screws: evaluation of degradation and osteointegration processes of bioabsorbable screws. Radiol Med. 2004; 107(1-2):47–57. PMID: 15031696.
8. Warden WH, Chooljian D, Jackson DW. Ten-year magnetic resonance imaging follow-up of bioabsorbable poly-L-lactic acid interference screws after anterior cruciate ligament reconstruction. Arthroscopy. 2008; 24(3):370.e1–370.e3. PMID: 18308192.

9. Johnston M, Morse A, Arrington J, Pliner M, Gasser S. Resorption and remodeling of hydroxyapatite-poly-L-lactic acid composite anterior cruciate ligament interference screws. Arthroscopy. 2011; 27(12):1671–1678. PMID: 21978431.

10. Barber FA, Dockery WD. Long-term absorption of betatricalcium phosphate poly-L-lactic acid interference screws. Arthroscopy. 2008; 24(4):441–447. PMID: 18375277.
11. Macarini L, Milillo P, Mocci A, Vinci R, Ettorre GC. Poly-L-lactic acid–hydroxyapatite (PLLA-HA) bioabsorbable interference screws for tibial graft fixation in anterior cruciate ligament (ACL) reconstruction surgery: MR evaluation of osteointegration and degradation features. Radiol Med. 2008; 113(8):1185–1197. PMID: 18956150.
12. Lee SR, Jang HW, Lee DW, Nam SW, Ha JK, Kim JG. Evaluation of femoral tunnel positioning using 3-dimensional computed tomography and radiographs after single bundle anterior cruciate ligament reconstruction with modified transtibial technique. Clin Orthop Surg. 2013; 5(3):188–194. PMID: 24009904.

13. Fules PJ, Madhav RT, Goddard RK, Newman-Sanders A, Mowbray MA. Evaluation of tibial bone tunnel enlargement using MRI scan cross-sectional area measurement after autologous hamstring tendon ACL replacement. Knee. 2003; 10(1):87–91. PMID: 12649033.

14. Robinson J, Huber C, Jaraj P, Colombet P, Allard M, Meyer P. Reduced bone tunnel enlargement post hamstring ACL reconstruction with poly-L-lactic acid/hydroxyapatite bioabsorbable screws. Knee. 2006; 13(2):127–131. PMID: 16352431.

15. Weber AE, Delos D, Oltean HN, et al. Tibial and femoral tunnel changes after ACL reconstruction: a prospective 2-year longitudinal MRI study. Am J Sports Med. 2015; 43(5):1147–1156. PMID: 25681503.
16. Frosch KH, Sawallich T, Schutze G, et al. Magnetic resonance imaging analysis of the bioabsorbable Milagro interference screw for graft fixation in anterior cruciate ligament reconstruction. Strategies Trauma Limb Reconstr. 2009; 4(2):73–79. PMID: 19697105.

17. Lajtai G, Noszian I, Humer K, Unger F, Aitzetmuller G, Orthner E. Serial magnetic resonance imaging evaluation of operative site after fixation of patellar tendon graft with bioabsorbable interference screws in anterior cruciate ligament reconstruction. Arthroscopy. 1999; 15(7):709–718. PMID: 10524818.

18. Moisala AS, Jarvela T, Paakkala A, Paakkala T, Kannus P, Jarvinen M. Comparison of the bioabsorbable and metal screw fixation after ACL reconstruction with a hamstring autograft in MRI and clinical outcome: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2008; 16(12):1080–1086. PMID: 18762911.

19. Singhal MC, Holzhauer M, Powell D, Johnson DL. MRI evaluation of the tibial tunnel/screw/tendon interface after ACL reconstruction using a bioabsorbable interference screw. Orthopedics. 2008; 31(6):575–579. PMID: 18661880.

20. Lind M, Feller J, Webster KE. Tibial bone tunnel widening is reduced by polylactate/hydroxyapatite interference screws compared to metal screws after ACL reconstruction with hamstring grafts. Knee. 2009; 16(6):447–451. PMID: 19423351.

21. Cox CL, Spindler KP, Leonard JP, Morris BJ, Dunn WR, Reinke EK. Do newer-generation bioabsorbable screws become incorporated into bone at two years after ACL reconstruction with patellar tendon graft?: a cohort study. J Bone Joint Surg Am. 2014; 96(3):244–250. PMID: 24500587.
22. Hunt JA, Callaghan JT. Polymer-hydroxyapatite composite versus polymer interference screws in anterior cruciate ligament reconstruction in a large animal model. Knee Surg Sports Traumatol Arthrosc. 2008; 16(7):655–660. PMID: 18418577.

