Abstract
Background
Joint replacement surgery is having an increasing demand as national healthcare systems confront an ever ageing population. Surgical complications associated with lower limb arthroplasty are well known but less investigation has been performed examining its effect on air travel, more specifically, unwanted and significant inconvenience caused to travelers going through airport security.
Methods
In lower limb arthroplasty clinics, 50 patients who met our selection criteria were given questionnaires. Ten airport security officers from 4 international airports (London Stansted, London Gatwick, London Heathrow, and Amsterdam Schiphol International Airport) were also given a separate questionnaire. The opinion of the Civil Aviation Authority was also sought.
Results
All 50 patients (mean age, 70.4 years; range, 55 to 84 years) who were presenting in lower limb arthroplasty clinics and who met our selection criteria volunteered to enter the study. Twenty-eight of these patients were female (mean age, 69.1 years; range, 55 to 84 years) and 22 were male (mean age, 71.2 years; range, 58 to 81 years). Of the patients, 14% stated that their joint replacements did not set off the airport security alarm. Responses were received from 10 airport security officers as well. Six airport security officers were male and 4 were female. All of the airport officers were aware of some form of implant identification card with 90% stating that these were useful to them at airport security. Eight-four percent of the patients stated that an implant identification card outlining what joint replacement they possessed and when this had been done would be very useful. Sixteen percent of the patients did not think a card would be beneficial since all of them had set off the airport alarm system only once or less in their lifetime.
In the United Kingdom (UK), joint replacement surgery has been performed as early as the 1960s. Since its introduction, the popularity of this treatment modality has grown exponentially, bringing with it new implants and further technical advances.
A total of 160,000 total hip replacements (THRs) and total knee replacements (TKRs) are performed each year in England and Wales with joint replacement surgery increasing in frequency. This is clearly a common surgical procedure performed in active patients who travel frequently. As such, the potential influence of airport security checks on patient travel is extremely wide ranging.
The influence of replacement implants for patients undergoing security checks like those performed prior to commercial airline flight has been briefly examined in the literature. More recent studies have demonstrated that prosthetic devices are more commonly detected by airport metal detectors1) when compared to previous data.2)
As airport security measures have been heightened and detection apparatus has become more sophisticatedthose who have undergone joint replacement surgery face much greater and more frequent inconvenience, with more invasive security checks becoming a commonplace.3)
Studies examining detection of orthopaedic implants by airport security have been published in the literature;4) however, a formal opinion from airport security and the difficulties that the staff there encounters and a response from The Civil Aviation Authority do not exist.
We set out to establish if the use of an implant identification card would lead to a reduction in the number of invasive searches performed by security staff on those who have undergone lower limb arthroplasty.
This would not only lead to a much improved travel experience for patients but improve safety at airports by diminishing the work load on security staff. With more modern methods of travel being introduced, such as biometric chipped ePassports, it is essential that medical practice adapts and modernises accordingly and produces documentation that permits those who travel after joint arthroplasty in order to provide better patient care.
The aim of this study was to present the most commonly occurring difficulties found by patients at airport security checks and their remarks regarding joint replacement implant identification cards and if such documentation was wanted and/or led to more streamlined travel.
We conducted a cross-sectional observational study on the impact of replacement implants on patients travelling through airport security. This was performed on patients who presented to outpatient departments in February 2014.
Four airport security departments (London Stansted, London Gatwick, London Heathrow, and Amsterdam Schiphol International Airport) were approached from March 2015 to August 2015. This involved a formal discussion with airport security officers and completion of a questionnaire. After completion, procedures regarding airport security and joint replacement surgery were discussed and outlined.
A formal opinion was also sought from The Director of Aviation Security, a member of the Civil Aviation Authority's Executive Committee, responsible for the regulation and compliance of aviation security in the UK, for airports, airlines, cargo handlers, and in-flight suppliers.
A questionnaire was provided to patients in our department who had undergone lower limb joint replacement surgery, either total knee or total hip replacement (Appendix 1). Inclusion criteria was limited to those who had experienced airport security checks after surgery as a direct result of their lower limb arthroplasty and who could provide informed consent. Patients were excluded if they possessed other medical devices that also risked setting off airport security alarms such as diabetic infusion pumps.
