Abstract
Hip dysplasia is the most common cause of secondary osteoarthritis (OA). To prevent the early onset of secondary OA, Nishio's transposition osteotomy, Steel's triple osteotomy, Eppright's dial osteotomy, Wagner's spherical acetabular osteotomy, Tagawa's rotational acetabular osteotomy (RAO), and Ganz' periacetabular osteotomy (PAO) have been proposed. PAO and RAO are now commonly used in surgical treatment of symptomatic acetabular dysplasia in Europe, North America, and Asia. The aim of this paper is to present the followings: the patient selection criteria for RAO; the surgical technique of RAO; the long-term outcome of RAO; and the future perspectives.
Hip dysplasia is the most common cause of secondary osteoarthritis (OA).12) Murphy et al.3) noted that no patient with a well-functioning hip until the age of 65 years had had the following characteristics: a center-edge angle of less than 16°, an acetabular index of depth to width of less than 38%, an acetabular index of the weight bearing zone of more than 15°, uncovering of the femoral head of more than 31%, or an acetabulum in which the most proximal point of the dome had been at the lateral edge (zero peak-to-edge distance). A variety of techniques have been proposed to prevent the early onset of secondary OA including Nishio's transposition osteotomy,4) Steel's triple osteotomy,5) Eppright's dial osteotomy,6) Wagner's spherical acetabular osteotomy,7) Tagawa's rotational acetabular osteotomy (RAO),8) and Ganz' periacetabular osteotomy (PAO).9)
PAO and RAO are now commonly used in surgical treatment of symptomatic acetabular dysplasia in Europe, North America, and Asia. These procedures reorient the acetabulum to reduce superolateral acetabular inclination, improve femoral head coverage, translate the joint center medially, and normalize loading of the anterolateral acetabular rim.810)
The aim of this paper is to present the followings: the patient selection criteria for RAO, the surgical technique of RAO, the long-term outcome of RAO, and the future perspectives.
The primary indications for RAO include pain lasting for more than 6 months, adequate range of motion, radiographic evidence of residual hip dysplasia, and closure of the triradiate cartilage, which are identical to those for PAO.1112) In a number of studies, abduction and internal rotation radiographs were used to determine if the femoral head would roll into the acetabulum and obtain the expected congruity after surgery (Fig. 1A and B). The preoperative maximum lateral center-edge angle was 10° to 20°.1112) The mean age at the time of surgery was 27 to 53 years.12)
There are some controversies on the patient selection criteria for PAO or RAO with regard to the advanced stage or age at the time of surgery. Trousdale et al.13) reported on 42 patients who underwent PAO. Among the patients with a Tonnis grade 1, 2, or 3, the results were best in those with grade 1 involvement and poor in those with grade 2 or 3 for a mean follow-up of 4 years. Nakamura et al.14) reported the long-term results of RAO in 131 patients (145 hips) who had been followed for a mean of 13 years. A Merle d'Aubigne score of greater than 15 points was obtained in 90 of the 112 hips (80%) with prearthritic or early-stage arthritis but in only nine of the 33 hips with advanced-stage or end-stage arthritis. Siebenrock et al.15) suggested the factors that mitigate against a good clinical score of Merle d'Aubigne score > 15 points) and prevention of OA progression after a PAO were advanced stage and older age at the time of surgery. Recent studies reported that properly selected patients with advanced-stage OA could have a good clinical score (> 80 points of Harris hip score or > 15 points of Merle d'Aubigne score) after RAO.1617) Yasunaga et al.16) proposed the essential criteria for advanced-stage OA patients were a good postoperative joint congruency (Fig. 2) expected and a preoperative minimum joint space width of > 2.2 mm. Hasegawa et al.17) also noticed a preoperative joint space of > 2 mm was essential for cases with advanced-stage OA.
RAO is performed fundamentally according to the technique of Ninomiya and Tagawa,8) apart from cutting the outer cortical bone of the ilium and ischium using an air drill and fixation of the rotated acetabulum.
The patient is placed in the exact lateral decubitus position with the extremity draped free on the table. No traction table or any other distraction device is used. Intraoperative fluoroscopy is used to confirm the appropriate osteotomy line, femoral coverage, and joint congruency.
The anterior approach is done between the tensor fascia lata and the sartorius. First, the lateral femoral cutaneous nerve should be detected and preserved. Then, the rectus femoris is exposed and cut (Fig. 3C). Anterior part of the gluteal medius is divided subperiosteally from the iliac wing.
The iliacus muscle is divided anteriorly and the bursa of ilio-psoas tendon is exposed. The bursa is cut, the ilio-psoas tendon is retracted anteriorly, and the ilio-pubic eminence is exposed. This is the osteotomy site of the pubic bone (Fig. 3D).
The external rotators muscles are divided and the posterior wall of acetabulum is exposed subperiosteally. Hohmann retractors are placed at the greater sciatic notch and the lesser sciatic notch (Fig. 3E). Under the gluteus medius, the iliac bone is exposed subperiosteally.