23. Tamai N, Myoui A, Tomita T, et al. Novel hydroxyapatite ceramics with an interconnective porous structure exhibit superior osteoconduction in vivo. J Biomed Mater Res. 2002; 59(1):110–117. PMID: 11745543.
24. Rodeo SA, Kawamura S, Kim HJ, Dynybil C, Ying L. Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft-tunnel motion? Am J Sports Med. 2006; 34(11):1790–1800. PMID: 16861579.
25. Clatworthy MG, Annear P, Bulow JU, Bartlett RJ. Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc. 1999; 7(3):138–145. PMID: 10401649.

26. Hoher J, Moller HD, Fu FH. Bone tunnel enlargement after anterior cruciate ligament reconstruction: fact or fiction? Knee Surg Sports Traumatol Arthrosc. 1998; 6(4):231–240. PMID: 9826805.
27. Emond CE, Woelber EB, Kurd SK, Ciccotti MG, Cohen SB. A comparison of the results of anterior cruciate ligament reconstruction using bioabsorbable versus metal interference screws: a meta-analysis. J Bone Joint Surg Am. 2011; 93(6):572–580. PMID: 21411708.
28. Weiler A, Peine R, Pashmineh-Azar A, Abel C, Sudkamp NP, Hoffmann RF. Tendon healing in a bone tunnel: Part I: biomechanical results after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy. 2002; 18(2):113–123. PMID: 11830804.
Fig. 1
Flowchart of inclusion and exclusion of participants. PLLA: poly-L-lactic acid, HA: hydroxyapatite, MRI: magnetic resonance imaging.
