Abstract
Background
The purpose of this review was to assess the risk of infection-related complications following cemented and cementless hemiarthroplasty in elderly patients.
Methods
We searched PubMed, EMBASE, and Cochrane Library databases for published randomized clinical trials comparing cemented hemiarthroplasty with cementless hemiarthroplasty in patients with a femoral neck fracture and more than 65 years of age. Eight randomized controlled trials were available for analysis. A meta-analysis (with a fixed-effects model) and a meta-regression analysis (with continuous variables) were performed.
Results
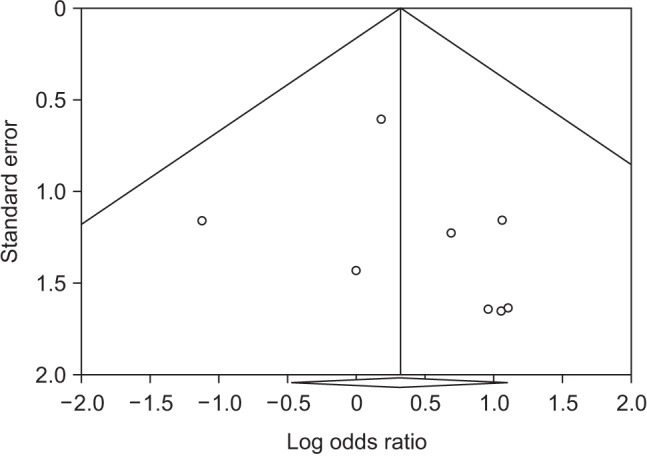
The 8 trials included 1,204 hips (608 cemented and 596 cementless). There was no significant difference between the cemented and cementless groups regarding the incidence of deep infection, superficial infection, pneumonia, and urinary tract infection. The overall incidence of postoperative deep infection was 2.3% (14/608) in the cemented group and 1.2% (7/596) in the cementless group (relative risk, 1.74; 95% confidence interval, 0.74 to 4.14; I2 = 0%; p = 0.206). No publication bias was found in the funnel plot.
Hemiarthroplasty is now the treatment of choice for displaced fractures of the femoral neck in elderly patients.12) Hemiarthroplasty can be performed in two different ways: fixation with bone cement or press-fit without cement.
Early rehabilitation can be achieved with less pain after cement fixation by providing an immediate strong interlock between the prosthesis and the periprosthetic bone tissue.3) Cement fixation can decrease postoperative complications related to late mobilization, such as pneumonia or urinary tract infection (UTI), compared to cementless fixation.4) However, cementless fixation is associated with a shorter operation time and less intraoperative blood loss.5)
Until recently, five systematic reviews and meta-analyses comparing cemented hemiarthroplasty and cementless hemiarthroplasty have been published.678910) Most studies have evaluated mortality, postoperative pain, function, and general medical complication rates. However, no previously published meta-analysis has focused on infection-related complications.
The purpose of the current study was to assess the risk of postoperative complications related to infection after hemiarthroplasty in elderly patients. Therefore, we reviewed all up-to-date randomized clinical trials that reported on the followings: (1) postoperative deep infection; (2) postoperative superficial infection; (3) pulmonary infection; and (4) UTI.
Two reviewers (BHY, JGS) independently searched PubMed, EMBASE, and Cochrane Library databases for eligible trials from September 3, 2016. The following search terms were used in the PubMed database: (hip [Medical Subject Heading term, MeSH] OR hip [all fields] OR hip joint [MeSH term]) AND (arthroplasty [MeSH term] OR arthroplasty [all fields]) AND (bone cements [MeSH term] OR bone cement [all fields] OR cemented [all fields]) AND (cementless [all fields] OR uncemented [all fields]) AND English [language]. In the other databases, the following keywords were used: hip, replacement, arthroplasty, bone cement, and cementless or uncemented. The identified studies were then filtered to limit the search to publications from 1980 to 2016.