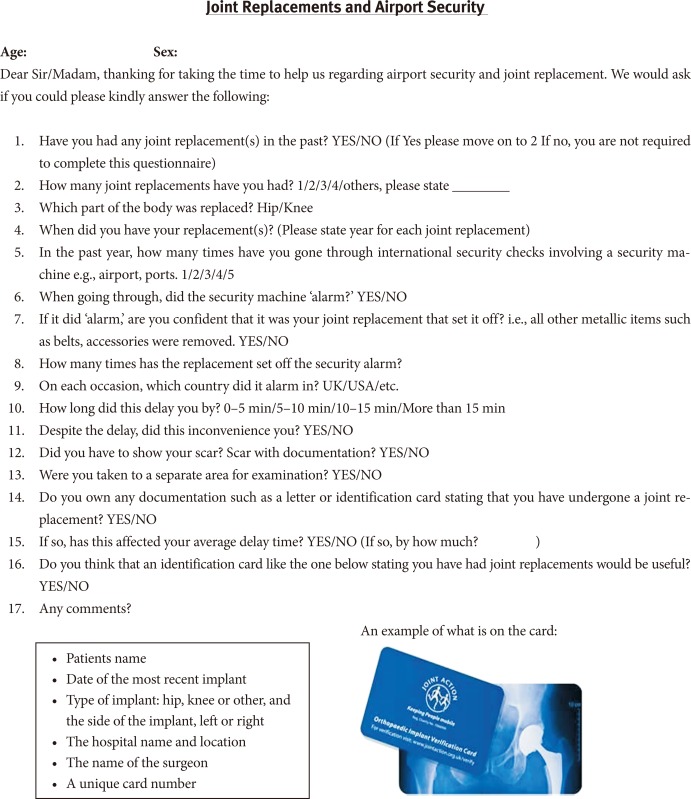
Patients were asked for demographic information (age and sex only) and questions specific to hip and knee replacement such as how many replacements they had had, when these had been performed and further closed questions were asked relevant to airport security checks and accredited hip and knee replacement documentation (Fig. 1).
Airport security officers were asked two questions: (1) Are you aware of implant identification cards? and (2) If so, are these information cards helpful in traveler security checks? They were then permitted to make any comments.
In order to assess the quality of the questionnaires, these were assessed by 6 independent lower limb arthroplasty consultants and 6 patients prior to dissemination in outpatient clinics. During clinical consultations, patients were asked if they were willing to participate in the study. If so, they were provided with a questionnaire and clarification was made that they fully comprehended the questions during the consultation. After completion, questionnaires were then collected by the nursing staff as patients departed from clinic and the data was then examined.
Due to the observational nature of this study and the fact that no patient identifiable data was utilised, Institutional Review Board approval was not required.
Responses were received from 10 airport security officers with 90% (9 out of 10) stating that these were useful to them at airport security. Presentation of these implant identification cards negated the need to take individuals to separate areas for strip search examination, which meant that airport staff did not need to be redirected elsewhere, replacement staff was not required, travelers were not delayed unnecessarily and airport security checking of passengers was more efficient.
We obtained questionnaires from 50 patients (mean age, 70.4 years; range, 55 to 84 years) presenting in lower limb arthroplasty clinics who met our selection criteria. Twenty-eight of these patients were female (mean age, 69.1 years; range, 55 to 84 years) and 22 were male (mean age, 71.2 years; range, 58 to 81 years).
Twenty-three patients presented post single primary arthroplasty surgery: 12 and 11 of these patients underwent total knee and total hip replacement surgery, respectively. Twenty-three patients presented after having 2 joint replacements: 3 patients had a single hip and knee replacement together, 9 patients had bilateral total hip arthroplasty and 11 patients had bilateral total knee replacement surgery. Two patients who completed the questionnaire had 3 joints replaced, with both patients having had bilateral hip and solitary knee replacement surgery. The other 2 patients underwent 4 joint replacements-bilateral hips and knees.
