Abstract
Background
The aim of this study is to evaluate the effect of depression, anxiety, and optimism on postoperative satisfaction and clinical outcomes in patients who underwent less than two-level posterior instrumented fusions for lumbar spinal stenosis and degenerative spondylolisthesis.
Methods
Preoperative psychological status of subjects, such as depression, anxiety, and optimism, was evaluated using the Hospital Anxiety and Depression Scale (HADS) and the Revised Life Orientation Test (LOT-R). Clinical evaluation was determined by measuring changes in a visual analogue scale (VAS) and the Oswestry Disability Index (ODI) before and after surgery. Postoperative satisfaction of subjects assessed using the North American Spine Society lumbar spine questionnaire was comparatively analyzed against the preoperative psychological status. The correlation between patient's preoperative psychological status (depression, anxiety, and optimism) and clinical outcomes (VAS and ODI) was evaluated.
Results
VAS and ODI scores significantly decreased after surgery (p < 0.001), suggesting clinically favorable outcomes. Preoperative psychological status of patients (anxiety, depression, and optimism) was not related to the degree of improvement in clinical outcomes (VAS and ODI) after surgery. However, postoperative satisfaction was moderately correlated with optimism.
As the population ages, the prevalence of degenerative spine disease patients (e.g., spinal stenosis and degenerative spondylolisthesis) has increased, and the incidence of surgical treatment for such patients has risen accordingly.1) Although surgery for degenerative spine disease patients who complain of intermittent claudication, persistent back pain, and radiating pain in the lower limbs is known to be an extremely effective treatment, it has not always shown satisfactory outcomes for everyone.23) Many studies report patient satisfaction rates of 60%–80%.45)
A variety of factors that influence postoperative satisfaction have been examined and identified in an effort to improve patient satisfaction with spinal surgery. Patient factors, such as sex, age, and body mass index (BMI) and disease factors, such as diagnosis, prevalence period, and complications can affect patient satisfaction with spinal surgery.67) Psychological status before surgery is also believed to influence the outcome of surgery and satisfaction. Spengler et al.8) reported that psychological factors had a correlation with the outcomes of elective discectomy for herniation of a lumbar disc. Another study showed that psychological disorders affected outcomes of chronic lower back pain treatment.9)
In general, patients who receive surgery for degenerative spine disease complain of depression and anxiety related to pain or discomfort in daily living activities, but some patients do not. So we asked all patients who received surgery in one spine center to complete questionnaires on the visual analogue scale (VAS), Oswestry Disability Index (ODI), Hospital Anxiety and Depression Scale (HADS), and Revised Life Orientation Test (LOT-R) and the North American Spine Society (NASS) lumbar spine questionnaire before surgery and during follow-up in the outpatient office since 2010.
The present study attempted to evaluate the effect of depression, anxiety, and optimism on postoperative patient satisfaction and clinical outcomes by analyzing the collected data.
This study is approved by Institutional Review Board of Hanyang University Guri Hispital (No. 2012-003) on Human Subjects Research and Ethics Committees. For this retrospective cohort study, we initially enrolled 339 patients who underwent less than two-level posterior instrumented fusions for lumbar spinal stenosis and degenerative spondylolisthesis between January 2010 and February 2013. They were screened for potential inclusion in the study. Thirty-six patients refused to sign the informed consent. Forty-two patients were lost to follow-up; they did not visit the outpatient office and could not be contacted via phone. Therefore, 261 patients available for at least 2 years of postoperative follow-up were selected for the retrospective analysis of imaging data and medical records. The inclusion criteria for the study were (1) reasons for surgery were continuation of back pain, radiating pain to the lower extremities, and intermittent claudication despite 3 months of conservative treatment and (2) fusion was needed due to wide decompression or instability. All subjects were diagnosed with degenerative spine disease based on physical examination and magnetic resonance imaging (MRI).
Patients were excluded for any of the following reasons: (1) previous spinal surgery (n = 26); (2) accompanying severe deformities such as degenerative scoliosis (n = 15); and (3) severe comorbidities (n = 14) during follow-up, such as brain infarction or myocardial infarction restricting daily living activities, or revision surgery. Ultimately, total 206 patients were included in the study (Fig. 1). There were 69 males and 137 females with a mean age of 62.4 years (range, 54 to 79 years). The mean duration of symptoms before surgery was 12.7 months (range, 5 to 21 months) (Table 1).
The VAS was used to assess back pain and radiating pain to the lower extremities before and 24 months after surgery. The subjects were asked to choose the score that best corresponds to their pain from 0 point for no pain to 10 points for unbearable pain. The ODI was used to assess disability to perform daily living activities. The ODI comprised of 9 items assessing pain intensity, personal care, lifting, walking, sitting, standing, sleeping, social life, and travelling, excluding sexual activity. Each item contains 6 different degrees of functional disability. Subjects were instructed to select the degree that corresponds most closely to their experience. Clinical improvement was defined as changes in the VAS and ODI before and after surgery, and correlations of these values with preoperative optimism, anxiety, and depression scores were analyzed.