Bibliographies of the selected articles were also reviewed manually to identify any articles not found in the primary search. Two observers (BHY, JGS) reviewed the titles and abstracts of the identified articles. If both observers agreed that a study did not meet the eligibility criteria, it was excluded.
Inclusion criteria were (1) randomized controlled studies on cemented and cementless hemiarthroplasty in patients with a femoral neck fracture and more than 65 years of age; and (2) articles reporting at least one of the following main clinical outcomes: the rate of superficial wound infection, deep infection, or general perioperative complications related to infection.
Exclusion criteria were (1) articles that included revision cases; (2) articles that used national registry data; (3) articles that reported no infection in both cemented and cementless groups; (4) articles that grouped reports of outcomes without distinguishing cases with complications in detail; and (5) reviews and basic science articles.
Data, including the year of publication, study design, number of hips treated with hemiarthroplasty, type of implant used, technique of cement use, status of antibiotic loading in bone cement, mean length of follow-up, number of hips lost to follow-up, and time when infection occurred, were extracted and entered into a spreadsheet.
The primary outcome was the rate of deep infection in patients who underwent hemiarthroplasty. Secondary outcomes were postoperative complications recorded as follows: (1) superficial wound infection treated with antibiotics only without surgery; (2) pneumonia; and (3) UTI.
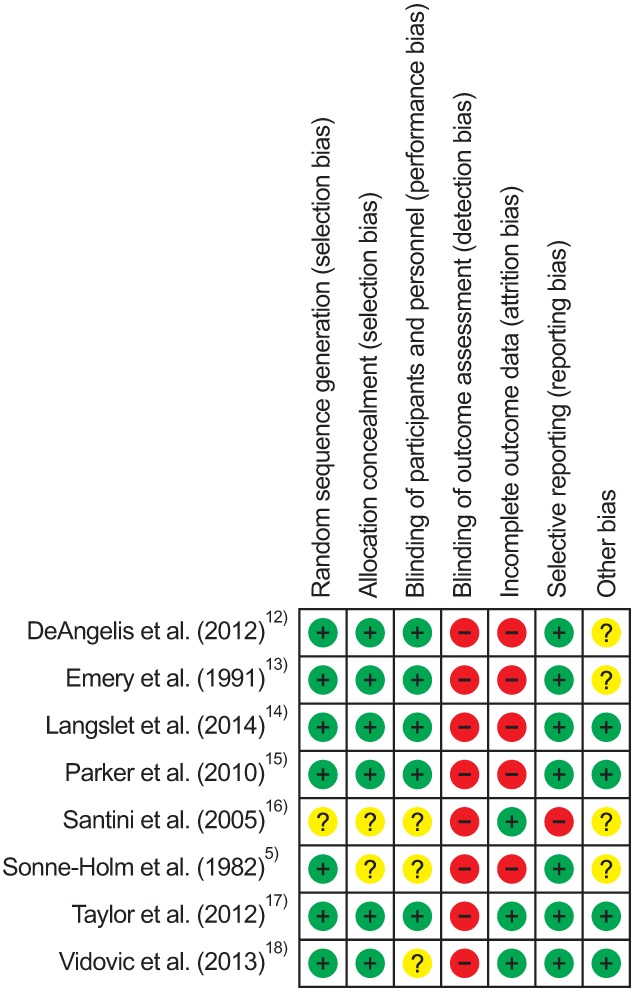
Reviewers (BHY, JGS) independently evaluated the methodological quality of the included trials using a specific tool for assessing the risk of bias recommended by the Cochrane Collaboration. This comprises a description and a judgment for each entry in a risk of bias table, in which each entry addresses a specific feature of the study. The judgment for each entry involves answering a question with one of the following responses: yes, indicating a low risk of bias; no, indicating a high risk of bias; and unclear, indicating either a lack of information or uncertainty over the potential for bias.11)
For each study, we calculated the relative risks with 95% confidence intervals by using crude 2 × 2 tables on the basis of intention to treat analysis, whenever possible, from the original publications.11) To test heterogeneity, we used Higgins I2 statistics. Significant heterogeneity was not observed in these studies (p = 0.957); therefore, we reported data from a fixed-effects model. We also performed meta-regression analysis to evaluate the association between the study's results and continuous variables. We assessed publication bias using Begg's funnel plot and Egger's test. If publication bias exists, the Begg's funnel plot is asymmetric or the Egger's test p-value is < 0.05. The meta-analysis was performed using Comprehensive Meta-analysis software ver. 3.3 (Biostat, Englewood, NJ, USA).
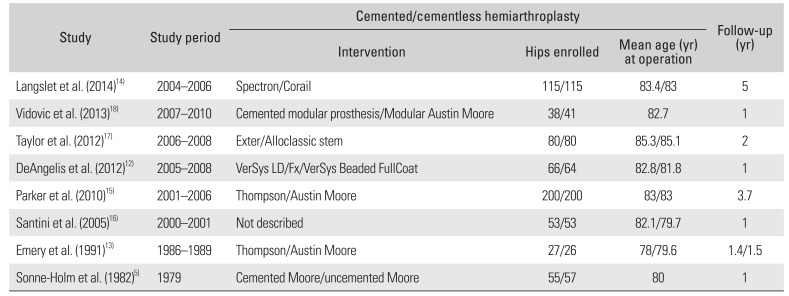
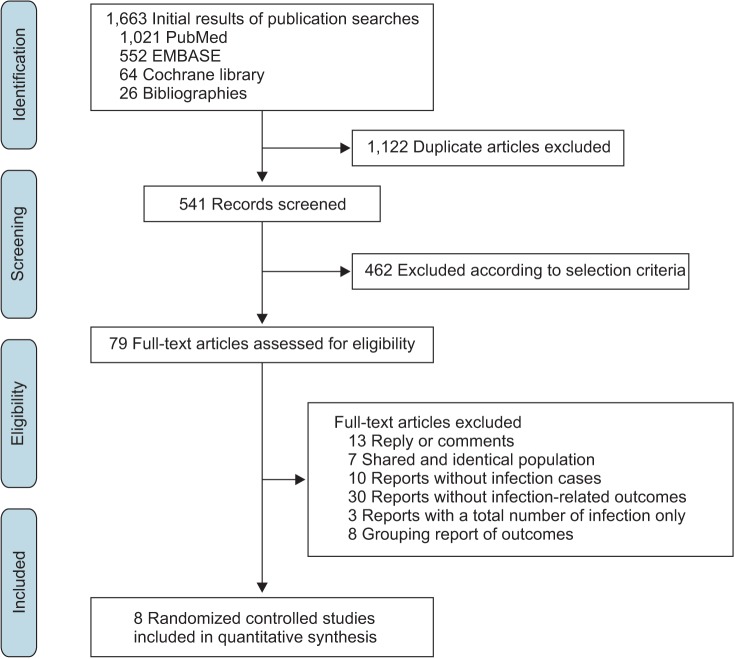