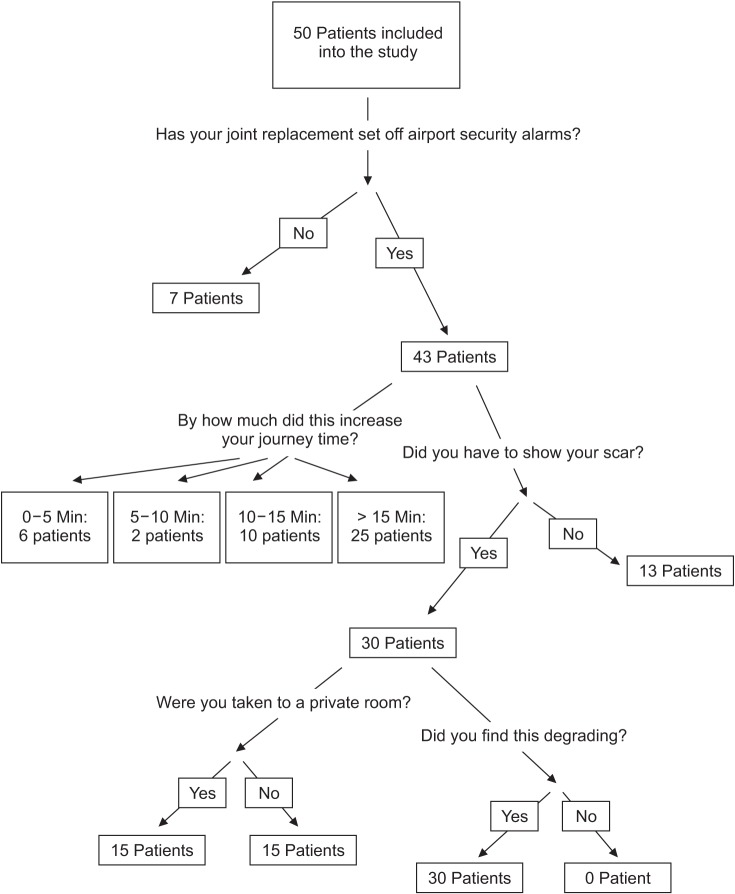
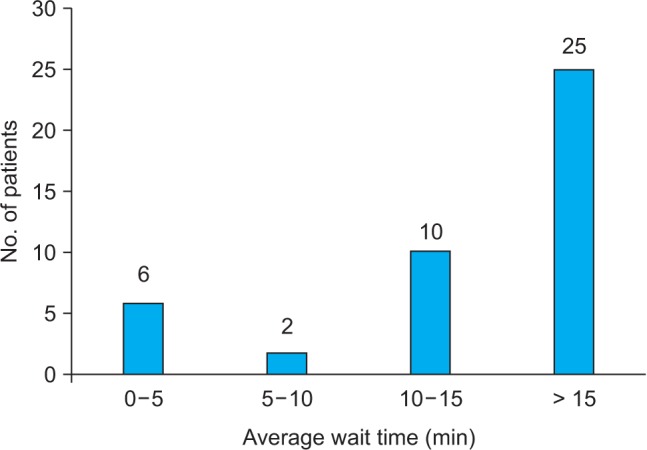
Of the 43 patients whose implants set off the airport security alarms, 6 stated the additional security checking delayed their time at airport security by 0–5 minutes, 2 by 5–10 minutes, 10 by 10–15 minutes and 25 by greater than 15 minutes (Fig. 2). Thirty-seven patients remarked that over time, this became a significant inconvenience to their travel: all of these patients were stopped on average for greater than 5 minutes. Of the 43 patients that set off the alarm system, 30 patients had to show their scar overlying the implant, 15 of these were taken to a private room for this purpose. All 30 patients stated, in addition to the yes/no responses on the questionnaire supplied, that they found this process degrading.
Of the 50 patients, 6 patients possessed an implant identification card. Of these, all 6 stated that after acquisition of an implant identification card they no longer needed to demonstrate their implant scar, which they had needed to before card acquisition, because airport security officers were satisfied on presentation of the card. They underwent a frisk search only and stated this was a much better experience, and they fully endorsed the card and recommended other patients who had undergone total joint arthroplasty to obtain one. These patients were delayed on average by 0–5 minutes after acquisition of the card and 10–15 minutes before they obtained a card.
Amongst the industry Operations Committee of the Civil Aviation Authority, the members recognised that passengers with orthopaedic implants felt reassured and more confident in going through airport security if they were in possession of more formal documentation, and that such an approach might have benefits over passengers carrying, for example, a letter from their surgeon.
Metal detection equipment creates an alternating electromagnetic field. Metallic implants are capable of undergoing temporary magnetism, as such, disturbances occur in the electromagnetic eddy currents generated from the source induced by the implant and subsequently detected by the receiver.5) Implant iron content and manufacturing processes determine magnetic conductivity. The composition of metal implants has varied with time in light of advances that are coupled with modernisation and the growing use of alloys.
There are two types of detectors employed at airport security gates. These are arch detectors and hand-held detectors. It is compulsory for all passengers to pass through arch detectors and if warranted, hand-held detectors will be used if a threshold level is reached by arch detection.
Metal detector detection settings and alarm settings are set by the Federal Aviation Authority (FAA) and have become more sensitive since the 9/11 attack in New York, USA. in light of increased security concerns. The variation between older and more modern arch and handheld detectors was demonstrated by Boivin et al.6) More sophisticated software programs can discriminate between different implant metal alloys and discussions with airport security staff have revealed that varying lengths of implant can also be determined.
Our study has attempted to consider a more efficient and ultimately customer-friendly process for facilitating the processing of passengers travelling with orthopaedic implants through airport security. The current method of individuals carrying nonstandardised and accredited implant authentication documents has improved security checking for both patients and security officers. It appears that a lack of consistency exists in the process of security checks on those with orthopaedic implants and this has resulted in uneven treatment of these passengers with varying requirements placed on them by security staff at different locations.
