Abstract
Background
To evaluate the clinical outcome of revision of primary shoulder replacement by using reverse total shoulder arthroplasty (RTSA).
Methods
Seven patients underwent revision RTSA with a mean follow-up of 22.1 months (range, 12 to 54 months). Their mean age at the time of operation was 75.5 years (range, 70 to 80 years). Assessments were performed on the preoperative and postoperative visual analogue scale (VAS) score, muscle strength, range of motion, University of California at Los Angeles (UCLA) score, Constant score, subjective satisfaction and the anteroposterior and axillary views of the glenohumeral joint. The primary operation was hemiarthroplasty in 5 patients, total shoulder replacement in 1 patient, and reverse shoulder arthroplasty in 1 patient. The cause of revision surgery was infection in 2 patients, humeral stem loosening in 2 patients, glenoid arthropathy in 2 patients, and glenoid loosening in 1 patient. The mean duration from primary operation to revision surgery was 52 months (range, 27 to 120 months).
Results
The VAS score for pain during motion was improved from 7.3 preoperatively to 2.1 postoperatively (p = 0.03). There were increases in the mean active forward flexion (from 62.1° to 92.8°), abduction (from 70° to 87.1°), external rotation (from 44.2° to 47.4°), and internal rotation (from L5 to L4; p > 0.05) postoperatively. Performance in activities of daily living improved (p > 0.05), except for lifting 10 lb above the shoulder (from 1.2 to 1.1; p = 0.434). Overall, 5 of 7 patients were satisfied with the results of revision surgery. The mean Constant score improved from 44.8 preoperatively to 57.1 postoperatively (p = 0.018). The mean UCLA score improved from 12.8 preoperatively to 22.8 postoperatively (p = 0.027). In the postoperative radiological evaluation, no radiolucency was observed around the base plate or humeral stem.
Conclusions
Pain could be reduced after revision RTSA, but improvements in range of motion and function were difficult to achieve. We think that the patients' satisfaction was relatively high despite the low function score due to the preoperative severe pain and marked limitation of range of motion.
The incidence of shoulder arthroplasty has shown a gradual increase for the past 10 years and is still increasing. With advancement in surgical techniques and prosthetic designs, the lifespan of implants has been improving and the indications of shoulder arthroplasty have expanded to include younger populations. Consequently, the number of revision surgeries has also been increasing due to early and late complications after shoulder arthroplasty. Total shoulder arthroplasty (TSA) has been frequently used as a revision surgery, but relatively unsatisfactory outcomes have been reported in many studies,123) especially due to soft tissue dysfunction or glenoid loosening, instability, or infection.45) Meanwhile, the prevalence of reverse TSA (RTSA) as a salvage procedure for failed primary anatomical prosthesis or reverse prosthesis has also been increasing.6) Although RTSA can be a good treatment option after failed arthroplasty, concerns emerged over the fact that outcomes of revision RTSA are less favorable than those of primary RTSA and that its complication rates are high.7) Austin et al.8) reported on a comparison between 28 cases of primary RTSA and 28 cases of revision RTSA, in which clinical outcomes and range of motion (ROM) were poorer in revision RTSA than in primary RTSA, with a complication rate of 36%. However, several recent studies have reported satisfactory outcomes of revision RTSA as a salvage procedure. Flury et al.9) performed revision RTSA on 21 cases of rotator cuff dysfunction that occurred after TSA and reported improved postoperative ROM and pain with a high satisfaction rate of 84% for 46 months of follow-up. Patel et al.10) performed revision RTSA on 31 cases of failed shoulder arthroplasty and reported improvement in all postoperative outcomes, with a high satisfaction rate of 82.2% for 40.7 months of follow-up. The objective of the present study was to report the initial clinical outcomes in patients who received revision RTSA as a salvage procedure for failed prior arthroplasty. We believed that postoperative pain relief and functional improvement could be achieved.
Final approval of exemption from review by the Kyung Hee University Hospital Institutional Review Board was obtained because this study was retrospective in nature (No. 1605-12).
We retrospectively reviewed 7 patients who underwent RTSA for revision surgery among 142 patients who were treated with reverse shoulder arthroplasty (RSA) between April 2008 and June 2014. The mean age of the patients at the time of operation was 75.5 years (range, 70 to 80 years), and the mean follow-up period was 22.1 months (range, 12 to 54 months). Five of the included patients were female. Four patients had the revision surgery on the right shoulder, and 3 had it on the left shoulder. The cause for undergoing primary arthroplasty was proximal humerus fracture in 3 patients, cuff tear arthropathy in 2 patients, humeral head avascular necrosis in 1 patient, and rheumatoid arthritis in 1 patient (Table 1). The mean interval between the initial and revision operations was 52 months (range, 27 to 120 months).