Before osteotomy, the articular cartilage is evaluated with arthroscopy. The arthroscope is inserted at the anterior capsule with leg traction by an assistant.
At the anterior part, after the joint space is detected, the osteotomy line is decided. The osteotomy line is one fingerbreadth above the joint space. At the posterior site, the osteotomy line is almost horizontal at the level of the base of the ischium. At the greater sciatic notch, the osteotomy line is mid-part between the joint space and the greater notch (Fig. 3E). Bone graft is taken from the external wall of the iliac wing.
Before the osteotomy, using an air drill, the outer cortical bone of the ilium and ischium is cut (Fig. 3F and G). With this technique, the cancellous bone can be cut smoothly with a curved osteotome and the inner cortical bone of the ilium can be cut precisely.
The pubic bone is cut at the iliopubic eminence. The anterior ilium bone is cut with a curved osteotome. The sound of hammer permits detection when the tip of the osteotome reaches the inner cortical bone and excessive penetration into the intrapelvic space can be avoided (Fig. 3H and I).
Hooking over the osteotomy site of the pubic bone, an assistant positions the patient's hip in abduction-external rotation. Then, the acetabulum is rotated in an anterolateral direction (Fig. 3J). In order to move the femoral head medially, the intrapelvic portion of the free acetabulum should be thinned and excess bone should also be removed from the pelvic side.
The rotation provides a more horizontal weight-bearing area while maintaining the contact between the osteotomy sites in the pubic and ischium and returning the superiorly subluxated femoral head to a more normal position.
One or two trapezoidal bone grafts are taken from the external wall of the iliac wing and used to fill the space between the ilium and the rotated acetabulum. The acetabulum is fixed with a Kirschrer wire temporarily.
Postoperative traction or cast immobilization is not used. After one day of bed rest, the patient is allowed to use a wheelchair, and non-weight-bearing walking is allowed as tolerated. Partial weight-bearing is begun 3 to 5 weeks after surgery depending on articular degeneration. Full weight-bearing is started 4–6 months after surgery, following the disappearance of the Trendelenburg sign.
Penetration of the osteotome into the joint should be avoided absolutely because it might cause progression of OA or osteonecrosis of the rotated acetabulum. The level of the osteotomy at the anterior ilium is very important. Until the experience is acquired, the level of the osteotomy at the anterior ilium should be confirmed under fluoroscopy.
Direct insertion of the osteotome into the ilium might cause fracture of the ilium, especially in the case of advanced-stage OA. Our technique of cutting the outer cortical bone of the ilium and ischium with an air drill before the osteotomy is valuable for preventing fractures.
Kaneuji et al.21) reported a long-term outcome of rotational acetabular osteotomy after a minimum of 20 years. In their report, the mean Harris hip score improved from preoperative points of 77 to final points of 90 in 23 hips with pre-OA and from 75 to 85 in 29 hips with early-stage OA. Hasegawa et al.22) also reported a follow-up study of eccentric rotational acetabular osteotomy with a mean duration of 20 years. Although their report included 18 hips with pre-OA, 49 hips with early-stage OA, 40 hips with advanced-stage OA, and 23 hips with simultaneous intertrochanteric valgus osteotomy, the mean preoperative Harris hip score of 70 points improved to a mean of 88 points. Thirty hips had a fair clinical outcome (Harris hip score < 80 points). In both reports, patients with pre-OA showed better clinical sores than patients with early-stage or advanced-stage OA.
We reported a follow-up study of rotational acetabular osteotomy with a mean duration of 20 years.23) Twenty-one patients with pre-OA (27 hips) and 110 patients with early-stage OA (118 hips) were available at a minimum of 15 years. Of the total 131 patients (145 hips), the mean age at the time of surgery was 22 years in the pre-OA group and 38 years in the early-stage group. The mean follow-up was 21 years in the pre-OA group and 20 years in the early-stage group. The mean Merle d'Aubigne and Postel score improved from 15 to 18 points in the pre-OA group and from 15 to 16 points in the early-stage OA group, mainly because of increased scores for pain. A total of 14 patients (15 hips) experienced worsening of their score from a mean of 14.5 to 12.0. Of these patients, the preoperative radiographic stage was pre-OA in only 1 patient (1 hip). In these patients, 8 patients (9 hips) with early-stage OA had total hip arthroplasties (THAs). Our clinical findings thus corroborate those of previous reports.
Kaneuji et al.21) reported 6 of 23 hips (26%) with pre-OA and 10 of 29 hips (34%) with early-stage OA showed radiographic OA progression; and 3 hips in each group were converted to THA. Hasegawa et al.22) reported 6 of 18 hips (33%) with pre-OA and 6 of 49 (12%) hips with early-stage OA showed radiographic OA progression, and the survival rate with conversion to THA as the endpoint was 97% at 20 years. In our study,23) 2 of 27 hips (7.4%) with pre-OA and 24 of 118 hips (20%) with early-stage OA showed OA progression. The survivorship analysis, with radiographic signs of progression of OA as the endpoint, predicted a survival rate of 82% at 20 years and, with conversion to THA as the endpoint, predicted a rate of 94% at 20 years in all cases.