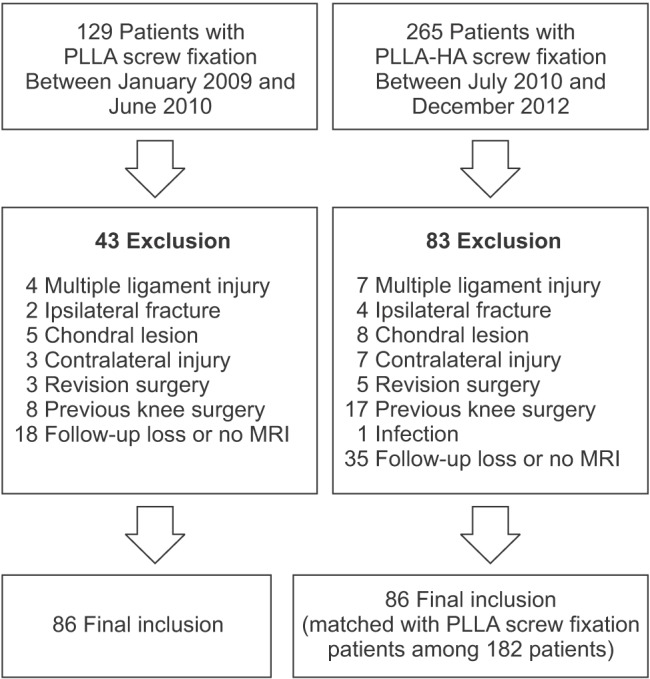
Fig. 2
Tibial bone tunnel maximum cross-sectional area was measured automatically by picture archiving and communication system (Maroview ver. 5.4; MAROTECH Inc.).
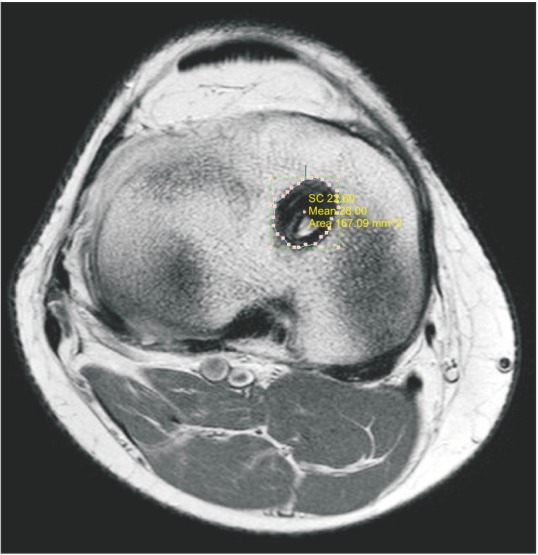
Fig. 3
The signal quality of the bone tunnel-screw-graft system was evaluated to estimate the degree of osteointegration of the screw (arrow) on the coronal view of T2-weighted magnetic resonance imaging and classified as good (A), partial (B), some (C), and little (D).
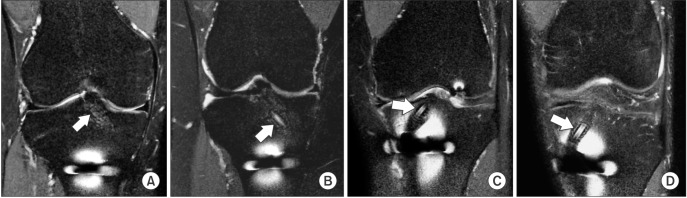
Fig. 4
Foreign body reactions (arrow) were classified as no reaction (A), edema (B), or cyst formation (C) on the coronal view of T2-weighted magnetic resonance imaging.
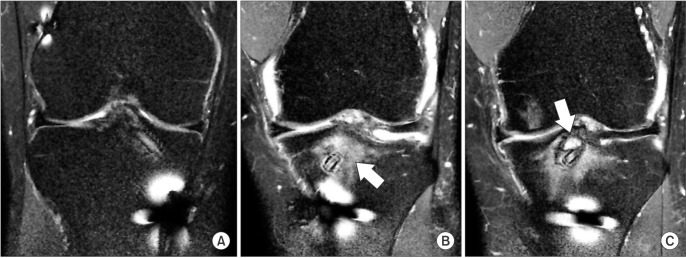
Fig. 5
Coronal (A) and sagittal (B) views of magnetic resonance imaging after anterior cruciate ligament reconstruction using the poly-L-lactic acid screw showed significant widening in the proximal area of the tibial tunnel (arrow).
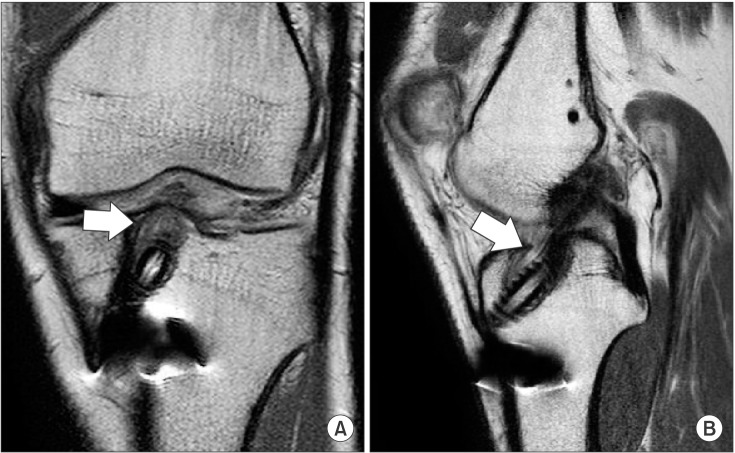
Table 1
Preoperative Patient Characteristics
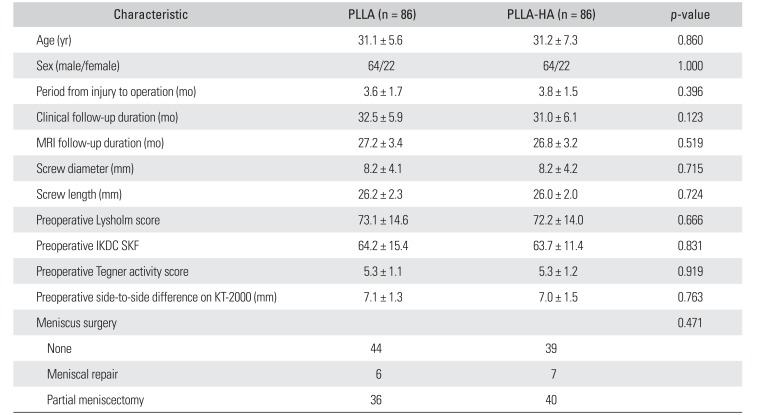
Table 2
Comparison of Postoperative Clinical Outcomes and MRI Results




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download