All patients underwent preoperative physical examinations, and postoperative clinical evaluations were performed regularly at 3 months, 6 months, and 12 months after surgery and annually thereafter in the outpatient clinic. Last follow-up values were compared with preoperative values. Subjective pain level was assessed by using the visual analogue scale (VAS) for pain, and rotator cuff muscle strength was measured by using a portable, handheld Nottingham Mecmesin myometer (Mecmesin Ltd., Nottingham, UK). Muscle strength during forward flexion was measured in 90° forward flexion on the scapular plane while sitting in a chair, and muscle strength during external and internal rotations was measured with the shoulders in neutral position and the elbows flexed at 90°. Shoulder joint ROM was evaluated based on the preoperative and postoperative forward flexion, external rotation, internal rotation, and external abduction data. Assessment of clinical functions was conducted by using the Constant score11) and the shoulder rating scale of the University of California at Los Angeles (UCLA).12) Subjective satisfaction was assessed at the final follow-up, and the levels of satisfaction were divided into very satisfied, satisfied, not better and not worse, and worse. In all patients, the anteroposterior view of the glenohumeral joint and the axillary view were obtained preoperatively and postoperatively, as well as at each follow-up visit. In the preoperative radiological examination, loosening of the humeral and glenoid components and glenohumeral instability were identified. Humeral component loosening, glenoid base plate loosening, scapular notching, and hardware failure were identified in the most recent follow-up. The degree of lateralization of the humeral component was determined by measuring the preoperative and postoperative transverse distance between the greater tuberosity and the center of rotation. In addition, the degree of distalization of the humeral component was determined by measuring the preoperative and postoperative vertical distance between the greater tuberosity and the acromion. Humeral component loosening was assessed according to the criteria presented by Sperling et al.,13) while glenoid loosening was determined according to the criteria presented by Lazarus et al.14)
The senior author (YGR) performed all the operations under general anesthesia in a beach chair tilted by 60°. For prosthesis, the Aequalis system (Tornier, Montbonnot Saint Martin, France) was used in 3 of 7 patients, the Biomet system (Biomet, Warsaw, IN, USA) was used in 3 patients, and Biomet and Aequalis systems were used for the glenoid and humeral components, respectively, in 1 patient. The skin incision made in the previous surgery was used, and the operation was performed via the deltopectoral approach in all patients. The humeral stem was removed in 6 of 7 patients, of whom 2 required anterior corticotomy and vertical humeral osteotomy. In the patients who underwent vertical humeral osteotomy, after removal of the previous humeral stem, a Tornier humeral long stem was inserted, and wiring was added (Fig. 1). In one patient who did not undergo humeral stem removal, revision surgery was performed after an adapter was inserted, as there was no humeral stem loosening (Fig. 2). In 4 patients who showed a glenoid cavitary defect on preoperative three-dimensional computed tomography (3DCT), a Biomet screw-type baseplate was inserted, with 1 patient additionally receiving a simultaneous iliac bone graft. In the other 3 patients, an Aequalis peg-type baseplate was inserted. In all patients, tension in the deltoid and conjoined tendons was checked as well as tension during humeral longitudinal traction and dislocation during external rotation with a trial cup. The subscapularis was already lost in 6 of the 7 patients, and subscapularis repair was possible in only 1 patient. After standard wound closure, the arm was placed in a “hand shake” orthosis.
Postoperatively, patients were immobilized in a “hand shake” orthosis for 6 weeks. On the day after the operation, passive pendulum exercise and exercises for the elbow, wrist, and hand were performed. After 6 weeks, active forward flexion was allowed after removal of the orthosis. Resistance exercise was recommended from 12 weeks after the operation.
The cause of revision surgery was infection in 2 patients, humeral stem loosening in 2 patients, glenoid arthropathy in 2 patients, and glenoid loosening in 1 patient. RTSA was performed as a one-stage revision surgery in 5 patients and second-stage revision surgery in 2 patients with infection.
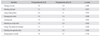