At present, no specific regulations covering the security screening of individuals with orthopaedic implants exist but the following standard advice is offered: The general advice would be that when passing through the walkthrough metal detectors, metallic implants will almost always alarm, leading to the passenger being hand searched by hand-held metal detectors. If passing through a security scanner, the implants will most likely show as an anomaly, leading to a targeted search. An enhanced, private hand search may be necessary if the officer is unable to satisfy him/herself that no prohibited articles are carried.
It was apparent from those involved in airport security that the benefits of implant identification cards stating whether passengers had undergone joint replacement were marked. The possession of such a card led to more streamlined, time-efficient security checks being made whilst ensuring safety was not compromised. The purpose of the identification card is not to stop the use of the hand-held devices nor to compromise safety with regards to security checks conducted at airport security but instead to stop the time-delaying private checking process where a greater history has to be taken and passengers are undressed in order to provide proof of a scar and previous surgery. Not only do these private checks lead to unnecessary use of manpower and time delays for security staff but are sources of significant anxiety and inconvenience to passengers. Recent airport security breaches have led to the tightening of airport security, which means that it is now more important than ever to ensure airport security staff are used optimally and efficiency is maximised.
Although some reports have stated that those who have undergone joint replacement are unlikely to encounter a major disruption when travelling through airline security,4) this goes against data collected from security staff at 4 international airports and patients involved in our study. It must be appreciated that the issues raised on airport security by joint replacement are much more commonplace and lead to time-consuming and unnecessary additional security checks. These difficulties were also revealed in the study performed in our unit.
It should be highlighted that with existing biometric data available on ePassports, further information pertaining to a patient's implant history could be entered onto the passports themselves, which would permit airport security staff to access the validated data at security checkpoints.
The British Orthopaedic Association in conjunction with The British Airport Authority had previously introduced the free orthocard, a personalised credit card sized card that was designed to inform that the individual possessing it had undergone joint replacement surgery. Six patients included in this study possessed this specific form of implant identification card and highly endorsed its use. Unfortunately, the project proved economically unviable and these cards are no longer issued and have been discontinued due to unsustainable costs.
The authors of this study recommend the use of a validated and accredited implant identification card which not only makes individuals' experience of airport security more favourable and efficient but also aids airport security staff in the ways mentioned in this article. Limitations do still exist in the use of implant identification cards as they are not universally accepted. In spite of being difficult to implement, we suggest the development of a universally recognised implant identification card that is accredited by the UK Civil Aviation Authority and the National Health Service be made in conjunction with Orthopaedic Surgeons in order to improve patients' postoperative experience of joint arthroplasty.
Further potential also exists. The introduction of biometrically chipped ePassports has brought with it the potential to install a patient's medical information, such as a total joint arthroplasty, upon the passport, which would negate the need to produce further accredited and validated documentation. This would later permit a patient's medical history to be updated when necessary in order to reflect a more accurate and recent medical history and used by security staff at their discretion. The patient would be at liberty to enter medical history they see fit and relevant for airport travel.
The authors of this study believe that whilst we are not advocating that airport security staff does not need to ensure they are fully satisfied prior to permitting travelers to pass through security, notification of these staff of patients with orthopaedic implants requires a more modern solution. Stopping these patients at airport security for examinations is likely to become more commonplace considering an increased frequency of joint replacement surgery is performed and heightened security measures and checks are introduced. Whilst it is encouraging that The Operations Committee of the Civil Aviation Authority was of the opinion that moving forward with a potential proposal to somehow improve patient experience at airport security would not meet any resistance in principle either from industry or from the regulator, we must ensure that expectations are managed.
References
1. Obremskey WT, Austin T, Crosby C, et al. Detection of orthopaedic implants by airport metal detectors. J Orthop Trauma. 2007; 21(2):129–132. PMID: 17304069.

2. Pearson WG, Matthews LS. Airport detection of modern orthopedic implant metals. Clin Orthop Relat Res. 1992; (280):261–262.

3. Lee AJ, Jacobson SH. Identifying changing aviation threat environments within an adaptive Homeland Security Advisory System. Risk Anal. 2012; 32(2):319–329. PMID: 21801188.

4. Abbassian A, Datla B, Brooks RA. Detection of orthopaedic implants by airport metal detectors. Ann R Coll Surg Engl. 2007; 89(3):285–287. PMID: 17394716.

5. Beaupre GS. Airport detection of modern orthopedic implant metals. Clin Orthop Relat Res. 1994; (303):291–292.
6. Boivin W, Coletta J, Kerr L. Characterization of the magnetic fields around walk-through and hand-held metal detectors. Health Phys. 2003; 84(5):582–593. PMID: 12747477.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download