Abstract
There are few reports on the surgical treatment of secondary malignancy arising from an osteochondroma on the lateral side of the proximal tibia. From March 2008 to December 2011, 3 patients were treated for a secondary chondrosarcoma from an osteochondroma of the proximal tibia involving the fibula. The operative procedure can be summed up as follows: (1) resection of the tumor including the fibula; (2) preservation of the peroneal nerve and the fibular head; and (3) arthrodesis of the proximal tibiofibular joint. Serial radiological studies showed successful fusion in the proximal tibiofibular joint in all patients. The Musculoskeletal Tumor Society functional scores were excellent in all 3 patients. No patients showed instability of the ipsilateral knee joint in any direction. All 3 patients could return to sports activities. Until the last follow-up, there was no evidence of disease recurrence. We suggest that the operative procedure described in this article would provide satisfactory oncological and functional outcomes.
Osteochondromas are the most common benign tumors of the bones, representing 35% of benign bone tumors and occurring in 3% of the general population.123) Patients usually present with an osteochondroma during the second and third decades of life. Although osteochondromas can occur in any bone, they are found most commonly around the knee and the shoulder. Patients undergo surgical treatment due to growth disturbance, nerve compression, joint motion limitation, pain, tendon irritation, overlying bursitis or malignant transformation. Osteochondromas in the proximal tibia are frequently symptomatic because of abundant tendinous structures and lack of the soft tissue. Surgical resection of an osteochondroma of the medial condyle of the proximal tibia is relatively easy. However, for the lateral side, the peroneal nerve and the fibula make it difficult to extirpate the lesion.
Malignant transformation is the most serious complication of an osteochondroma. Less than 1% of osteochondromas undergo malignant transformation into secondary chondrosarcoma.456) Even though surgical resection is the mainstay of therapy, few reports dealt with surgical treatment of secondary malignancy of osteochondromas arising from the lateral side of the proximal tibia. In this report, we introduce a surgical procedure and outcomes for secondary chondrosarcoma from an osteochondroma of the proximal tibia involving the fibula.
From March 2008 to December 2011, three patients with a mean age of 27.7 years (range, 22 to 38 years) were treated for secondary chondrosarcoma from an osteochondroma of the proximal tibia involving the fibula at Seoul National University Bundang Hospital. All 3 cases were solitary lesions. Two of them experienced pain and swelling on the lateral side of the knee. One patient presented with a 6-month growing mass with a positive Tinel's sign over the fibular neck. All patients had been informed of the existence of an osteochondroma at another clinic before the index visit. Radiologic studies showed definite changes in shape and size of the lesion compared with previous examination. No patient complained of limited range of motion of the knee joint.
A presumptive diagnosis was made based on the radiologic studies. Our radiological criteria for malignant transformation of an osteochondroma were as follows: (1) a growing lesion on serial radiographs taken after skeletal maturity; (2) a lesion with cartilage cap thickness greater than 1–3 cm on magnetic resonance imaging (MRI) scans; and (3) a lesion with scattered punctuated calcification. No patient underwent biopsy before the definitive surgery.
In all 3 cases, surgery was performed in three major steps: (1) isolation of the peroneal nerve; (2) en bloc resection of the lesion including the fibula and lateral cortex of the proximal tibia preserving the fibula head; and (3) arthrodesis of the proximal tibiofibular joint (Fig. 1).
A skin incision was made along the peroneal nerve beginning posteriorly just proximal to the fibular head and terminating 2–3 cm distal to the tumor. After identification of the common peroneal nerve under the peroneus longus, the tunnel of peroneus longus and extensor digitorum longus was unroofed. The tibialis anterior was detached from Gerdy's tubercle and the proximal tibia. After isolation of the deep peroneal nerve and the anterior tibial artery, the articular branch of the deep peroneal nerve and the recurrent tibial artery were ligated. Posteriorly, the peroneal origin of the soleus and the tibialis posterior was detached.
Under fluoroscopic guidance, the proximal and distal osteotomies preserving the fibular head were performed. The lateral cortex of the proximal tibia from which the tumor originated was resected en bloc. The proximal tibiofibular arthrodesis was carried out by fixation with a cannulated screw after removal of articular cartilage. Pathology of the resected specimen confirmed a grade 1 secondary chondrosarcoma in all patients.