Depression, anxiety, and optimism were evaluated using the HADS and LOT-R. The HADS is a patient-oriented survey that assesses anxiety and depression on a 0-4 point scale using 7 items for anxiety and 7 items for depression. Higher scores reflect higher anxiety and depression.10) It is effective in assessing the symptom severity of anxiety and depression in both somatic and psychiatric primary care patients and in the general population.11) The LOT-R is a 10-item survey that evaluates optimism. The raw score is converted to a 100-point scale score, and higher scores reflect an optimistic inclination, while lower scores reflect a pessimistic inclination.12) A recent study for analysis of the accuracy of the LOT-R showed that it is a reliable and valid measurement of optimism.13)
The NASS lumbar spine questionnaire was used to evaluate subjects' expectations of surgery and fulfillment of their expectations.14) Expectations were measured using a 5-point scale on 8 items: leg pain, back pain, walking capacity, independence in everyday activities, sporting activities, general physical capacity, frequency and quality of social contacts, and mental well-being. Higher scores (range, 0 to 40 points) reflect greater expectations of surgery. Satisfaction was measured using a 2-point scale on the same 8 items, and higher scores (range, 0 to 16 points) reflect greater satisfaction. Expectations of surgery were assessed before surgery. Satisfaction after surgery against preoperative expectations was analyzed using the questionnaire completed 24 months after surgery. Subjects were also asked to identify the item they expected to improve the most after surgery among the following 5 items: leg pain, back pain, walking capacity, independence in everyday activities, and general physical capacity. The greatest satisfaction they experienced was also identified through the survey completed 24 months after surgery.
SPSS ver. 19.0 (IBM Co., Armonk, NY, USA) was used for the analyses. Pearson correlation analysis was used to determine correlations among preoperative depression, anxiety, and optimism of patients, changes in VAS and ODI scores before and after surgery, preoperative expectations, and satisfaction after surgery. Multivariate analysis was performed by ordinal regression for each dependent variable studied. Reported values for each independent variable include the coefficient β of the regression fit. Satisfaction with surgery was tested using an independent two-sample t-test. Statistical significance was defined as p < 0.05.
The degree of pain measured by the VAS was significantly reduced from 7.23 ± 1.45 before surgery to 4.04 ± 1.71 at 24 months after surgery (p < 0.001). Subjective disability score on the ODI was also significantly reduced from 58.95 ± 18.23 before surgery to 32.10 ± 8.10 at 24 months after surgery, indicating clinically favorable outcomes (p < 0.001).
LOT-R score before surgery was 54.92±17.43. The anxiety score on the HADS was 8.78 ± 4.51 and the depression score on the HADS was 9.33 ± 4.85 (Table 2). A correlation analysis of preoperative psychological status and clinical outcomes based on changes in VAS and ODI scores showed that optimism was weakly correlated with improvement in VAS and ODI (r = 0.215, p < 0.001; r = 0.296, p < 0.001, respectively). Anxiety and depression were also weakly correlated with improvement in ODI (r = –0.300, p < 0.001; r = –0.276, p < 0.001, respectively). Improvement in VAS was not significantly correlated with preoperative anxiety or depression (r = –0.054, p = 0.442; r = –0.116, p = 0.096, respectively) (Table 3). Expectations of subjects before surgery based on the NASS lumbar spine questionnaire was 26.53 ± 3.78 and satisfaction after surgery was 9.62 ± 5.35 (Table 2). A correlation analysis of the NASS questionnaire and preoperative psychological status demonstrated that preoperative expectations and postoperative satisfaction had a moderately positive correlation with only optimism (r = 0.437, p < 0.001; r = 0.562, p < 0.001, respectively) (Table 3).
On the multivariate analysis performed by ordinal regression, changes in the VAS and ODI and expectations and satisfaction on the NASS questionnaire were used as dependent variables. Results were quite different from those of the univariate analysis. Anxiety was significantly moderately correlated with the VAS (β = 0.448, p = 0.002). Factors associated with ODI showed a moderate correlation with anxiety (β = 0.353, p = 0.014). When preoperative expectation scale was used as a dependent variable, optimism was significantly correlated (β = 0.464, p < 0.001). Optimism and anxiety were significantly highly correlated with postoperative satisfaction (β = 0.805, p < 0.001; β = 0.681, p = 0.016, respectively). Other independent variables (sex, age) showed no correlation with dependent variables. There was no multicollinearity problem between variables (Table 4).
In this study, relationships among preoperative anxiety, depression, and optimism, clinical outcomes, and postoperative satisfaction (improvement of pain and disability) were examined in patients who received spinal fusion for lumbar spinal stenosis and degenerative spondylolisthesis. There have been many studies across diverse medical fields on the effects of psychosocial aspects of patients with chronic diseases on the natural course and treatment outcomes of diseases. One study of patients who received open-heart surgery for coronary heart disease reported that expectations of surgery and preoperative anxiety and depression can affect the recovery of patients.15) In the field of orthopedic surgery, there has been increasing attention on such psychological factors. For example, one study reported that depression is a factor that can predict undesirable treatment outcomes in patients with chronic back pain.161718) Another study using the Minnesota Multiphasic Personality Inventory (MMPI) on 135 herniated lumbar intervertebral disc patients found that satisfaction with surgery decreases with increasing symptomatology of depression. 