Abstract
Background
The results of operative treatments for symptomatic accessory navicular are debatable. In some cases, recurrent pain may develop after the Kidner procedure. The purpose of this study is to review the reasons for recurrent pain after the Kidner procedure and to suggest possible options for revision surgery.
Methods
We reviewed the clinical and radiological outcomes in 9 patients who underwent revision surgery for recurrent pain after the Kidner procedure. During the revision surgery, the tibialis posterior tendon was reattached to the navicular either by advancing the tendon in 4 patients or by lengthening the tendon in another 4 patients. In the other 1 patient, the flexor digitorum longus tendon was transferred. Surgeries for the accompanying deformities were performed simultaneously in all patients. The results were evaluated using the American Orthopaedic Foot and Ankle Society ankle-hindfoot score and a visual analog scale. The mean follow-up was 2.3 years (range, 1 to 5 years).
Results
The mean American Orthopedic Foot and Ankle Society ankle-hindfoot score improved from 71.25 to 81.50 in the advancement group, and 71.75 to 90.00 in the lengthening group. The mean visual analog scale improved from 7.75 to 4.25 in the advancement group and from 7.50 to 1.75 in the lengthening group.
The navicular bone is a common location for an accessory bone. The developmental anomaly of accessory navicular syndrome is found in approximately 10%–21% of normal feet.12) The accessory navicular is classified into three types: type I is completely separated from the navicular tuberosity, type II is separated from the mother bone by a synchondrosis, and type III is united by a bony bridge to the navicular tuberosity.34) Among the different types of accessory navicular, type II is the most symptomatic.
When conservative treatments for painful accessory navicular, such as shoe modification, inserts, and life style modification, fail to provide adequate pain relief, surgical treatment is recommended. The current literature supports several surgical treatment options for symptomatic accessory navicular:34567891011) simple excision; excision and relocation of the tibialis posterior (TP) tendon (the Kidner procedure); percutaneous drilling; and fusion of the accessory navicular to the body of the navicular. The results of these surgical treatments are debatable. In some cases, the Kidner procedure may hinder proper healing and cause degeneration of the relocated TP tendon. Furthermore, if there is discontinuity at the TP tendon insertion sites, failure of the reattachment may cause severe functional deficits, including possible proximal migration of the TP tendon.1) However, no clinical case of proximal migration of the TP tendon has been reported after surgery for symptomatic accessory navicular.
We believe that the increased tension at the reattachment site is one of the reasons for recurrent pain after the Kidner procedure. Thus, we hypothesized that planovalgus or hindfoot valgus deformities are related to recurrent pain after the Kidner procedure.
The purpose of this study is to review the reasons for recurrent pain after surgery for symptomatic accessory navicular and to suggest possible options for surgical revision.
This is a retrospective case series. The inclusion criteria were patients who underwent revision surgery for recurrent pain after the Kidner procedure and completed at least 12-months of follow-up after the revision surgery. The exclusion criteria were patients with recurrent pain from nonunion after fusion of an accessory navicular, a history of a local steroid injection, local infection, or underlying diseases such as uncontrolled diabetic mellitus, rheumatoid arthritis, or seronegative spondyloarthropathy. Surgical treatments were performed on 10 patients from August 2004 to March 2010. Nine patients (9 feet) were included in this study because 1 patient was lost to follow-up (Table 1). Six patients underwent their initial surgery at another hospital, and the remaining 3 patients had their initial surgery performed by the author (WCL) at the study institution. The mean duration between the initial surgery and the revision surgery was 2.6 years (range, 0.5 to 5 years). The mean follow-up period was 2.3 years (range, 1 to 5 years). This study was approved by the Institutional Review Board (No. IIT-2012-268) and informed consent was obtained from all patients.
In 1 patient, the TP tendon could not be reattached to the navicular due to retraction of the distal stump proximal to the tip of the medial malleolus, and so a transfer of the flexor digitorum longus (FDL) was performed instead. In 4 patients, the distal stump of the TP tendon was attached with forceful advancement alone (the advancement group). The remaining 4 patients underwent TP tendon lengthening above the ankle joint by Z-plasty, and then the distal stump was attached to the navicular with minimal force (the lengthening group). The average length of advancement or lengthening of the tendon was approximately 2 cm.