Based on the aforementioned search criteria, 8 randomized controlled trials were available for the final analysis. 512131415161718) The process from the initial publication searches to the final selection of clinical trials is displayed in a flowchart (Fig. 1). There were 1,204 hips included in the 8 studies: 608 hips in the cemented group and 596 in the cementless group. The study design, types of implants used, and included data extracted from each of the analyzed studies are summarized in Table 1.
The overall incidence of postoperative deep infection was 2.3% (14/608) in the cemented group and 1.2% (7/596) in the cementless group. The overall superficial wound infection incidence was 1.5% (9/608) in the cemented group and 1.7% (10/596) in the cementless group. The incidence of pneumonia and UTI were 3.6% (21/608) and 1.8% (11/608) in the cemented group, and 5.0% (30/596) and 2.2% (13/596) in the cementless group, respectively.
In the fixed-effects meta-analysis of all 8 trials, the use of cement was not associated with an increased risk of postoperative deep infection (relative risk, 1.74; 95% confidence interval, 0.74 to 4.14; I2 = 0%; p = 0.206) (Fig. 2). When the other infection-related outcomes were analyzed, no significant differences between cemented and cementless hemiarthroplasty were found (Fig. 3). We found no significant association between the odds ratio (OR) and the difference in operation time between two groups, year of publication, and duration of follow-up (Table 2).
Infection-related complications remain a potentially devastating complication, resulting in major morbidity for the patient, which adversely affects the outcome of arthroplasty. 19) Despite surgeons' best efforts, deep infection, in particular, can ultimately lead to a dysfunctional or disfiguring result.20)
Our meta-analysis showed no significant difference in the OR of postoperative deep infection between cemented and cementless hemiarthroplasty. The longer operating time for cemented hemiarthroplasty can be a risk factor for an increased incidence of infection.21) In the included studies of our analysis, the operation time was on average 11 minutes longer for cemented hemiarthroplasty than for cementless hemiarthroplasty.12131415161718) We additionally have performed meta-regression analysis on the OR and the difference in operation time between two groups, but no significant difference was found (Table 2).
It is interesting to compare this with our previous report in patients with primary total hip arthroplasty (THA).22) The previous review revealed that the use of cement in THA was associated with an increased risk of deep infection (OR, 1.53). In contrast, this analysis noted the risk of deep infection (OR, 1.74) in the cemented group showed no significant difference. The surgery time of hemiarthroplasty is usually much shorter than that of total hip arthroplasty.23) The surgery time of hemiarthroplasty takes only within 1 hour, it could not make a significant difference.24) Also, the cumulative sample size was not enough to demonstrate the significant difference although meta-analysis was performed. Similar postoperative deep infection rates after hemiarthroplasty between two groups were also observed from national registry studies (Table 3).252627)