19) In a recent study, Pincus et al.20) reported that severe psychological distress, depression, and somatization can contribute to chronic development of back pain. In a study using Zung Self-Rating Depression Scale and a modified somatic perception questionnaire (MSPQ), the authors insisted that depression and heightened somatic anxiety are associated with disability and quality of life, but not with pain.21) Pollock et al.22) used the Distress and Risk Assessment Method (DRAM) to analyze improvements in the VAS and ODI after surgery in 74 patients who received posterior lumbar interbody fusion. They classified patients based on the preoperative psychological status into normal, risk, depression, and somatization groups. They found that the somatization group showed weaker improvement in VAS and ODI after surgery compared to other groups, indicating that preoperative psychological status can influence postoperative clinical outcomes. In contrast, Okoro and Sell23) found no difference in the degree of improvement in VAS and ODI after surgery among patients who underwent elective surgery (discectomy or decompression) and were classified using the DRAM.
In the current study, we investigated correlations between clinical outcomes and preoperative anxiety, depression, and optimism assessed using the HADS and LOT-R. There has been no article that uses the HADS and LOT-R in spine surgery patients. However, the accuracy of HADS and LOT-R have been validated in some studies.1113) Results observed in our patients were different from our expectations. The VAS and ODI were less correlated with psychological factors, such as anxiety, depression, and optimism. While the preoperative psychological status of patients may not directly affect the degree of improvement in subjective pain and disability after surgery, the multi-variate analysis showed that anxiety is a significant factor to be considered before surgery: anxiety was moderately correlated with the VAS and ODI.
Mondloch et al.24) performed a systematic review of studies that examined the correlations between expectations for recovery and clinical outcomes. They found that 15 out of 16 papers reported moderate or greater correlations between positive expectations and desirable clinical outcomes. In one study of herniated lumbar intervertebral disc patients, Lutz et al.25) reported better clinical outcomes in patients with higher expectations of surgery. In our study, the correlation between expectations—previously reported to influence the clinical outcomes—and preoperative psychological status of patients was analyzed. Optimistic patients reported higher expectations of surgery. Patient's satisfaction after surgery was also correlated with optimism. It showed that optimistic patients may get more satisfaction from their expectations. Additional analyses on the item that patients expected would improve the most and the item that they rated as showing the greatest satisfaction after surgery were performed. The results showed that patients expected the greatest improvement in walking capacity and leg pain. On postoperative satisfaction, patients reported that they experienced the greatest satisfaction with walking capacity and leg pain. For most patients, preoperative expectations were fulfilled. This suggests that clinical outcomes can be improved by increasing patients' expectations of surgery based on careful evaluation of psychological status prior to surgery, increasing motivation for surgery, and proper management. However, we must not ignore the possibility that increasing the expectation could lead to reduced patient satisfaction if expectations were not met. All these statistical results suggest that optimistic perspective is a significant psychological factor that influences clinical outcomes after spine surgery for lumbar spinal stenosis and degenerative spondylolisthesis.
Several limitations should be considered in interpreting our findings. Firstly, changes in psychological status after surgery were not evaluated. Since this study focused on analyzing the effect of preoperative psychological status on postoperative satisfaction and clinical outcomes, the psychological status of patients after surgery was not evaluated. Considering that the psychological status of patients may change after surgical treatment, additional studies are needed to investigate correlations between postoperative psychological status and clinical outcomes. Secondly, other demographic factors that may affect postoperative satisfaction and clinical outcomes, such as occupation, educational background, or medical history, were not evaluated. However, previous studies have demonstrated that such patient factors can influence clinical outcomes and postoperative satisfaction.67) Thirdly, we checked VAS scores for both back pain and leg pain and then used the higher VAS score between back pain and leg pain scores for analysis. Lastly, there was a lack of distinction between state anxiety and trait anxiety. The same limitation was also observed with depression. Although preoperative anxiety and depression status of the patients might have been affected by the fact they would undergo a surgery, we did not consider the distinct characteristics of anxiety and depression in this study.
In summary, anxiety and optimism before surgery might be correlated with the degree of improvement in subjective disability after surgery in terms of satisfaction and clinical outcomes. Therefore, careful evaluation and proper management of the preoperative psychological status of patients should be conducted in order to predict clinical outcomes and increase patient satisfaction. Further research is needed to investigate clinically useful methods to improve the preoperative psychological status.
References
1. Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 2005; 30(12):1441–1445. PMID: 15959375.