Prior to the revision surgery, all patients had difficulty performing a single limb heel rise on physical examination and had hindfoot valgus deformities on radiographic evaluation. Planovalgus deformities were noted in 7 feet; the first talometatarsal angle angulated plantarward by greater than 10° as noted on a weight-bearing foot lateral radiograph. Two patients had a hindfoot valgus deformity with normal longitudinal arches. Surgeries for the planovalgus or hindfoot valgus deformity were performed simultaneously in all patients with medial displacement calcaneal osteotomy (MDCO), lateral column lengthening (LCL), or both, to relieve the tension at the reattachment site of the TP tendon (Table 1). MDCO was performed in 6 feet, including 2 feet with hindfoot valgus with normal longitudinal arches, and LCL was performed in 5 feet. Two patients underwent both MDCO and LCL.
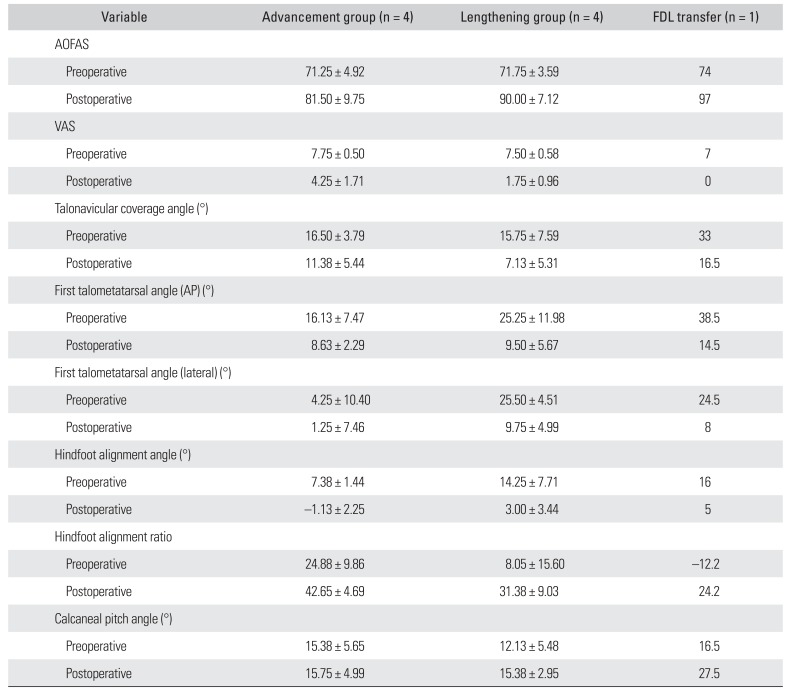
Preoperative and postoperative clinical evaluations were performed using the American Orthopedic Foot and Ankle Society (AOFAS) ankle-hindfoot score1213) and a 10-point visual analog scale (VAS) for pain. Radiographic and clinical results were separately tabulated for each group (Table 2). However, the statistical power was too low to compare the groups. Therefore, only the preoperative and postoperative results of the patients were compared.
The radiographic assessments were made with weight-bearing dorsoplantar (anteroposterior [AP]) and lateral radiographs of the foot and hindfoot alignment radiographs. All radiographs were digitally obtained through the Picture Archiving Communication System (Marosis Enterprise PACS, Marosis Enterprise PACS; Infinitt, Seoul, Korea). On the weight-bearing foot AP radiographs, the talonavicular coverage angle, and the first talometatarsal angle were measured. On the weight-bearing foot lateral radiographs, the first talometatarsal angle and the calcaneal pitch angle were measured. On the hindfoot alignment view, the hindfoot alignment angle and the hindfoot alignment ratio were obtained.14) The hindfoot alignment angle, which is the angle between the tibial axis and the calcaneal axis, was measured and expressed as a positive number when it was in the valgus position. The hindfoot alignment ratio was obtained by dividing the width from the calcaneus medial to the tibial axis by the calcaneal width at its widest portion on the alignment view. If the tibial axis line passed through more medial side compared to the medial calcaneal cortex, the measurements were expressed as negative values.
Statistical analysis was not performed owing to the insufficient sample size; in order to achieve sufficient power for statistical analysis (β ≤ 0.20, power ≥ 0.80), each group needed 15 patients.
The MDCO and LCL procedures were performed before the soft tissue reconstruction. LCL was performed by fusing the calcaneocuboid joint in 2 feet, and by osteotomy at the anterior calcaneus in 3 feet by using the Evans procedure.
For the TP tendon advancement, the degenerative segment of the TP tendon was excised and the distal end of the tendon was advanced to the navicular, with the foot positioned in approximately 20° of plantarflexion and inversion. The tendon was securely fixed with one or two 2.7-mm suture anchors (Arthrex, Naples, FL, USA). Additional sutures were applied between the tendon and the adjacent soft tissues.
To lengthen the TP tendon, a 6-cm longitudinal incision was made on the posterior aspect of the medial border of the tibia, after excision of the degenerative segment of the TP tendon. After exposure of the tendon, Z-plasty lengthening was performed via a 5-cm longitudinal incision in the middle of the tendon (Fig. 1). The TP tendon was lengthened by 2 cm and repaired with interrupted 3-0 nylon sutures. The distal end of the TP tendon was securely fixed using one or two 2.7-mm suture anchors.
For the FDL transfer, the master knot of Henry was dissected and the FDL tendon was transected distal to that point. Using 2-0 Ethibond polyester suture (Ethicon, New Brunswick, NJ, USA), a single strand was placed into the distal end of the FDL tendon. The FDL tendon was then rerouted from the plantar to the dorsal direction of the navicular through a 5-mm bone tunnel. The FDL was then sutured back onto itself with two simple interrupted 2-0 Ethibond polyester sutures.
