Abstract
Background
This study attempts to prove a cause and effect relationship between spine immobilization following posterior fixation for unstable burst fractures and degeneration observed following hardware removal.
Methods
We enrolled 57 patients (259 intervertebral discs [IVDs]) who underwent only posterior instrumentation without fusion for thoracolumbar and lumbar unstable burst fractures. We arbitrarily named the IVD that has an endplate fracture after immobilization using pedicle screws as the fractured endplate and immobilized disc (FEID), the IVD that has no endplate fracture after immobilization using pedicle screws as the nonfractured endplate and immobilized disc (NFEID), and the IVD that has no endplate fracture and no immobilization instrumentation as the normal disc (ND). At 2 years after implant removal, magnetic resonance imaging (MRI) was performed again for comparison. The extent of disc degeneration was classified using the Pfirrmann classification system.
Results
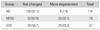
FEIDs were present in 67 levels, NFEIDs in 78 levels, and NDs in 114 levels. According to the Pfirrmann classification, 7.9% of the NDs, 32.1% of the NFEIDs, and 43.3% of the FEIDs were more degenerated at 2 years after implant removal. The FEIDs and NFEIDs were more degenerated than the NDs and the FEIDs were more degenerated than the NFEIDs at statistically significant levels (p < 0.001 for both).
One of the important functions of the intervertebral disc (IVD) is shock absorption with the vertebral endplate that enables spine to flex, extend and twist.1) Degeneration of the IVD is a physiological change associated with aging rather than disease, and it has a close relationship with the endplate. The vertebral endplates are typically less than 1 mm thick, and while this varies considerably across the width of any single disc, they tend to be thinnest in the central region adjacent to the nucleus.123) Moore1) reported that the Schmorl's node is an endplate defect caused by damage such as trauma. Vernon-Roberts4) argued that degenerative changes in the disc are more frequent in persons who have Schmorl's nodes and thus the endplate fracture is related to degenerative changes of the IVD. Some authors reported that pathological signal changes of the IVD on magnetic resonance imaging (MRI) can be observed after spine trauma, whereas others reported spine trauma has no relationship with pathological signal changes of the IVD.56)
The claim that endplate fractures are closely related to degenerative changes of the IVD is not novel. Kirkaldy-Willis et al.7) insisted that the spine becomes stabilized due to the limited movement with the progression of degeneration, whereas Stokes and Iatridis8) insisted that immobilization of the spine is related with degeneration of the IVD. Likewise, the relationship between spine immobilization and degeneration of the IVD is still controversial. To date, there have been many studies conducted on the effect of only endplate fractures or only immobilization on degeneration of the IVD. In contrast, this study evaluates degeneration of normal discs, immobilized discs, and immobilized discs with endplate fractures among patients who underwent posterior instrumentation without fusion for unstable burst fractures and instrumentation removal after fracture site healing. The aim of this study was to determine the relationship between degeneration of the IVD and spine immobilization under the hypothesis that immobilization accelerates degenerative changes.
We enrolled 57 patients who had been treated between September 1, 2003 and August 31, 2012 and met our inclusion and exclusion criteria (Table 1). All patients with an unstable burst fracture (Thoracolumbar Injury Classification and Severity Score [TLICS] > 5) which was not secondary to osteoporosis or pathological were managed by posterior instrumentation. This study was approved by the Institutional Review Board of Daegu Catholic University Medical Center (No. CR-14-055).
The surgery was performed 2.4 days (range, 0 to 5 days) after injury using only the posterior approach. After insertion of a pedicle screw-rod system into the vertebra above and below the fractured vertebra via a paramedian approach between the multifidus and longissimus muscle, fixation was achieved by connecting rods while producing distraction. The insertion trajectory of the pedicle screw was from the lateral side of the facet joint to the vertebral body, striving for least violation of the adjacent facet joint. No laminotomies or laminectomies were performed. The fracture site was reduced by ligamentotaxis. No procedures to gain fusion were carried out, and there was no attempt at bone grafting of the vertebral body through the pedicle. If the pedicle of the affected vertebrae was appropriate for pedicle screw insertion, we performed short-segment pedicle fixation involving 2 levels above and 1 level below the affected vertebra. The patients were permitted to ambulate 2 or 3 days postoperatively using an external support such as thoraco-lumbo-sacral orthosis or lumbo-sacral orthosis. Implant removal was carried out between 8 and 14 months after the primary procedure with removal of other extremity implants.
All patients were evaluated using plain radiographs, computed tomography (CT) scans, and MRI at the time of injury. Endplate fractures were diagnosed by presence of a displaced fracture line through the endplate on CT and MRI (Fig. 1). Based on MRI findings, we named the IVD that has an endplate fracture after immobilization using pedicle screws as fractured endplate and immobilized disc (FEID), the IVD that has no endplate fracture after immobilization using pedicle screws as nonfractured endplate and immobilized disc (NFEID), and the IVD that has no endplate fracture and no immobilization instrumentation as normal disc (ND) (Fig. 2). MRI was also performed 2 years after implant removal.
The degree of IVD degeneration was assessed using the Pfirrmann classification system9) (Table 2). The two MRI scans obtained at the time of injury and at 2 years after implant removal were reviewed by an orthopedic spine surgeon who was neither related to this study and nor participated in the surgery. If the difference in the extent of degeneration of the IVD on MRI between at the time of injury and at 2 years after instrument removal was over grade 2, degenerative changes were considered to have progressed (Fig. 3).
