Abstract
Background
Reverse total shoulder arthroplasty has become a widely accepted surgical procedure in Japan since the time when the implants were approved for use in 2014. There is a doubt, however, as to whether the implants designed for Western people are suitable for Japanese people, particularly for females of relatively small stature. The purpose of this study was to investigate the glenoid dimension, with special focus on the length after glenoid reaming, in Japanese rotator cuff tear patients.
Methods
Fifty-six shoulders of 55 patients (35 males and 20 females; mean age, 63.8 years) were studied. Using the three-dimensional computed tomography images of the entire scapula before shoulder surgery, we measured the glenoid height and width, and calculated the correlation between these measurements and the patient's height. Further, we measured the anteroposterior length of the scapular neck at the subchondral bone and the length at 15 mm medial to the subchondral bone, to simulate both the glenoid width after reaming (width of the ‘virtual reamed surface’) and the space available for the end of the center post of a standard glenoid baseplate.
Results
The average glenoid height and width were 35.8 mm and 28.1 mm in males and 30.8 mm and 23.4 mm in females, respectively. There was a significant correlation between patient height and glenoid size (glenoid height, r = 0.69; width, r = 0.75; p < 0.01). The mean value of the width of the virtual reamed surface was 27.0 mm in males and 22.5 mm in females. The mean anteroposterior length at 15 mm medial to the subchondral bone was 12.4 mm in males and 9.5 mm in females; the length was shorter than 8 mm in 6 female shoulders.
Conclusions
There was a significant correlation between patient height and glenoid size. Considering that the common diameter of the commercially available baseplates and their center posts is greater than 25 mm and 8 mm, respectively, these prosthetic parts would be too large, especially for the Japanese female glenoid. Given that the current results of Japanese shoulder dimensions are similar to those of Asian people, ‘Asian size implants’ should be developed.
Reverse total shoulder arthroplasty (RSA), which was developed by Grammont et al.1) in France, is the inverted version of the constrained designs that were introduced in the 1970s for the treatment of painful arthritis in the rotator cuff deficient shoulder. Its unique design of a lower and more medial center of rotation of the shoulder can increase the moment arm of the deltoid muscle.23) The success of the prosthesis has led to expansion of the indications from cuff tear arthropathy with pseudoparalysis to other disorders which are deficient in cuff function.4) Following the excellent results achieved in many countries, RSA was also granted approval to be performed in Japan in 2014, and since then it has been rapidly applied. As of September 2016, a total of 5 series of commercial implants have become available for RSA in Japan.
Regarding these prostheses, it is important to note that according to previous studies, Japanese shoulders are generally smaller than those of the Western population. Matsumura et al.5) used computed tomography (CT) to analyze the dimension of the glenoid fossa and reported that the mean glenoid height and width were 31.5 mm and 23.1 mm, respectively, in the Japanese healthy population, which were smaller than those in the Western population.67) Moreover, as baseplates are generally fixed after reaming in practical surgeries, the reamed glenoids of Japanese patients would show an even shorter width than the results of Matsumura et al.5) Ji et al.8) also demonstrated that the size of the female glenoid was sometimes smaller than the baseplate in a Korean population, and claimed that manufacture of a new prosthesis size suitable for Koreans should be undertaken.
The RSA implants currently available in Japan were all developed in Western countries and are designed to fit European and American people. Thus, there is a concern that the implants might not be suitable for smaller Japanese patients. In fact, the width of baseplates currently available in Japan ranges from 22 to 29 mm, and most of the baseplates are larger than 25 mm. This discrepancy in width between Japanese glenoids and commercial baseplates may be one of the structural reasons for inadequate fixation of the baseplates.
In this study, we investigated the glenoid dimensions with a particular focus on the length after glenoid reaming, in Japanese rotator cuff tear patients for the purpose of (1) evaluating the dimensions of the glenoid and scapular neck in Japanese rotator cuff tear patients (RSA is mainly indicated in such patients and the population background, such as age, should be matched through the selection) and (2) clarifying the prevalence and extent of the size mismatch between the postreamed glenoid of Japanese patients and the baseplates which are currently (September 2016) available in Japan.
This study was approved by the Ethical Committee of Kyoto University School of Medicine (No. E2228).
Fifty-six shoulders of 55 rotator cuff tear patients (35 males and 20 females; mean age, 63.8 ± 9.6 years [range, 39 to 83 years]; median age, 66.0 years; 36 right shoulders and 20 left shoulders) were included in this imaging study. All of the patients were Japanese who had undergone surgical treatment (arthroscopic rotator cuff repair, arthroscopic superior capsular reconstruction,9) and RSA) for their shoulder from January 2012 to February 2015 in Kyoto University Hospital. No patient had previous shoulder surgery. The preoperative three-dimensional (3D) CT images of the affected shoulders were retrospectively examined.