We found two factors associated with radiographic OA progression: age at the time of surgery (older than 46 years) and postoperative joint congruency (fair). Hasegawa et al.22) described 4 factors leading to a poor outcome: a small (< 2 mm) preoperative minimum joint space, joint congruency, simultaneous intertrochanteric valgus osteotomy, and lateral subluxation of the femoral head postoperatively. Regarding joint congruency, several authors emphasized that postoperative good joint congruency is essential for a favorable outcome after PAO and RAO.212425) Patients with previous surgery or who need simultaneous femoral osteotomy are at risk of unfavorable postoperative joint congruency, and favorable long-term results cannot be expected.
In our study,23) there were 24 patients (24 hips) whose age of older than 65 years at the final follow-up and radiographic OA progression was prevented in 14 patients (58%). This result suggests that rotational acetabular osteotomy can change the natural history of the dysplastic hip according to the report by Murphy et al.3)
The key challenges are (1) preoperative evaluation of articular cartilage; (2) indication for older patients; (3) intraarticular treatment combined with PAO or RAO. According to Millis and his associates,2627) the success of PAO depends on articular cartilage that is sufficiently healthy to sustain normal load transmission. Shimogaki et al.28) also reported RAO caused considerable changes in joint morphology and histological changes in the articular cartilage, particularly in the medial part of the acetabulum. Yasunaga et al.29) found that even when postoperative joint congruency was classified as good in their criteria, there was the possibility of OA progression if the intraoperative arthroscopic evaluation is Outerbridge grade 4. Magnetic resonance imaging (MRI) can better assess the health of cartilage before surgery and predict which joints will still be painful postoperatively than plain radiographs.30) Delayed gadolinium-enhanced MRI,30) magnetic resonance arthrography,31) or T2 mapping MRI32) is valuable for the preoperative precise evaluation of articular cartilage. Cunningham et al.33) reported a level II prognostic study. They concluded patients whose hips have a lower delayed gadolinium enhanced MRI of cartilage (dGEMRIC) index are less likely to benefit from PAO. Based on the evidence, the preoperative precise evaluation of articular cartilage is important for patient selection of PAO and RAO even in early OA. For symptomatic patients older than 40 years of age who have a dysplastic hip, the operative indications for THA or joint-preserving procedures are controversial.3435363738) Sharifi et al.36) concluded PAO was more cost-effective than THA for patients with Tonnis grade 0, 1, and 2 OA. Hsieh et al.35) evaluated 31 patients who were managed with PAO for the treatment of Tonnis grade 0 to 2 OA in 1 hip and THA for the treatment of Tonnis grade 3 OA in the other hip. More patients preferred PAO to THA (53% compared with 23%) at a mean of 6 years after PAO and 7 years after THA. McAuley et al.39) reported the survivorships of THA in patients 50 years of age and younger were 89% at 10 years of follow-up and 60% at 15 years of follow-up. PAO and RAO remain important options for older patients with early OA or younger patients with advanced OA who are not yet willing to undergo THA because of the high rates of revision THA needed owing to prolongation of the average lifespan. Although it is unclear why the outcome of RAO with cases of older age or advanced stage is acceptable, the cause may be associated with Asian patients' short stature and low body mass index.
In some cases, PAO or RAO may be indicated for hips with lateral joint space narrowing and MRI evidence of articular cartilage damage but with widened and congruent joint space in the abduction view. In these cases, severe articular cartilage degeneration can be observed under the arthroscope during surgery. Recently, arthroscopic femoral osteochondroplasty for cam impingement with microfracture in degenerated cartilage of the acetabulum has been reported.4041) The drilling procedure for damaged articular cartilage as a bone marrow-stimulating procedure was first reported by Pridie42) in 1959 and is often performed as a treatment of osteochondral lesions of knees. For cases with degenerated cartilage, microfracture or drilling combined with PAO or RAO has a potential for regeneration of articular cartilage.
RAO is an effective and safe surgical procedure for symptomatic dysplastic hips of pre- and early-stage OA with expected excellent or good postoperative joint congruency. Additional long-term follow-up studies are needed to demonstrate improvement over the natural history of hip dysplasia.
Figures and Tables
Fig. 1
Preoperative and postoperative radiographs. Preoperative anteroposterior (AP) views in neutral position (A) and abducted position (B). (C) Postoperative AP view in neutral position.
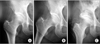
Fig. 2
Postoperative joint congruency is classified into 4 grades: excellent (A), good (B), fair (C), and poor (D).