2. Katz JN, Stucki G, Lipson SJ, Fossel AH, Grobler LJ, Weinstein JN. Predictors of surgical outcome in degenerative lumbar spinal stenosis. Spine (Phila Pa 1976). 1999; 24(21):2229–2233. PMID: 10562989.

3. Junge A, Dvorak J, Ahrens S. Predictors of bad and good outcomes of lumbar disc surgery: a prospective clinical study with recommendations for screening to avoid bad outcomes. Spine (Phila Pa 1976). 1995; 20(4):460–468. PMID: 7747230.
4. Turner JA, Ersek M, Herron L, Deyo R. Surgery for lumbar spinal stenosis: attempted meta-analysis of the literature. Spine (Phila Pa 1976). 1992; 17(1):1–8. PMID: 1531550.
5. Hoffman RM, Wheeler KJ, Deyo RA. Surgery for herniated lumbar discs: a literature synthesis. J Gen Intern Med. 1993; 8(9):487–496. PMID: 8410420.
6. Ekman P, Moller H, Hedlund R. Predictive factors for the outcome of fusion in adult isthmic spondylolisthesis. Spine (Phila Pa 1976). 2009; 34(11):1204–1210. PMID: 19444068.

7. Bernard TN Jr. Repeat lumbar spine surgery: factors influencing outcome. Spine (Phila Pa 1976). 1993; 18(15):2196–2200. PMID: 8278831.
8. Spengler DM, Ouellette EA, Battie M, Zeh J. Elective discectomy for herniation of a lumbar disc: additional experience with an objective method. J Bone Joint Surg Am. 1990; 72(2):230–237. PMID: 2303509.