Among 57 patients, 40 were men and 17 were women. Their mean age at the time of injury was 39 ± 10.1 years (range, 16 to 53 years). Fractured levels were T12 in 10 (17.5%), L1 in 10 (17.5%), L2 in 19 (33.3%), and L3 in 18 (31.6%). More detailed disc distribution is shown in Table 3. The mean follow-up period (from the first MRI to the last MRI) was 28 months (range, 24 to 32 months).
Among 259 IVDs of 57 patients, FEIDs were present in 67 levels, NFEIDs in 78 levels, and NDs in 114 levels. According to the Pfirrmann classification, 9 levels of the NDs (7.9%), 25 levels of the NFEIDs (32.1%), and 29 levels of the FEIDs (43.3%) were more degenerated at 2 years after implant removal. The NFEIDs and FEIDs were more degenerated than the NDs statistically significantly (p < 0.001). The FEIDs were more degenerated than the NFEIDs statistically significantly (p < 0.001). The highest percentage of degeneration was identified in the FEIDs followed by the NFEIDs and then NDs (Table 4).
A network of microscopic blood vessels penetrates the endplates during development of the growing spine, principally to provide nutrition for the disc, before disappearing around the time of skeletal maturity.110) Apart from a sparse vascular supply in the outer lamellae of the annulus, mature discs are almost totally reliant on diffusion of essential solutes across the endplates for nutrition and metabolic exchanges.111) An endplate fracture may induce pathological signal changes of the IVD on MRI, and inflammatory reaction accelerates degenerative changes of the IVD.561213) As mentioned above, there are many studies demonstrating the important role of the endplate in the IVD metabolism.17811)
Narrowing of the disc space has also been commonly observed after fractures of the thoracolumbar spine and associated with progressive kyphosis and pain in patients treated conservatively or with recurrent kyphosis after posterior reduction and fixation.141516171819) It is unclear whether this narrowing is a result of biochemical changes, as seen in degenerative disc disease, or narrowing represents an adaptation to changes in the morphology of the disc space as a result of the bony endplate fracture.20)
Some studies argued that radiological and histological disc degeneration can occur after 30s without trauma history and subjective symptoms.2122) In contrast, Oner et al.20) suggested that radiological signal changes after trauma means morphological changes rather than degenerative changes, and it is not degenerative disc space narrowing but a morphological change that occurs when the disc material leaks into the fractured site of an endplate of the vertebral body. This disc material can cause therapeutic failure or a secondary kyphotic change, but an endplate fracture alone is not enough for explaining IVD degeneration. Variable IVD injury patterns and therapeutic patterns are important for long-term stability of the spine,23) but not much else is known about adjacent disc degeneration and healing process.20)
There are many studies on the relationship of spinal cyclic loading and disc degeneration.24) Stokes and Iatridis8) noted that the mechanical condition of the IVD has a “safe window” and overloading of the IVD due to disc injury or delayed repair can cause problems. Immobilization may disrupt hemostasis of the IVD and accelerate degeneration of the IVD. As such, many studies insist that human spine degeneration can occur in immobilization or hypermobility of the spine.825) Therefore, controlled compression on the disc is essential to maintain healthy composition, structure, and mechanical properties of the spine.8)
Roaf observed that the discs are always stronger than the endplate under compression so that compression forces create a fracture of the endplate before causing damage to the IVD.26) According to Modic and Ross,27) endplate fractures do not violate the disc to cause its degeneration, but pedicle screw fixation can reduce cyclic loading to cause disc degeneration.
In this study we compared the MRI scans taken at the time of injury and 2 years after implant removal to evaluate the pedicle screw rigidity, fracture configuration, fracture reduction, underlying anatomy of the spine, stability of the fractured region by sagittal/coronal alignment and other variables according to degenerative changes of each disc.
One of the limitations of our study is the lack of evaluation on adjacent disc degeneration after instrumentation. According to various studies that address adjacent disc degeneration, degenerative changes do not appear to have correlation with clinical symptoms252829) and are observed at least several years and a decade afterward. However, our study dealt with short-term changes at around 4 years after immobilization. Therefore, further studies should be conducted on the relationship between clinical symptoms and degenerative changes in a longer follow-up. Demonstration of radiographic changes alone without clinical correlation is of little value. However, in the current study, we thought there was no need to assess clinical symptoms because the FEIDs, NFEIDs, and NDs were included in the analysis. It would be possible to determine the correlation between the extent of degeneration and the clinical symptom of each patient after long-term follow-up. Third, the possible difference in the degenerative change of the IVD between the thoracolumbar spine and that of the lumbar was not considered.
In conclusion, this study reaffirms that both endplate fracture and spine immobilization using transpedicular screw fixation without fusion play an important role in disc degeneration. The incidence of disc degeneration was highest in the fractured endplate and immobilization group followed by the immobilized and no fracture group. The group with normal appearing discs without immobilization showed the lowest incidence of disc. The differences among groups were statistically significant. Therefore, we think that spine immobilization with transpedicular screws has a significant influence on disc degeneration, and endplate fractures accelerate the degeneration process. Moreover, it appears that endplate fractures combined with spine immobilization without fusion have a greater impact on the degenerative process of IVD than endplate fractures alone.
Figures and Tables
Fig. 1
Displaced endplate fracture was diagnosed based on sagittal (A) and coronal (B) images of computed tomography.