The electronic images of the patients were transmitted through the picture archiving and communication system and observed via viewer software (Centricity Enterprise Web ver. 3.0; GE Healthcare Japan, Tokyo, Japan). The 3D surfaces were reconstructed using a commercially available software (Aquarius NET 4.4.4.23; TeraRecon, San Mateo, CA, USA). We examined the following two points. The superoinferior length (height) and anteroposterior length (width) of the glenoid surface were measured using the 3D-reconstructed images (Fig. 1). The correlation between glenoid size (height and width) and patient's height was calculated. To simulate the approximate glenoid surface which would remain after reaming for baseplate setting, first we defined the scapular plane which included the most distal point of the inferior scapular angle, the center of the glenoid surface, and the medial pole of the scapula.10) Second, the axial plane was created, which was vertical to the scapular plane including the glenoid center and the medial pole of the scapula (Fig. 2). The glenoid width after reaming (i.e., the width of the ‘virtual reamed surface’) was measured using this axial plane. The dashed yellow line just below the subchondral bone was considered to indicate the glenoid surface after reaming, accordingly its length was recorded as the width of the virtual reamed surface (Fig. 3).
As of September 2016, the following 5 types of implants were available in Japan: Aequalis Reverse II shoulder (Wright Medical, Memphis, TN, USA), Trabecular Metal Reverse Shoulder System (Zimmer Biomet, Warsaw, IN, USA), Comprehensive Reverse Shoulder System (Zimmer Biomet), SMR Modular Shoulder Replacement (Lima Co., Udine, Italy), and Delta Xtend Reverse Shoulder System (DePuy Synthes, Warsaw, IN, USA). In consideration of the standard baseplate of small size, the baseplates with the shortest width are SMR (22 mm) and Aequalis (25 mm). The former has a markedly large center post diameter, and it is a unique implant, not a standard type implant. Therefore, we simulated the Aequalis baseplate as a small standard baseplate with a center post of 15 mm in length and 8 mm in diameter. In order to fix this baseplate adequately, the scapular neck anteroposterior length should be greater than 8 mm, even at the site 15 mm medial to the virtual reamed surface; we also recorded the anteroposterior length of this portion (Fig. 4).
The correlation between the glenoid size and patient height was quantified using Spearman correlation. Sex differences in patient height, glenoid size, width of the virtual reamed surface, and anteroposterior length at 15 mm medial to the virtual reamed surface were compared using two-tailed Student t-tests. A p-value of less than 0.05 was considered significant. Statistical analyses were performed using JMP Pro ver.11.0.0 (SAS Institute Inc., Cary, NC, USA).
In order to determine the intra/interobserver reliability, 2 observers, an orthopedic clinical fellow and a shoulder specialist, examined the same 20 glenoid bones that were randomly selected using Research Randomizer (www.randomizer.org). The former observer took measurements on 2 separate occasions with at least an 1-week interval to check the intraobserver reliability. The latter observer also performed the measurements independently to examine the interobserver reliability. The intra/interobserver reliability was evaluated through calculation of the intraclass correlation coefficients.11)
In the 56 shoulders, there was no severely deformed glenoid, such as the Walch B2 or C pattern.12) The evaluation of our intraobserver and interobserver reliability showed good agreement. The former was calculated as the intraclass correlation coefficients for the 2 measurements of one observer and the values were 0.974 for glenoid width and 0.952 for the width at 15 mm medial to the virtual reamed surface. The latter was calculated as the intraclass correlation coefficients for the 2 observers and the values were 0.962 for glenoid width and 0.934 for the width at 15 mm medial to the virtual reamed surface.
At the glenoid surface, the mean height and width were 35.8 ± 2.2 mm (range, 31.8 to 39.7 mm) and 28.1 ± 1.6 mm (range, 25.1 to 32.1 mm), respectively, in males, and 30.8 ± 1.8 mm (range, 27.9 to 34.6 mm) and 23.4 ± 1.7 mm (range, 20.2 to 26.0 mm), respectively, in females (Table 1). There was a significant correlation between patient height and glenoid size (glenoid height, r = 0.69; width, r = 0.75; p < 0.01).
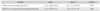
The mean width of the virtual reamed surface was 27.0 ± 1.6 mm (range, 23.2 to 30.0 mm) in males and 22.5 ± 1.5 mm (range, 19.8 to 25.2 mm) in females. The mean anteroposterior length at 15 mm medial to the virtual reamed surface was 12.4 ± 1.4 mm (range, 9.7 to 15.7 mm) in males and 9.5 ± 1.3 mm (range, 7.4 to 11.6 mm) in females (Table 2). In 6 shoulders of 20 female patients, the anteroposterior length at 15 mm medially was less than 8 mm, which is the same as the diameter of the center post of the small standard baseplate.