9. Daubs MD, Norvell DC, McGuire R, et al. Fusion versus nonoperative care for chronic low back pain: do psychological factors affect outcomes? Spine (Phila Pa 1976). 2011; 36(21 Suppl):S96–S109. PMID: 21952192.
10. Huston GJ. The Hospital Anxiety and Depression Scale. J Rheumatol. 1987; 14(3):644. PMID: 3498040.
11. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002; 52(2):69–77. PMID: 11832252.
12. Glaesmer H, Rief W, Martin A, et al. Psychometric properties and population-based norms of the Life Orientation Test Revised (LOT-R). Br J Health Psychol. 2012; 17(2):432–445. PMID: 22106985.

13. Steca P, Monzani D, Greco A, Chiesi F, Primi C. Item response theory analysis of the life orientation test-revised: age and gender differential item functioning analyses. Assessment. 2015; 22(3):341–350. PMID: 25078402.
14. Daltroy LH, Cats-Baril WL, Katz JN, Fossel AH, Liang MH. The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine (Phila Pa 1976). 1996; 21(6):741–749. PMID: 8882698.
15. Chunta KS. Expectations, anxiety, depression, and physical health status as predictors of recovery in open-heart surgery patients. J Cardiovasc Nurs. 2009; 24(6):454–464. PMID: 19858954.
16. Cashion EL, Lynch WJ. Personality factors and results of lumbar disc surgery. Neurosurgery. 1979; 4(2):141–145. PMID: 440545.

17. Long CJ. The relationship between surgical outcome and MMPI profiles in chronic pain patients. J Clin Psychol. 1981; 37(4):744–749. PMID: 6458625.

18. Herron L, Turner JA, Ersek M, Weiner P. Does the Millon Behavioral Health Inventory (MBHI) predict lumbar laminectomy outcome? A comparison with the Minnesota Multiphasic Personality Inventory (MMPI). J Spinal Disord. 1992; 5(2):188–192. PMID: 1606377.

19. Dvorak J, Gauchat MH, Valach L. The outcome of surgery for lumbar disc herniation: I. a 4-17 years' follow-up with emphasis on somatic aspects. Spine (Phila Pa 1976). 1988; 13(12):1418–1422. PMID: 3212575.
20. Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. pine (Phila Pa 1976). 2002; 27(5):E109–E120.

21. Chaichana KL, Mukherjee D, Adogwa O, Cheng JS, McGirt MJ. Correlation of preoperative depression and somatic perception scales with postoperative disability and quality of life after lumbar discectomy. J Neurosurg Spine. 2011; 14(2):261–267. PMID: 21214315.

22. Pollock R, Lakkol S, Budithi C, Bhatia C, Krishna M. Effect of psychological status on outcome of posterior lumbar interbody fusion surgery. Asian Spine J. 2012; 6(3):178–182. PMID: 22977697.

23. Okoro T, Sell P. The prediction of outcome in somatised patients undergoing elective lumbar surgery. J Bone Joint Surg Br. 2009; 91(4):517–521. PMID: 19336814.

24. Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you'll do? A systematic review of the evidence for a relation between patients' recovery expectations and health outcomes. CMAJ. 2001; 165(2):174–179. PMID: 11501456.
25. Lutz GK, Butzlaff ME, Atlas SJ, Keller RB, Singer DE, Deyo RA. The relation between expectations and outcomes in surgery for sciatica. J Gen Intern Med. 1999; 14(12):740–744. PMID: 10632818.