The mean VAS score during motion decreased from 7.3 preoperatively to 2.1 at the last follow-up (p = 0.03). Forward flexion improved from 62.1° preoperatively to 92.8° postoperatively (p = 0.091), abduction from 70° to 87.1° (p = 0.248) and external rotation from 44.2° to 47.4° (p = 0.345). Internal rotation improved from a spine level of L5 to L4 (p = 0.595). Although the differences were not statistically significant, postoperative ROM showed an increase from the preoperative ROM. On the assessment of muscle strength, the preoperative and postoperative mean values were respectively 2.5 kg and 6.5 kg for forward flexion, 4 kg and 6 kg for external rotation, and 2.8 kg and 7.4 kg for internal rotation, showing improvements (Table 2). On the activities of daily living, the preoperative and postoperative values were respectively 1.8 and 2.0 for putting on a coat (p = 0.463), 1.4 and 1.6 for washing the back (p = 0.631), 2.0 and 2.1 for using a back pocket (p = 0.797), 1.9 and 2.0 for managing the toilet (p = 0.638), 1.9 and 2.3 for combing hair (p = 0.352), 1.4 and 2.0 for reaching to a high shelf (p = 0.453), 1.2 and 1.1 for lifting 10 lb above the shoulder (p = 0.434), 1.9 and 2.0 for washing the opposite axilla (p = 0.356), and 1.8 and 2.2 for bringing the hand to the mouth (p = 0.154). The results showed overall improvement with the exception of lifting 10 lb above the shoulder. However, the levels of improvement were small and statistically insignificant (Table 3).
The UCLA score was 12.8 preoperatively and 22.8 postoperatively (p = 0.027). The Constant score increased from 44.8 to 57.1 (p = 0.018), showing statistically significant difference. The subjective ratings of satisfaction showed that of the 7 patients, 5 were very satisfied or satisfied and 2 were unsatisfied. Of the patients who were unsatisfied, the mean active forward flexion was 48.5° and the mean Constant score was 31. Of the 2 patients who were unsatisfied, 1 had radial nerve palsy and lymph edema because of postoperative complications that occurred immediately after the operation. Radial nerve palsy was speculated to have occurred as the increase in the size of exploration caused traction in the surrounding structures. However, the patient showed improvement at 5 months of postoperative follow-up. Active forward elevation of the patient was restricted to 60°, and the Constant score was 28. The patient had received a mastectomy on the same side 9 months earlier, which was suspected to have caused the postoperative lymph edema and persistent pain by blocking the lymphatic channel of the incision site. The other patient who was unsatisfied with the clinical outcome had received a second-stage revision due to deep infection, and the causal bacterium was identified to be methicillin-resistant Staphylococcus aureus. We speculate that being unsatisfied may be attributed to the length of time required for the revision, as it took 6 months to remove the implant, control the infection, and then finally perform the second revision.
In the preoperative radiological evaluation, 2 patients showed loosening around the humeral stem, 3 patients showed superior instability, 2 patients showed glenoid arthritis, and 1 patient showed glenoid loosening. In the postoperative radiological evaluation, no radiolucency was observed around the base plate or humeral stem, and grade I scapular notching was observed in 3 patients. The postoperative humeral component showed a mean distalization of 23 mm and a mean medialization of 18 mm. No postoperative instability or dislocation was observed.
The number of shoulder arthroplasties performed has been increasing each year.15) As the number of primary arthroplasty increases, the need for revision arthroplasty is also increasing.16) Prior to the introduction of RTSA by Paul Grammont in 1985, resection arthroplasty, arthrodesis, and conversion to hemiarthroplasty had been performed as a salvage procedure for failed arthroplasty, but they failed to show reliable pain relief or functional improvements.171819) RTSA can be used for revision surgery for failed TSA. Walker et al.20) reported that after revision RTSA on 22 patients with failed TSA, pain was relieved and functional outcomes were improved with a decrease in VAS score (from 5 preoperatively to 1.5 postoperatively) and an increase in American Shoulder and Elbow Surgeons (ASES) score (from 38.5 preoperatively to 67.5 postoperatively). In particular, forward flexion showed an increase from 50° preoperatively to 130° postoperatively, resulting in 89% of the patients being satisfied with the outcome.20) Kelly et al.21) also performed revision RSA in 30 patients, where the final follow-up showed increases in Constant score from 24 preoperatively to 65 postoperatively and in ASES score from 55 preoperatively to 72 postoperatively. Moreover, they observed an improvement in ASES pain score from 6.6 preoperatively to 1.6 postoperatively. As 24 of 30 patients (80%) were shown to be very satisfied or satisfied, RSA was reported to be potentially effective as a salvage procedure for failed arthroplasty. Results of revision RSA can vary depending on the kind