Postoperatively, all patients were immobilized in a short leg non-weight-bearing cast for 6 weeks. For the first 3 weeks, the ankle was placed in 10° of plantarflexion and inversion, and this was followed by 3 weeks of casting in a neutral position. Weight-bearing as tolerated was permitted once the ankle was cast in the neutral position. After 6 weeks of postoperative care, the cast was removed and a stirrup brace was applied and maintained for another 6 weeks.
The intraoperative findings of all the patients revealed different degrees of degeneration of the TP tendon. After the revision surgery, all the patients had normal muscle strength when examined by manual resistance of the TP and all the patients were able to perform a single heel rise.
In all the patients, the AOFAS score, VAS, and radiographic parameters improved after surgery (Table 2). The mean AOFAS score improved from 71.50 (range, 67 to 76) to 85.75 (range, 67 to 100) in all patients: from 71.25 (range, 67 to 76) to 81.50 (range, 67 to 88) in the advancement group, and from 71.75 (range, 67 to 75) to 90.00 (range, 84 to 100) in the lengthening group. The mean VAS improved from 7.62 (range, 7 to 8) to 3.00 (range, 1 to 6) in all patients: from 7.75 (range, 7 to 8) to 4.25 (range, 2 to 6) in the advancement group, and from 7.50 (range, 7 to 8) to 1.75 (range, 1 to 3) in the lengthening group. Two of the 4 patients in the advancement group reported a pain VAS ≥ 4 in contrast to none in the lengthening group. The 1 patient with FDL transfer reported satisfactory results. One patient in the advancement group complained of unsatisfactory results including pain and difficulty with rehabilitation after undergoing reattachment in the extreme inversion position. This patient underwent an additional surgery (TP tendon lengthening and FDL transfer) 4 years after the revision surgery.
This study was conducted to investigate the characteristics of the feet and the outcomes of surgical treatment for recurrent pain after the Kidner procedure. In the total 9 patients available for this study, reattachment of the TP tendon with lengthening (the lengthening group) showed better clinical results than the forceful reattachment of the TP tendon (the advancement group).
In this series, all patients were reoperated on because of severe pain at the attachment site of the TP tendon; they could not perform a single heel rise on the affected foot at the time of the revision. The decision about which procedure to perform was not made on clear-cut criteria, and the characteristics and severity of the patients' symptoms varied. However, the authors noted that all the feet had pes planovalgus or hindfoot valgus deformity, and all patients showed degenerative changes of the TP tendon at its reattachment site. Although several articles have reported on patients with persistent symptoms after the Kidner procedure, no current literature reviews the possible treatment options and outcomes in these patients.3111516) The authors believe that this is the first review of revision surgery for persistent pain after the Kidner procedure.
The relationship between painful accessory navicular and flatfoot is controversial, and it is not clear whether flatfoot is the cause of painful accessory navicular or vice versa.381617) Vaughan and Singh18) reported that pes planus may contribute to ongoing pain after excision of the accessory navicular. Seven of the 9 patients in the present study had planovalgus deformity; however, 2 patients had normal longitudinal arches with only hindfoot valgus deformity. We believe that both planovalgus and hindfoot valgus deformities can be associated with recurrent pain after the Kidner procedure, because both flatfoot and hindfoot valgus can increase the tension on the TP tendon and result in degeneration of the tendon, thereby causing recurrent pain.
In the study patients, the TP tendon already has been advanced during the initial surgery to close the gap after excision of the accessory navicular. During revision surgery, an additional gap was created after debridement of the degenerated segment of TP tendon discovered in all the cases of this series, and additional advancement of the TP tendon was required. In this series, the mean length of advancement or lengthening of the tendon was 2 cm, after the degenerated portion was debrided. Because the excursion of the TP tendon was only 2 cm, excessive tension was inevitable at the TP tendon reattachment site after advancing the TP tendon.19) Although patients in the advancement group showed improvements after the revision surgery, they complained of pain after prolonged standing or walking. In contrast, all the patients in the lengthening group showed good results. After experiencing poor results from advancement of the TP tendon during the initial treatment, the tendon was lengthened to reduce the tension at the reattachment site.