Fig. 1
Flow diagram illustrating study design. VAS: visual analogue scale, ODI: Oswestry Disability Index, HADS: Hospital Anxiety and Depression Scale, LOT-R: Revised Life Orientation Test, NASS: North American Spine Society.
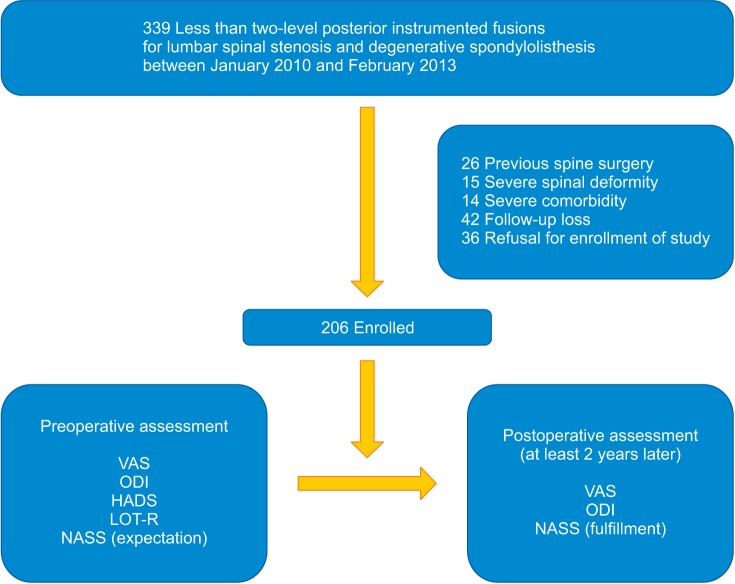
Table 1
Baseline Demographics
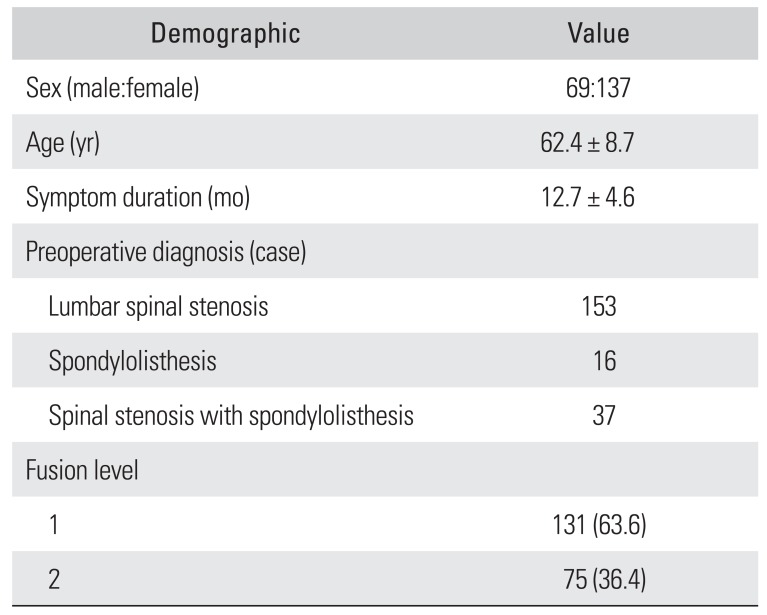
Table 2
Clinical and Psychological Results
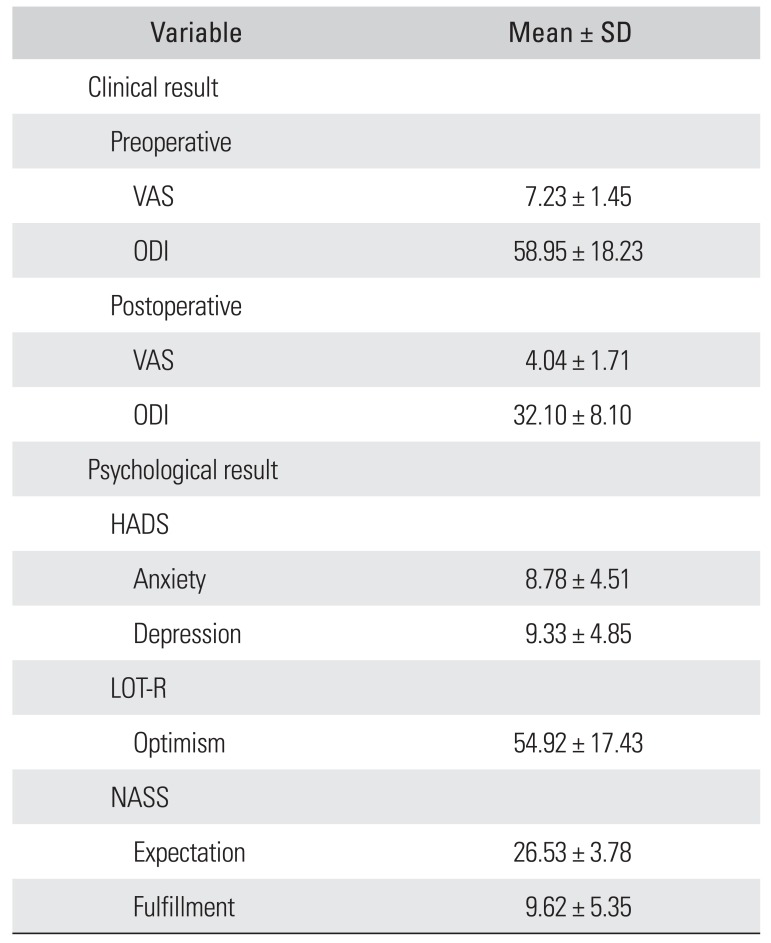
Table 3
Univariate Correlations between Psychological Factors and Clinical Variables
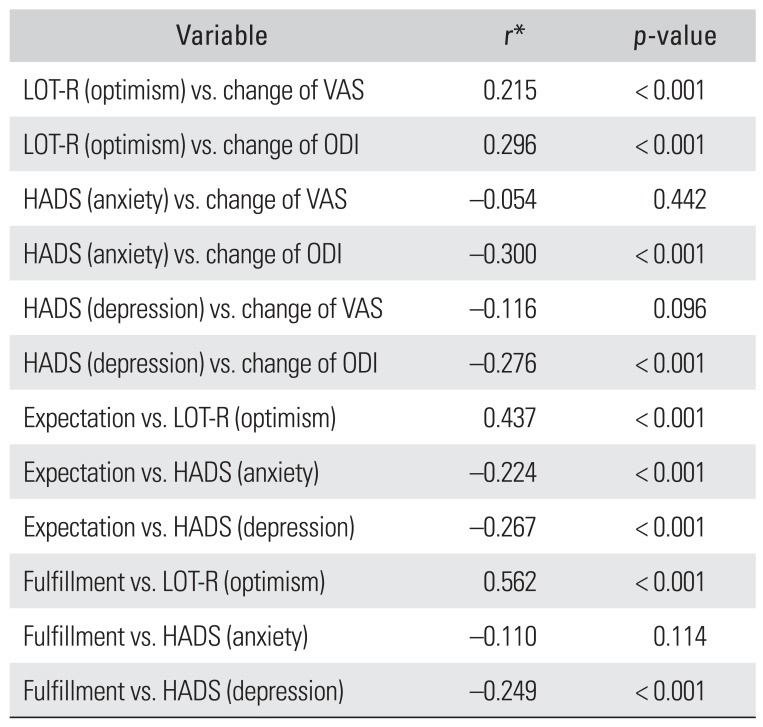
Table 4
Multivariate Correlations between Psychological Factors and Clinical Variables
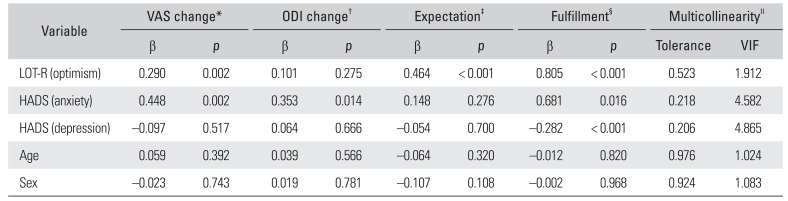
VAS: visual analogue scale, ODI: Oswestry Disability Index, VIF: variance inflation factor, LOT-R: Revised Life Orientation Test, HADS: Hospital Anxiety and Depression Scale.
*R = 0.301, R2 = 0.091, F = 3.939, p = 0.002. †R = 0.355, R2 = 0.126, F = 5.672, p < 0.001. ‡R = 0.454, R2 = 0.206, F = 10.222, p < 0.001. §R = 0.672, R2 = 0.451, F = 32.412, p < 0.001. ∥VIF < 12.0.
Multiple regression analysis, p < 0.05. Multicollinearity statistics, VIF < 12.0.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download