of primary arthroplasty performed.8) Levy et al.22) performed revision surgery on 29 cases of failed hemiarthroplasty due to glenoid erosion, and 24-month follow-up monitoring showed an increase in ASES score from 22.3 preoperatively to 57.5 postoperatively and an improvement in SST score from 0.9 preoperatively to 2.6 postoperatively, indicating that RSA was an effective salvage procedure. However, complications occurred in 6 patients (32%) and glenoid bone loss after humeral hemiarthroplasty was located primarily in the posterior glenoid, making stable fixation of the base plate for glenoid challenging. Thus, they stated that preoperative CT should be used to identify posterior erosion for determining whether a bone graft is required.22) Moreover, as attempting to remove enough cement from the glenoid side to obtain viable bone bleeding glenoid can increase the risk of cavitary defect, the number of cases that require glenoid bone graft also inceases.20) In the present study, strut iliac bone graft was performed in 1 patient due to sizable glenoid bone loss after the glenoid component was removed. Revision RTSA for failed RSA was reported to yield less favorable outcomes than revision RTSA for other arthroplasties, because second-stage revision surgery was needed due to infection in majority cases.23) The present study also showed that patients who underwent second-stage revision RTSA after implant removal due to infection at 6 months after the initial RSA at another medical institute showed much less favorable clinical outcome and lower subjective satisfaction than the other patients. Recently, as a platform system composed of a versatile humeral stem and metal back glenoid can be used during revision RTSA for failed TSA, the operation can be performed conveniently without removal of the humeral stem and result in lower complication rates.24) In one of our cases, conversion RTSA was performed by inserting only the adapter without removing the humeral stem due to the humeral component of the hemiarthroplasty being firmly fixed, and thus the operation time was reduced. In this patient, VAS score decreased from 6 preoperatively to 1 postoperatively. UCLA score increased from 11 preoperatively to 21 postoperatively, Constant score increased from 17 preoperatively to 34 postoperatively. However, preoperative forward flexion of 0° improved only to 20° postoperatively, which made active exercise mostly impossible. The reason for this was speculated to be the diminished function of the deltoid caused by excessive detachment of the deltoid muscle insertion during the adapter insertion process due to the adapter not being inserted well for being too thick. Complications that can occur after revision RTSA include scapular notching, instability, infection, aseptic glenoid loosening, humeral fracture, and nerve palsy.6) In the present study, 1 patient experienced temporary radial nerve palsy.
Flury et al.9) reported results of revision RTSA: there was a statistically significant improvement in ROM, but active flexion/abduction were approximately 90°, which was not comparable to the results of primary RTSA. In addition, they mentioned that although the VAS score for pain decreased from 8.7 to 3.0, the final VAS score was 3, indicating that pain still lingered postoperatively. Despite this, patient satisfaction reached 84%, suggesting that preoperatively severe ROM limitation and extreme pain can offset unfavorable postoperative outcome. The present study also showed that the ROM and VAS score after the revision RTSA improved less than expected. Nevertheless, 5 of the 7 patients indicated very satisfied or satisfied in their subjective rating of satisfaction of the clinical outcome. Therefore, the authors also speculate that severe preoperative pain and ROM limitation affected postoperative satisfaction. The limitations of the present study include the fact that it was retrospectively conducted with a small sample size. However, because revision shoulder arthroplasty cases are not common, and revision RTSA is even less common, we believe that this can be overcome by more experience. However, we can claim that one of the advantages of the study was that all the operations were performed by the same surgeon.
In conclusion, revision RTSA can yield pain relief; however, improvements in motion and function were difficult to achieve. Although ROM or functional outcome were improved from preoperative levels, the improvements were not as significant as expected. Patients were satisfied with the outcomes despite low function score, which is likely to be related to severe preoperative pain and preoperative ROM limitation.
Figures and Tables
Fig. 1
The patient underwent conversion from total shoulder arthroplasty to reverse total shoulder arthroplasty. (A) Initial preoperative radiograph showing superior migration of the prosthesis and radiolucency around the glenoid component. (B) Strut iliac bone graft and screw-type baseplate were implanted to achieve stable fixation of the glenoid component.