Several studies have evaluated glenoid morphology using CT scans in Asian populations. Matsumura et al.5) analyzed 160 healthy Japanese shoulders using CT scans and reported an average glenoid height of 31.5 mm and glenoid width of 23.1 mm. Phonphok and Kulkamthorn13) in a study of Thai people reported a mean glenoid height and width of 32.3 mm and 24.4 mm, respectively. In contrast, in a study of mostly Caucasians, Iannotti et al.7) measured the glenohumeral joints of cadavers and living patients using a caliper or magnetic resonance imaging and found a mean glenoid height of 39 mm and width of 29 mm. In comparison with Europeans or Americans, the glenoid size of Asians is generally smaller according to these studies. In the present study, the respective mean glenoid height and width were 33.3 mm and 25.9 mm in total, 35.8 mm and 28.1 mm in males, and 30.8 mm and 23.4 mm in females. Overall, our results were closer to the previous Asian data than those of Caucasians.5713) In addition, he glenoid width is particularly small in Asian females. Accordingly, there is a concern that the commonly used RSA implants that were designed and developed in Western countries may not be of appropriate fit for Asian shoulders.
We defined the virtual reamed surface as the plane after the RSA reaming procedure and measured the width of it. This width was intended to indicate the exact width of the glenoid at the time of baseplate implantation, which should be slightly shorter than prereamed glenoids. Although to date there has been no study simulating the glenoid after reaming, the value of the virtual reamed surface should be beneficial for shoulder surgeons who routinely perform RSAs. In this study, the female subjects had a mean virtual reamed surface width of 22.5 ± 1.5 mm (range, 19.8 to 25.2 mm). Our female glenoid width was very close to the previously reported Asian female results (current study, 23.4 ± 1.7 mm; another study including healthy Japanese women, 21.3 ± 1.4 mm; and Thai population study, 22.0 ± 1.7 mm).513) Thus, it can be inferred that many Asian females have a much smaller glenoid than the currently commercially available baseplates.
When a large baseplate is positioned on a small glenoid, the risk of baseplate instability is likely to increase. In a biomechanical study using Korean female cadavers of short stature (< 160 cm), Chae et al.14) observed that subjects with a 29-mm baseplate showed more micromotions than those with 25 mm baseplates. They suggested that their specimens did not have sufficient glenoid bone stock to securely fix a 29-mm baseplate and that this inappropriate size match would likely result in early glenoid loosening.14)
In this study, we also highlighted the diameter of the scapular neck that should completely contain the center post of the baseplate. We presented an example of a standard small baseplate and the tail of its center post that reached the site 15 mm medial to the virtual reamed surface, and we examined the anteroposterior length of the scapular neck. On average, the 20 female patients in our study had a width of only 9.5 mm at 15 mm medial to the virtual reamed surface. In the 6 extremely small patients, the diameter was less than 8 mm, which was the same as the diameter of the center post of the standard example. This result strongly suggests that there is an undeniable risk whereby even the center post of the small standard baseplate can fracture or rupture the scapular neck. Indeed we can shift the center of the baseplate slightly anteriorward so as not to break the posterior wall of the scapular neck.15) However, the shift effect would be limiting according to our results. Therefore, the need for smaller implants suitable for Asian females is an urgent issue.
There are several limitations of this study. First, the sample size is small. This is because we selected only consecutive rotator cuff tear patients in order to match the population background with those for whom RSA is mainly indicated. Further studies with a larger sample size are expected. Second, CT scans that we used for glenoid size measurement can be a possible limitation as the thickness of the articular cartilage is neglected. We, however, fix the baseplates after removing the glenoid cartilage, and the size of the glenoid bone is crucial. Moreover, all measurements showed good to excellent intraobserver and interobserver reliabilities, and CT scans as a study tool are fully credible. Third, the Lima and Depuy Synthes baseplates have a curved back and the morphology of the virtual reamed surface would differ from the other commercial implants and our example. The width, however, of the virtual reamed surface was measured as a line length at the baseplate center, and a difference in baseplate morphology would have little effect on the interpretation of the result. Fourth, for some baseplates, the recommendation is to fix in a lower position, not at the center of the glenoid. However, the center post, which breaks a scapular neck at the center level, cannot be contained within any lower scapular neck, either. Our results should be considered as basic data for any implants.
In conclusion, our CT study of rotator cuff tear patients demonstrated that there is a significant correlation between patient height and glenoid size. The commercially available baseplates and their center posts can be too large, especially for the Japanese female glenoid. Considering the similarity of the Japanese shoulder dimensions to those of Asian people, ‘Asian size implants’ which are currently unavailable should be developed.
Figures and Tables
Fig. 1
Measurement of the size of the glenoid surface. The superoinferior length (height) and anteroposterior length (width) were measured on three-dimensional images.