Fig. 2
Intervertebral discs (IVDs) after instrumentation for spine fracture. ND: normal disc, an IVD that has no endplate fracture and no immobilization. NFEID: nonfractured endplate and immobilized disc, an IVD that has no endplate fracture but is immobilized using pedicle screws. FEID: fractured endplate and immobilized disc, an IVD that has endplate fracture and is immobilized using pedicle screws. *Fractured vertebra.
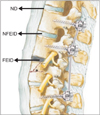
Fig. 3
Serial magnetic resonance imaging (MRI) showing more degenerative changes. (A) MRI imaging of the fractured vertebral body and injured endplate (white square) at the time of injury shows grade 1 degeneration. (B) Disc is homogeneous with bright hyperintense white signal intensity and normal disc height (white arrow). (C) MRI imaging of the treated vertebral body and endplate (yellow square) at 2 years after removal surgery shows grade 3 degeneration. (D) Disc is inhomogenous with an intermittent gray signal intensity and disc height is slightly or moderately decreased (yellow arrow).
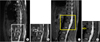
Table 1
Inclusion Criteria and Exclusion Criteria

Table 2
Classification System for Lumbar Disc Degeneration Based on Routine Magnetic Resonance Imaging

Based on appearance on fast spin echo T2-weighted sagittal images of the spine.
Adapted from Pfirrmann et al.9) with permission from Wolters Kluwer Health.
Table 3
Disc Level Distribution
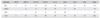
| Variable | T9-10 | T10-11 | T11-12 | T12-L1 | L1-2 | L2-3 | L3-4 | L4-5 | Total |
|---|---|---|---|---|---|---|---|---|---|
| ND | 6 | 10 | 14 | 18 | 19 | 10 | 19 | 18 | 114 |
| NFEID | - | 6 | 6 | 18 | 19 | 11 | 18 | - | 78 |
| FEID | - | - | 10 | 12 | 19 | 26 | - | - | 67 |
| Total | 6 | 16 | 20 | 48 | 57 | 47 | 19 | 18 | 259 |
References
1. Moore RJ. The vertebral endplate: disc degeneration, disc regeneration. Eur Spine J. 2006; 15:Suppl 3. S333–S337.

2. Edwards WT, Zheng Y, Ferrara LA, Yuan HA. Structural features and thickness of the vertebral cortex in the thoracolumbar spine. Spine (Phila Pa 1976). 2001; 26(2):218–225.