Fig. 2
(A) Preoperative radiograph showing the glenoid arthrosis. (B) The patient was managed with reverse total shoulder arthroplasty by using an adapter without revision of the humeral stem because it was securely fixed in the humerus.

Table 1
Demographic Characteristics of Patients Who Underwent Revision Reverse Total Shoulder Arthroplasty

Table 2
Preoperative and Postoperative Range of Motion and Muscle Strength
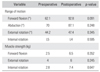
Table 3
Preoperative and Postoperative Activities of Daily Living
References
1. Sassoon AA, Rhee PC, Schleck CD, Harmsen WS, Sperling JW, Cofield RH. Revision total shoulder arthroplasty for painful glenoid arthrosis after humeral head replacement: the nontraumatic shoulder. J Shoulder Elbow Surg. 2012; 21(11):1484–1491.

2. Hattrup SJ. Revision total shoulder arthroplasty for painful humeral head replacement with glenoid arthrosis. J Shoulder Elbow Surg. 2009; 18(2):220–224.

3. Sperling JW, Cofield RH. Revision total shoulder arthroplasty for the treatment of glenoid arthrosis. J Bone Joint Surg Am. 1998; 80(6):860–867.

4. Carroll RM, Izquierdo R, Vazquez M, Blaine TA, Levine WN, Bigliani LU. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: long-term results. J Shoulder Elbow Surg. 2004; 13(6):599–603.

5. Dines JS, Fealy S, Strauss EJ, et al. Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am. 2006; 88(7):1494–1500.

6. Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011; 20(1):146–157.

7. Wall B, Nove-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007; 89(7):1476–1485.
8. Austin L, Zmistowski B, Chang ES, Williams GR Jr. Is reverse shoulder arthroplasty a reasonable alternative for revision arthroplasty? Clin Orthop Relat Res. 2011; 469(9):2531–2537.

9. Flury MP, Frey P, Goldhahn J, Schwyzer HK, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure: midterm results. Int Orthop. 2011; 35(1):53–60.

10. Patel DN, Young B, Onyekwelu I, Zuckerman JD, Kwon YW. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2012; 21(11):1478–1483.

11. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987; (214):160–164.

12. Ellman H, Hanker G, Bayer M. Repair of the rotator cuff: end-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986; 68(8):1136–1144.

13. Sperling JW, Cofield RH, O'Driscoll SW, Torchia ME, Rowland CM. Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elbow Surg. 2000; 9(6):507–513.

14. Lazarus MD, Jensen KL, Southworth C, Matsen FA 3rd. The radiographic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am. 2002; 84(7):1174–1182.

15. Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010; 19(8):1115–1120.

16. Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011; 93(24):2249–2254.

17. Cil A, Veillette CJ, Sanchez-Sotelo J, Sperling JW, Schleck C, Cofield RH. Revision of the humeral component for aseptic loosening in arthroplasty of the shoulder. J Bone Joint Surg Br. 2009; 91(1):75–81.

18. Dimmen S, Madsen JE. Long-term outcome of shoulder arthrodesis performed with plate fixation: 18 patients examined after 3-15 years. Acta Orthop. 2007; 78(6):827–833.

19. Maynou C, Menager S, Senneville E, Bocquet D, Mestdagh H. Clinical results of resection arthroplasty for infected shoulder arthroplasty. Rev Chir Orthop Reparatrice Appar Mot. 2006; 92(6):567–574.
20. Walker M, Willis MP, Brooks JP, Pupello D, Mulieri PJ, Frankle MA. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elbow Surg. 2012; 21(4):514–522.

21. Kelly JD 2nd, Zhao JX, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg. 2012; 21(11):1516–1525.

22. Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br. 2007; 89(2):189–195.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download