Fig. 2
Method of the measurement of the glenoid width. (A) The measurement was performed on the reconstructed axial slice. (B) The optimal slice was created from the whole three-dimensional data. (C) The axial slice was created vertical to the scapula plane. (D) The axial slice included the glenoid center and the medial pole of the scapula.

Fig. 3
Axial view perpendicular to the scapular plane. The dashed yellow line drawn just beneath the subchondral bone indicates the level of the virtual reamed surface of the glenoid neck. The length of the dashed yellow line just below the subchondral bone was measured as the width of the virtual reamed surface.
Fig. 4
Measurement of the anteroposterior length of the scapular neck at 15 mm medial to the virtual reamed surface. The length of the orange line was measured.
Table 1
Glenoid Size
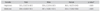
Table 2
The Width of the Scapular Neck at the Subchondral Bone (Virtual Reamed Surface) and at 15 mm Medial to the Virtual Reamed Surface
References
1. Grammont P, Trouilloud P, Laffay JP, Deries X. Concept study and realization of a new total shoulder prosthesis. Rhumatologie. 1987; 39(10):407–418.
2. Boileau P, Walch G. The three-dimensional geometry of the proximal humerus: implications for surgical technique and prosthetic design. J Bone Joint Surg Br. 1997; 79(5):857–865.
3. Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff: results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004; 86(3):388–395.
4. Smith CD, Guyver P, Bunker TD. Indications for reverse shoulder replacement: a systematic review. J Bone Joint Surg Br. 2012; 94(5):577–583.
5. Matsumura N, Oki S, Ogawa K, et al. Three-dimensional anthropometric analysis of the glenohumeral joint in a normal Japanese population. J Shoulder Elbow Surg. 2016; 25(3):493–501.

6. Churchill RS, Brems JJ, Kotschi H. Glenoid size, inclination, and version: an anatomic study. J Shoulder Elbow Surg. 2001; 10(4):327–332.

7. Iannotti JP, Gabriel JP, Schneck SL, Evans BG, Misra S. The normal glenohumeral relationships: an anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am. 1992; 74(4):491–500.

8. Ji JH, Jeong JY, Song HS, et al. Early clinical results of reverse total shoulder arthroplasty in the Korean population. J Shoulder Elbow Surg. 2013; 22(8):1102–1107.

9. Mihata T, Lee TQ, Watanabe C, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013; 29(3):459–470.

10. Kwon YW, Powell KA, Yum JK, Brems JJ, Iannotti JP. Use of three-dimensional computed tomography for the analysis of the glenoid anatomy. J Shoulder Elbow Surg. 2005; 14(1):85–90.

11. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979; 86(2):420–428.

12. Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999; 14(6):756–760.

13. Phonphok P, Kulkamthorn N. Assessment of approximate glenoid size in Thai people. J Med Assoc Thai. 2014; 97:Suppl 2. S14–S18.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download