Antibiotic-loaded bone cement and perioperative antibiotics have been shown to protect against infection in earlier studies.28) Additionally, perioperative transfusion of leukocyte-containing allogeneic blood components is an apparent risk factor for the development of postoperative bacterial infections.29) We attempted to perform subgroup analysis for cemented hemiarthroplasty, perioperative antibiotics, and blood transfusion. However, the use of perioperative antibiotic or antibiotic-loaded bone cement was described in only 4 studies,12141518) and blood transfusion was described in another 4 studies.5121516) Thus, we could not perform subgroup analysis in terms of antibiotics or blood transfusion.
Bone cement forms a solid bond between the stem and bone, providing favorable biomechanical advantages. This advantage can reduce the degree of early postoperative pain and lead to better mobility and early mobilization. Thus, we expected lower postoperative complication rates such as pneumonia by early ambulation or UTI via the early removal of an indwelling urinary catheter.4) There was no significant difference; however, the overall incidences of pneumonia and UTI were slightly lower in the cemented group than in the cementless group.
Cementless fixation is preferred in patients with a high risk of perioperative mortality.30) Serious intraoperative complications, including intraoperative death and cardiac arrest, were almost exclusively reported for the cemented procedures.25) In randomized studies, the suitability of each patient who received a cemented component was assessed by the anesthetist in charge, and patients whose risk of mortality was deemed unacceptable were excluded from the study.17)
The present study has some limitations. First, the cumulative sample size was not very large because most of the trials included relatively few hips. However, we additionally performed sample size calculation based on an OR (1.53) to estimate the required sample size: a total of 806 patients would be sufficient to detect difference with a power of 0.80 and a two-tailed alpha of less than 0.05. The number of subjects included in our study (1,204) was enough to detect difference. Second, potential sources of bias in these trials included a lack of blinding to the type of surgical treatment by the outcome assessors, an increased loss to follow-up, and postrandomization exclusion of study participants from analyses in several trials.
There is still debate about the choice between using cemented and cementless hemiarthroplasty for treating femoral neck fractures in elderly patients. In our meta-analysis, there were no significant differences in the postoperative complication rates between cemented and cementless hemiarthroplasty. Our meta-analysis suggests that when selecting a fixation method for hemiarthroplasty, infection-related postoperative complications are not a determinant factor to consider. Thus, the choice of implant for hemiarthroplasty can be made based on other factors such as the patient's comorbidities or the surgeon's preference.
ACKNOWLEDGEMENTS
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (No. HC15C1189).
References
1. Bhandari M, Devereaux PJ, Tornetta P 3rd, et al. Operative management of displaced femoral neck fractures in elderly patients: an international survey. J Bone Joint Surg Am. 2005; 87(9):2122–2130. PMID: 16140828.
2. Gjertsen JE, Vinje T, Engesaeter LB, et al. Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. J Bone Joint Surg Am. 2010; 92(3):619–628. PMID: 20194320.

3. Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2010; (6):CD001706. PMID: 20556753.

4. Husted H, Otte KS, Kristensen BB, Orsnes T, Wong C, Kehlet H. Low risk of thromboembolic complications after fast-track hip and knee arthroplasty. Acta Orthop. 2010; 81(5):599–605. PMID: 20919815.

5. Sonne-Holm S, Walter S, Jensen JS. Moore hemi-arthroplasty with and without bone cement in femoral neck fractures: a clinical controlled trial. Acta Orthop Scand. 1982; 53(6):953–956. PMID: 6758474.
6. Luo X, He S, Li Z, Huang D. Systematic review of cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures in older patients. Arch Orthop Trauma Surg. 2012; 132(4):455–463. PMID: 22160512.

7. Ahn J, Man LX, Park S, Sodl JF, Esterhai JL. Systematic review of cemented and uncemented hemiarthroplasty outcomes for femoral neck fractures. Clin Orthop Relat Res. 2008; 466(10):2513–2518. PMID: 18651200.

8. Li T, Zhuang Q, Weng X, Zhou L, Bian Y. Cemented versus uncemented hemiarthroplasty for femoral neck fractures in elderly patients: a meta-analysis. PLoS One. 2013; 8(7):e68903. PMID: 23935902.

9. Azegami S, Gurusamy KS, Parker MJ. Cemented versus uncemented hemiarthroplasty for hip fractures: a systematic review of randomised controlled trials. Hip Int. 2011; 21(5):509–517. PMID: 21948035.

10. Ning GZ, Li YL, Wu Q, Feng SQ, Li Y, Wu QL. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: an updated meta-analysis. Eur J Orthop Surg Traumatol. 2014; 24(1):7–14. PMID: 23412274.

11. Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. Chichester, UK: Wiley;2008.
12. Deangelis JP, Ademi A, Staff I, Lewis CG. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a prospective randomized trial with early follow-up. J Orthop Trauma. 2012; 26(3):135–140. PMID: 22198652.
13. Emery RJ, Broughton NS, Desai K, Bulstrode CJ, Thomas TL. Bipolar hemiarthroplasty for subcapital fracture of the femoral neck: a prospective randomised trial of cemented Thompson and uncemented Moore stems. J Bone Joint Surg Br. 1991; 73(2):322–324. PMID: 2005165.

14. Langslet E, Frihagen F, Opland V, Madsen JE, Nordsletten L, Figved W. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin Orthop Relat Res. 2014; 472(4):1291–1299. PMID: 24081667.

15. Parker MI, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures: a randomised controlled trial in 400 patients. J Bone Joint Surg Br. 2010; 92(1):116–122. PMID: 20044689.
16. Santini S, Rebeccato A, Bolgan I, Turi G. Hip fractures in elderly patients treated with bipolar hemiarthroplasty: comparison between cemented and cementless implants. J Orthop Traumatol. 2005; 6(2):80–87.

17. Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am. 2012; 94(7):577–583. PMID: 22488613.

18. Vidovic D, Matejcic A, Punda M, et al. Periprosthetic bone loss following hemiarthroplasty: a comparison between cemented and cementless hip prosthesis. Injury. 2013; 44(Suppl 3):S62–S66. PMID: 24060022.

19. Wijeratna MD, McRoberts J, Porteous MJ. Cost of infection after surgery for intracapsular fracture of the femoral neck. Ann R Coll Surg Engl. 2015; 97(4):283–286. PMID: 26263936.