Corrective surgery to reduce strain on the TP tendon should be determined according to the deformity in each individual case. In the presence of hindfoot valgus deformity without forefoot abduction or low longitudinal arch, MDCO was sufficient to reduce the tension. In the cases involving planovalgus deformity, the authors independently decided to use either the MDCO or LCL method of correction, or combination of both procedures.
To avoid problems associated with the Kidner procedure, the accessory navicular should be soundly fused to the mother bone.411) However, secure fixation of such a small bone is difficult, and assessment of the progression of the fusion is challenging owing to the small opposing surfaces between the accessory bone and the body of the navicular.
Another option for closing the gap of the TP tendon is a FDL transfer.20) In cases with stage 2 adult acquired flatfoot, an intercalary defect is created, centered at approximately 3–5 cm proximal to the insertion after debridement of the degenerated TP tendon; an FDL transfer is a common method to reconstruct the invertor function.
The TP tendon has multiple insertions besides the primary insertion at the navicular; therefore, it cannot be proximally retracted even though the TP tendon is detached from its insertion after surgery for painful accessory navicular. One patient in the present study showed proximal migration and needed FDL transfer. We believe that the major portion of the TP tendon was inserted only to the accessory navicular in this case. Kiter et al.1) have reported that disruption at the reattachment site may cause proximal migration of the tendon when the TP tendon mainly inserts at the accessory navicular. Although the clinical result of the patient treated with FDL transfer was satisfactory, other cases were not treated with an FDL transfer for the reconstruction of the gap at the insertion of the TP tendon. We believe that reattachment of the TP tendon would be better in the long-term, rather than sacrificing the FDL. However, FDL transfer is as an alternative method of treatment when reattachment of the TP tendon is not feasible.
There are several limitations in this study. The first limitation is the small number of cases, which means that statistically significant results could not be obtained. In order to achieve sufficient statistical power (β ≤ 0.20, power ≥ 0.80), 15 cases would have been needed in each group. As the symptoms of most patients are typically improved after excision of the accessory navicular, revision surgery is not common. However, we think this report on a small number of patients is meaningful because severe disability may be caused by persistent pain after the Kidner procedure. The second limitation is that the degree of associated preoperative and postoperative deformity was not significantly different between the groups. Interestingly, better clinical results were obtained in the lengthening group, which had a smaller talonavicular coverage angle, lower arch, and greater hindfoot valgus on the postoperative radiographs. These findings suggest that the lower degree of postoperative pain in the lengthening group cannot be explained by better correction of the flatfoot deformity. The third limitation is that the size of the accessory navicular was not assessed at the time of the initial surgery. As the TP tendon should be advanced a farther distance when a larger accessory navicular is excised, assessment of the size is an important factor. In this current study, 6 of the 9 patients had their initial surgery at another hospital and the size of the accessory navicular could not be determined. Therefore, we cannot assess whether a larger defect at the primary surgery was a contributing factor to the recurrent pain. The fourth limitation is that the TP tendon force was not measured with an objective method. Although all revision procedures and examinations were performed by the authors, the power of the TP tendon on manual examination, the single limb heel rise postoperatively, and subtle weakness after lengthening may not have been noticed by manual examination. In addition, further follow-up is needed to determine whether there are any long-term problems with the strength of the TP tendon.
In this study, recurrent pain after the Kidner procedure was associated with pes planovalgus or hindfoot valgus deformity. Reattachment of the TP tendon after lengthening demonstrated better outcome compared to advancement of the tendon. Additional procedures to correct the planovalgus or hindfoot valgus deformity should be considered to treat recurrent pain after surgery for symptomatic accessory navicular.
References
1. Kiter E, Gunal I, Karatosun V, Korman E. The relationship between the tibialis posterior tendon and the accessory navicular. Ann Anat. 2000; 182(1):65–68. PMID: 10668560.