3. Roberts S, Menage J, Urban JP. Biochemical and structural properties of the cartilage end-plate and its relation to the intervertebral disc. Spine (Phila Pa 1976). 1989; 14(2):166–174.

4. Vernon-Roberts B. Age-related and degenerative pathology of intervertebral discs and apophyseal joints. In : Jayson MI, editor. The lumbar spine and back pain. 4th ed. Edinburgh, Scotland: Churchill Livingstone;1992. p. 17–41.
5. Ghanem N, Uhl M, Muller C, et al. MRI and discography in traumatic intervertebral disc lesions. Eur Radiol. 2006; 16(11):2533–2541.

6. Oner FC, van Gils AP, Dhert WJ, Verbout AJ. MRI findings of thoracolumbar spine fractures: a categorisation based on MRI examinations of 100 fractures. Skeletal Radiol. 1999; 28(8):433–443.

7. Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, Reilly J. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine (Phila Pa 1976). 1978; 3(4):319–328.

8. Stokes IA, Iatridis JC. Mechanical conditions that accelerate intervertebral disc degeneration: overload versus immobilization. Spine (Phila Pa 1976). 2004; 29(23):2724–2732.

9. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001; 26(17):1873–1878.

10. Taylor JR. Growth of human intervertebral discs and vertebral bodies. J Anat. 1975; 120(Pt 1):49–68.
11. Holm S, Maroudas A, Urban JP, Selstam G, Nachemson A. Nutrition of the intervertebral disc: solute transport and metabolism. Connect Tissue Res. 1981; 8(2):101–119.

12. Knop C, Blauth M, Buhren V, et al. Surgical treatment of injuries of the thoracolumbar transition. 3: follow-up examination. Results of a prospective multi-center study by the “Spinal” Study Group of the German Society of Trauma Surgery. Unfallchirurg. 2001; 104(7):583–600.
13. Haschtmann D, Stoyanov JV, Gedet P, Ferguson SJ. Vertebral endplate trauma induces disc cell apoptosis and promotes organ degeneration in vitro. Eur Spine J. 2008; 17(2):289–299.

14. Malcolm BW, Bradford DS, Winter RB, Chou SN. Post-traumatic kyphosis: a review of forty-eight surgically treated patients. J Bone Joint Surg Am. 1981; 63(6):891–899.

15. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 8(8):817–831.

16. Lindsey RW, Dick W. The fixateur interne in the reduction and stabilization of thoracolumbar spine fractures in patients with neurologic deficit. Spine (Phila Pa 1976). 1991; 16:3 Suppl. S140–S145.

17. Steindl A, Schuh G. Late results after lumbar vertebrae fracture with Lorenz Bohler conservative treatment. Unfallchirurg. 1992; 95(9):439–444.
18. Akbarnia BA, Crandall DG, Burkus K, Matthews T. Use of long rods and a short arthrodesis for burst fractures of the thoracolumbar spine: a long-term follow-up study. J Bone Joint Surg Am. 1994; 76(11):1629–1635.

19. Speth MJ, Oner FC, Kadic MA, de Klerk LW, Verbout AJ. Recurrent kyphosis after posterior stabilization of thoracolumbar fractures: 24 cases treated with a Dick internal fixator followed for 1.5-4 years. Acta Orthop Scand. 1995; 66(5):406–410.

20. Oner FC, van der Rijt RR, Ramos LM, Dhert WJ, Verbout AJ. Changes in the disc space after fractures of the thoracolumbar spine. J Bone Joint Surg Br. 1998; 80(5):833–839.

21. Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt KF, Nerlich AG. Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo Award in basic science. Spine (Phila Pa 1976). 2002; 27(23):2631–2644.
22. Cheung KM, Karppinen J, Chan D, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine (Phila Pa 1976). 2009; 34(9):934–940.

23. Lin RM, Panjabi MM, Oxland TR. Functional radiographs of acute thoracolumbar burst fractures: a biomechanical study. Spine (Phila Pa 1976). 1993; 18(16):2431–2437.
24. Ching CT, Chow DH, Yao FY, Holmes AD. The effect of cyclic compression on the mechanical properties of the inter-vertebral disc: an in vivo study in a rat tail model. Clin Biomech (Bristol, Avon). 2003; 18(3):182–189.

25. Kumar MN, Jacquot F, Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 2001; 10(4):309–313.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download