20. Cahill JL, Shadbolt B, Scarvell JM, Smith PN. Quality of life after infection in total joint replacement. J Orthop Surg (Hong Kong). 2008; 16(1):58–65. PMID: 18453662.

21. Abdulkarim A, Ellanti P, Motterlini N, Fahey T, O'Byrne JM. Cemented versus uncemented fixation in total hip replacement: a systematic review and meta-analysis of randomized controlled trials. Orthop Rev (Pavia). 2013; 5(1):e8. PMID: 23705066.

22. Yoon BH, Ha YC, Lee YK, Koo KH. Postoperative deep infection after cemented versus cementless total hip arthroplasty: a meta-analysis. J Arthroplasty. 2015; 30(10):1823–1827. PMID: 26021907.

23. Wang F, Zhang H, Zhang Z, Ma C, Feng X. Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis. BMC Musculoskelet Disord. 2015; 16:229. PMID: 26316274.

24. Namba RS, Inacio MC, Paxton EW. Risk factors associated with surgical site infection in 30,491 primary total hip replacements. J Bone Joint Surg Br. 2012; 94(10):1330–1338. PMID: 23015556.

25. Gjertsen JE, Lie SA, Vinje T, et al. More re-operations after uncemented than cemented hemiarthroplasty used in the treatment of displaced fractures of the femoral neck: an observational study of 11,116 hemiarthroplasties from a national register. J Bone Joint Surg Br. 2012; 94(8):1113–1119. PMID: 22844055.
26. Jameson SS, Jensen CD, Elson DW, et al. Cemented versus cementless hemiarthroplasty for intracapsular neck of femur fracture: a comparison of 60,848 matched patients using national data. Injury. 2013; 44(6):730–734. PMID: 23206920.
27. Yli-Kyyny T, Sund R, Heinanen M, Venesmaa P, Kroger H. Cemented or uncemented hemiarthroplasty for the treatment of femoral neck fractures? Acta Orthop. 2014; 85(1):49–53. PMID: 24397746.

28. Hill C, Flamant R, Mazas F, Evrard J. Prophylactic cefazolin versus placebo in total hip replacement: report of a multicentre double-blind randomised trial. Lancet. 1981; 1(8224):795–796. PMID: 6111670.

29. Vamvakas EC, Carven JH. Transfusion of white-cell containing allogeneic blood components and postoperative wound infection: effect of confounding factors. Transfus Med. 1998; 8(1):29–36. PMID: 9569457.
30. Talsnes O, Vinje T, Gjertsen JE, et al. Perioperative mortality in hip fracture patients treated with cemented and uncemented hemiprosthesis: a register study of 11,210 patients. Int Orthop. 2013; 37(6):1135–1140. PMID: 23508867.