In the immediate postoperative period, active range-of-motion exercise was begun after subsiding of operative pain and full weighted-bearing in a knee brace was allowed to prevent a varus injury. Patients were observed in the clinic every 3 months for 2 years, every 6 months for the next 2 years, and annually thereafter. MRI of the primary tumor site was performed every 6 months for 2 years, and annually thereafter. At each clinic visit, a history was taken and a chest imaging was performed. At postoperative 1 year, the cannulated screw for arthrodesis of the proximal tibiofibular joint was removed after radiological confirmation of fusion. No patient received adjuvant radiotherapy or chemotherapy.
Functional evaluation was performed with the use of the functional classification system of the Musculoskeletal Tumor Society (MSTS), which includes 6 parameters, such as pain, function, emotional acceptance, use of walking supports, walking ability, and gait. Each was scored from 0 to 5, with a maximum score of 30.7) At each visit, physical examination of knee joint stability and functional evaluation of the peroneal nerve were performed. This study was performed under the approval of Seoul National University Bundang Hospital Institutional Review Board (No. B-1503/292-109).
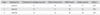
Brief characteristics and postoperative results of 3 cases are listed in Table 1. Pathologic findings were consistent with grade-1 chondrosarcoma with cartilage caps thicker than 1 cm in all 3 patients. The cartilage component had smaller cells that lack matrix formation with increased cellularity and invaded the bone component.
There was no immediate postoperative complication including wound infection, nerve palsy, and vascular compromise. There was no evidence of disease recurrence on the regional and chest images until the last follow-up. Serial radiological studies showed successful fusion in the proximal tibiofibular joint in all patients at a mean of 9.3 months after surgery (range, 8 to 10 months) (Fig. 2). The Musculoskeletal Tumor Society functional scores were excellent in all 3 patients. No patients showed instability of the ipsilateral knee joint in any direction. There were no neurological deficits of the peroneal nerve until the last follow-up. All 3 patients could return to sports activities.
In this report, we described our surgical procedure and its outcomes for secondary chondrosarcoma arising from an osteochondroma of the lateral side of the proximal tibia involving the proximal fibula. The procedure can be summed up as resection of the tumor including the fibula, preservation of the peroneal nerve and the fibular head, and arthrodesis of the proximal tibiofibular joint. Considering that malignant transformation of osteochondroma reveals a low-grade chondrosarcoma in most patients, we believe there is sufficient justification for preservation of the functional structures in the procedure.
The exact incidence of malignant transformation in osteochondroma is not known. Authors have reported that the incidence is 0.4%–2% in patients with solitary osteochondroma and 5%–25% in patients with hereditary multiple exostoses.689) Fortunately, most chondrosarcomas arising in an osteochondroma have proved to be low-grade. In a study by Ahmed et al,10) among 107 secondary chondrosarcomas arising in osteochondrosarcoma, 97 tumors were grade 1, and 10 tumors were grade 2. In addition, no tumor was grade 3. With respect to location, secondary chondrosarcoma tends to occur most commonly in the pelvis, trunk, and the proximal femur.91011) Affection of the proximal tibia and its outcomes has been rarely reported, although some large series study included a few cases.12) Surgical resection of a malignant bone lesion of the medial condyle of the proximal tibia is considered as relatively easy. However, a wide resection in the lateral side of the proximal tibia may cause permanent functional impairment, which is associated with sacrifice of the peroneal nerve and the proximal fibula.
With respect to the fibular resection, Malawer13) described two detailed resection types in 1984. Type I or marginal resection requires excision of the proximal fibula with 2–3 cm of the diaphysis and muscle cuff in all directions with preservation of the common peroneal nerve. Type II or wide extra-compartmental resection involves resection of 6 cm of normal diaphysis, the anterior and lateral muscle compartments, the peroneal nerve, the anterior tibial artery and the tibiofibular joint extra-articularly. Marginal or intralesional margin resection in malignant bone tumor usually results in poor oncological outcomes. However, some authors advocated intentional marginal resection around structures that are important for limb function. Kanazawa et al.14) reported the outcomes of intentional marginal excision of osteosarcoma of the proximal fibular to preserve limb function. When a good response to preoperative chemotherapy was expected based on radiologic studies, they preserved the peroneal nerve and the anterior tibial vessels in 3 patients with osteosarcoma in the proximal fibula. With a minimum 5-year follow-up, all 3 patients had normal ankle and knee functions without evidence of local recurrence. Considering that the majority of secondary chondrosarcomas from osteochondromas turn out low-grade neoplasms, preservation of functional structures can be regarded as a reasonable approach.