2. Grogan DP, Gasser SI, Ogden JA. The painful accessory navicular: a clinical and histopathological study. Foot Ankle. 1989; 10(3):164–169. PMID: 2613130.

3. Bennett GL, Weiner DS, Leighley B. Surgical treatment of symptomatic accessory tarsal navicular. J Pediatr Orthop. 1990; 10(4):445–449. PMID: 2358479.

4. Chung JW, Chu IT. Outcome of fusion of a painful accessory navicular to the primary navicular. Foot Ankle Int. 2009; 30(2):106–109. PMID: 19254502.

5. Kiter E, Gunal I, Turgut A, Kose N. Evaluation of simple excision in the treatment of symptomatic accessory navicular associated with flat feet. J Orthop Sci. 2000; 5(4):333–335. PMID: 10982680.

6. Kopp FJ, Marcus RE. Clinical outcome of surgical treatment of the symptomatic accessory navicular. Foot Ankle Int. 2004; 25(1):27–30. PMID: 14768961.

7. Macnicol MF, Voutsinas S. Surgical treatment of the symptomatic accessory navicular. J Bone Joint Surg Br. 1984; 66(2):218–226. PMID: 6707058.

8. Sullivan JA, Miller WA. The relationship of the accessory navicular to the development of the flat foot. Clin Orthop Relat Res. 1979; (144):233–237. PMID: 535230.

9. Nakayama S, Sugimoto K, Takakura Y, Tanaka Y, Kasanami R. Percutaneous drilling of symptomatic accessory navicular in young athletes. Am J Sports Med. 2005; 33(4):531–535. PMID: 15722276.

10. Malicky ES, Levine DS, Sangeorzan BJ. Modification of the Kidner procedure with fusion of the primary and accessory navicular bones. Foot Ankle Int. 1999; 20(1):53–54. PMID: 9921775.

11. Scott AT, Sabesan VJ, Saluta JR, Wilson MA, Easley ME. Fusion versus excision of the symptomatic Type II accessory navicular: a prospective study. Foot Ankle Int. 2009; 30(1):10–15. PMID: 19176179.

12. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the anklehindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994; 15(7):349–353. PMID: 7951968.

13. Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg. 2007; 46(2):65–74. PMID: 17331864.

14. Lee WC, Moon JS, Lee HS, Lee K. Alignment of ankle and hindfoot in early stage ankle osteoarthritis. Foot Ankle Int. 2011; 32(7):693–699. PMID: 21972764.

15. Ray S, Goldberg VM. Surgical treatment of the accessory navicular. Clin Orthop Relat Res. 1983; (177):61–66. PMID: 6861408.

16. Veitch JM. Evaluation of the Kidner procedure in treatment of symptomatic accessory tarsal scaphoid. Clin Orthop Relat Res. 1978; (131):210–213.

17. Sella EJ, Lawson JP, Ogden JA. The accessory navicular synchondrosis. Clin Orthop Relat Res. 1986; (209):280–285. PMID: 3731610.

18. Vaughan P, Singh D. Ongoing pain and deformity after an excision of the accessory navicular. Foot Ankle Clin. 2014; 19(3):541–553. PMID: 25129360.

19. Flemister AS, Neville CG, Houck J. The relationship between ankle, hindfoot, and forefoot position and posterior tibial muscle excursion. Foot Ankle Int. 2007; 28(4):448–455. PMID: 17475139.

20. Myerson MS, Corrigan J. Treatment of posterior tibial tendon dysfunction with flexor digitorum longus tendon transfer and calcaneal osteotomy. Orthopedics. 1996; 19(5):383–388. PMID: 8727331.

Fig. 1
(A) The intraoperative finding revealed degeneration of the tibialis posterior tendon. (B) To lengthen the tibialis posterior tendon, a 6-cm longitudinal incision was made on the posterior aspect of the medial border of the tibia. (C) The tibialis posterior tendon was lengthened by 2 cm and repaired with interrupted 3-0 nylon sutures and the distal end of the tibialis posterior tendon was securely fixed using 2.7-mm suture anchors.
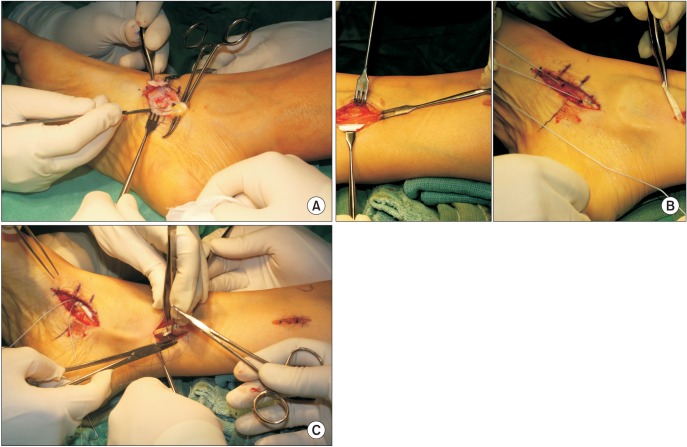
Table 1
Characteristics of the Patients
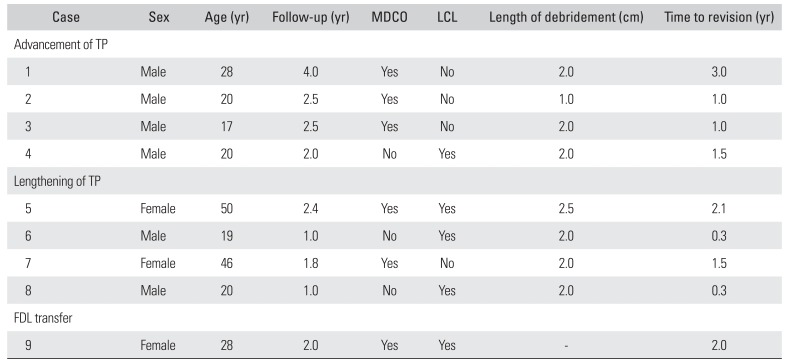
Table 2
Changes in Clinical and Radiographic Parameters According to the Treatment




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download