Fig. 2
Forest plot of the odds ratios with confidence intervals for deep infection. Two of the 8 studies reporting no cases of deep infection were excluded in this analysis. CI: confidence interval.
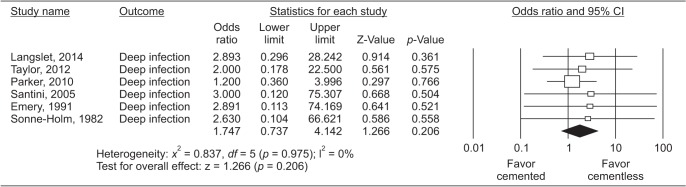
Fig. 3
Forest plot of the odds ratios with confidence intervals (CIs) for postoperative infection-related complications. (A) Superficial wound infection. (B) Pneumonia. (C) Urinary tract infection.
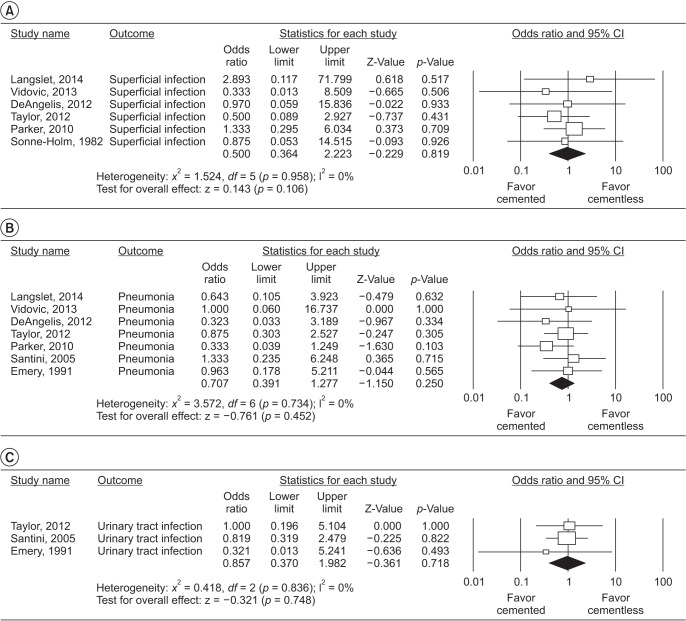
Table 1
Characteristics of Included Individual Studies
| Study | Study period | Cemented/cementless hemiarthroplasty | Follow-up (yr) | ||
|---|---|---|---|---|---|
| Intervention | Hips enrolled | Mean age (yr) at operation | |||
| Langslet et al. (2014)14) | 2004–2006 | Spectron/Corail | 115/115 | 83.4/83 | 5 |
| Vidovic et al. (2013)18) | 2007–2010 | Cemented modular prosthesis/Modular Austin Moore | 38/41 | 82.7 | 1 |
| Taylor et al. (2012)17) | 2006–2008 | Exter/Alloclassic stem | 80/80 | 85.3/85.1 | 2 |
| DeAngelis et al. (2012)12) | 2005–2008 | VerSys LD/Fx/VerSys Beaded FullCoat | 66/64 | 82.8/81.8 | 1 |
| Parker et al. (2010)15) | 2001–2006 | Thompson/Austin Moore | 200/200 | 83/83 | 3.7 |
| Santini et al. (2005)16) | 2000–2001 | Not described | 53/53 | 82.1/79.7 | 1 |
| Emery et al. (1991)13) | 1986–1989 | Thompson/Austin Moore | 27/26 | 78/79.6 | 1.4/1.5 |
| Sonne-Holm et al. (1982)5) | 1979 | Cemented Moore/uncemented Moore | 55/57 | 80 | 1 |
Table 2
Trends by Meta-Regression Analysis between Continuous Variables and Odds Ratio for Postoperative Deep Infection after Hemiarthroplasty
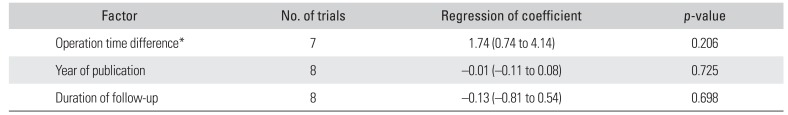
Table 3
Postoperative Infection-Related Complication Rates According to Fixation Method in Several Reports from National Registry Data
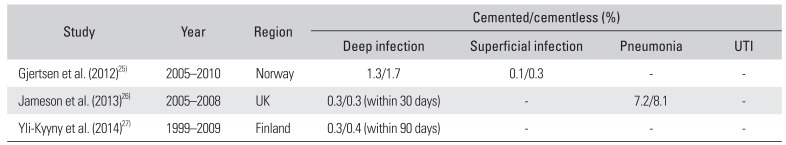
| Study | Year | Region | Cemented/cementless (%) | |||
|---|---|---|---|---|---|---|
| Deep infection | Superficial infection | Pneumonia | UTI | |||
| Gjertsen et al. (2012)25) | 2005–2010 | Norway | 1.3/1.7 | 0.1/0.3 | - | - |
| Jameson et al. (2013)26) | 2005–2008 | UK | 0.3/0.3 (within 30 days) | - | 7.2/8.1 | - |
| Yli-Kyyny et al. (2014)27) | 1999–2009 | Finland | 0.3/0.4 (within 90 days) | - | - | - |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download