Many authors have attempted modifications of the original classification proposed by Malawer. Erler et al.15) added two more resection types (type III and IV), both of which were based on Malawer's type I resection: type III resection involves the sacrifice of the deep peroneal nerve and type IV resection preserves the proximal tibiofibular joint. Any systematic study has not evaluated the role of arthrodesis of the proximal tibiofibular joint in knee stability and functional outcomes after resection of the proximal fibula. Most studies, in which type IV resection was included, reported that the arthrodesis of the proximal tibiofibular joint is not essential.16) Einoder and Choong17) also noted that wide resection of the fibular head for a tumor might not require reconstruction, unlike treatment of traumatic disruption of the lateral ligamentous structures of the knee. They reported that function was satisfactory in 6 consecutive cases where resection of the fibular head was done without ligamentous reconstruction after 14 years of follow-up. However, 3 of 6 patients in their series showed 1+ or 2+ lateral instability on physical examination. Meanwhile, there are some reports suggesting the necessity of arthrodesis. Youdas et al.18) in their study on donor site morbidity after vascularized fibula transfer, suggested that inadequate fixation of the proximal segment would cause superior migration of the fibula and excessive coronal plane motion on the donor site compared with the normal control. Krieg et al.19) reported a case with osteochondroma of the fibula for which they performed a marginal resection by reflecting the fibular head proximally and an arthrodesis of the proximal tibiofibular joint. In the current study, all 3 patients returned to sports activities. Moreover, one of them (patient no. 2) is a member of an amateur football team. In our opinion, the advantage of arthrodesis of the proximal tibiofibular joint after type IV fibular resection is that it provides lateral stability of the knee joint. In the normal knee, varus stress is restrained by the lateral ligament complex, and it is transferred to the fibular bony structure. Without an arthrodesis of the proximal tibiofibular joint, varus stress after type IV resection is transferred to the tibia via the tibiofibular joint. In this situation, the varus stress is restrained by the joint capsule of the joint rather than the lateral ligament complex. Arthrodesis of the proximal tibiofibular joint could return the role of varus restraint to the lateral ligament complex (Fig. 3).
We believe that the arthrodesis of the proximal tibiofibular joint after type IV fibular resection is worthy enough to compensate for the additional effort of arthrodesis and removal of the screw. We think that our reconstruction method could be one of options for reconstruction after resection of the lateral part of the knee according to patients' age and their demands.
In conclusion, for the secondary chondrosarcomas arising from an osteochondroma in the lateral side of the proximal tibia involving the fibula, we performed removal of the tumor including the proximal fibula while preserving the fibular head and the common peroneal nerve, followed by arthrodesis of the proximal tibiofibular joint. All of the three patients had no evidence of disease and showed excellent functional outcomes until the last follow-up. In spite of the limitation of the small number of patients and lack of a comparison group, we suggest that our procedure introduced in this article could provide satisfactory oncological and functional outcomes.
Figures and Tables
Fig. 1
Schematic drawings of the operative procedure. (A) Isolation of the peroneal nerve. (B) Arthrodesis of the proximal tibiofibular joint using a cannulated screw after en bloc resection of the tumor including segmental resection of the fibula.
Fig. 2
23-year-old man was diagnosed with secondary chondrosarcoma in the proximal tibia. (A) Plain radiographs taken 3 years before the surgery showing a benign osteochondroma in the proximal tibia. (B) Plain radiographs showing destruction of the fibula. (C) T2-weighted axial magnetic resonance imaging showing a thick cartilage cap with high signal intensity and bone scan showing increased uptake. (D) Plain radiographs taken in the immediate postoperative period and after removal of the cannulated screw. Yellow arrow: cartilage cap.
Fig. 3
Schematic drawings showing varus stress transfer in the normal knee (A), after resection of the proximal fibula (B), and after arthrodesis of the proximal tibiofibular joint (C). Red arrow: strain, green arrow: varus stress.
ACKNOWLEDGEMENTS
This study was supported by a grant from the Seoul National University Bundang Hospital Research Fund, Seongnam, Korea (No. 02-2013-113).
References
1. Kitsoulis P, Galani V, Stefanaki K, et al. Osteochondromas: review of the clinical, radiological and pathological features. In Vivo. 2008; 22(5):633–646.
2. Morton KS. On the question of recurrence of osteochondroma. J Bone Joint Surg Br. 1964; 46(4):723–725.

3. Saglik Y, Altay M, Unal VS, Basarir K, Yildiz Y. Manifestations and management of osteochondromas: a retrospective analysis of 382 patients. Acta Orthop Belg. 2006; 72(6):748–755.
4. Altay M, Bayrakci K, Yildiz Y, Erekul S, Saglik Y. Secondary chondrosarcoma in cartilage bone tumors: report of 32 patients. J Orthop Sci. 2007; 12(5):415–423.

5. Florez B, Monckeberg J, Castillo G, Beguiristain J. Solitary osteochondroma long-term follow-up. J Pediatr Orthop B. 2008; 17(2):91–94.

6. Garrison RC, Unni KK, McLeod RA, Pritchard DJ, Dahlin DC. Chondrosarcoma arising in osteochondroma. Cancer. 1982; 49(9):1890–1897.

7. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993; (286):241–246.

8. Norman A, Sissons HA. Radiographic hallmarks of peripheral chondrosarcoma. Radiology. 1984; 151(3):589–596.

9. Solomon L. Chondrosarcoma in hereditary multiple exostosis. S Afr Med J. 1974; 48(16):671–676.
10. Ahmed AR, Tan TS, Unni KK, Collins MS, Wenger DE, Sim FH. Secondary chondrosarcoma in osteochondroma: report of 107 patients. Clin Orthop Relat Res. 2003; (411):193–206.

11. Brien EW, Mirra JM, Luck JV Jr. Benign and malignant cartilage tumors of bone and joint: their anatomic and theoretical basis with an emphasis on radiology, pathology and clinical biology: II. juxtacortical cartilage tumors. Skeletal Radiol. 1999; 28(1):1–20.

12. Gitelis S, Bertoni F, Picci P, Campanacci M. Chondrosarcoma of bone: the experience at the Istituto Ortopedico Rizzoli. J Bone Joint Surg Am. 1981; 63(8):1248–1257.

13. Malawer MM. Surgical management of aggressive and malignant tumors of the proximal fibula. Clin Orthop Relat Res. 1984; (186):172–181.
14. Kanazawa Y, Tsuchiya H, Nonomura A, Takazawa K, Yamamoto N, Tomita K. Intentional marginal excision of osteosarcoma of the proximal fibula to preserve limb function. J Orthop Sci. 2003; 8(6):757–761.

15. Erler K, Demiralp B, Ozdemir MT, Basbozkurt M. Treatment of proximal fibular tumors with en bloc resection. Knee. 2004; 11(6):489–496.

16. Mootha AK, Saini R, Dhillon M, Bali K, Dhatt SS, Kumar V. Modified resection technique for proximal fibular osteochondromas. Orthop Traumatol Surg Res. 2011; 97(5):569–573.

17. Einoder PA, Choong PF. Tumors of the head of the fibula: good function after resection without ligament reconstruction in 6 patients. Acta Orthop Scand. 2002; 73(6):663–666.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download