Fig. 3
Surgical technique. (A) Skin incision. (B) The skin flap is elevated in posterior direction. (C) The rectus femoris is cut. (D) The site for osteotomy of the pubic bone is exposed. (E) The osteotomy line of the posterior wall of the acetabulum. A needle has been inserted in the joint. (F) The outer cortical bone of the ilium is cut with an air drill. (G) The outer cortical bone of the posterior wall and ischium has been cut. (H) The osteotomy of the anterior part of the ilium is shown. (I) The osteotomy of the posterior wall and ischium is shown. (J) The acetabulum is rotated in anterolateral direction. (K) The acetabulum is fixed with two poly-L-lactic acid (PLLA) screws. Ant: anterior, Inf: inferior, Sup: superior.

References
1. Aronson J. Osteoarthritis of the young adult hip: etiology and treatment. Instr Course Lect. 1986; 35:119–128.
3. Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip: a study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995; 77(7):985–989.

4. Nishio A. Transposition osteotomy of the acetabulum for the treatment of congenital dislocation of the hip. Nippon Seikeigeka Gakkai Zasshi. 1956; 30:482–484.
6. Eppright RH. Dial osteotomy of the acetabulum in the treatment of dysplasia of the hip. J Bone Joint Surg Am. 1975; 57(8):1172.
7. Wagner H. Osteotomies for congenital hip dislocation. The Hip Society. The hip: proceedings of the fourth open scientific meeting of the Hip Society. St Louis, MO: C.V. Mosby;1976. p. 45–66.
8. Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984; 66(3):430–436.

9. Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988; (232):26–36.

10. Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. Instr Course Lect. 2001; 50:229–238.

11. Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009; 467(8):2041–2052.

12. Yasunaga Y, Yamasaki T, Ochi M. Patient selection criteria for periacetabular osteotomy or rotational acetabular osteotomy. Clin Orthop Relat Res. 2012; 470(12):3342–3354.

13. Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995; 77(1):73–85.

14. Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10-23 years. Acta Orthop Scand. 1998; 69(3):259–265.

15. Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999; (363):9–20.

16. Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg Am. 2006; 88(9):1915–1919.

17. Hasegawa Y, Kanoh T, Seki T, Matsuoka A, Kawabe K. Joint space wider than 2 mm is essential for an eccentric rotational acetabular osteotomy for adult hip dysplasia. J Orthop Sci. 2010; 15(5):620–625.

18. Millis MB, Kain M, Sierra R, et al. Periacetabular osteotomy for acetabular dysplasia in patients older than 40 years: a preliminary study. Clin Orthop Relat Res. 2009; 467(9):2228–2234.

19. Yasunaga Y, Takahashi K, Ochi M, et al. Rotational acetabular osteotomy in patients forty-six years of age or older: comparison with younger patients. J Bone Joint Surg Am. 2003; 85(2):266–272.

20. Yamaguchi J, Hasegawa Y, Kanoh T, Seki T, Kawabe K. Similar survival of eccentric rotational acetabular osteotomy in patients younger and older than 50 years. Clin Orthop Relat Res. 2009; 467(10):2630–2637.

21. Kaneuji A, Sugimori T, Ichiseki T, Fukui K, Takahashi E, Matsumoto T. Rotational acetabular osteotomy for osteoarthritis with acetabular dysplasia: conversion rate to total hip arthroplasty within twenty years and osteoarthritis progression after a minimum of twenty years. J Bone Joint Surg Am. 2015; 97(9):726–732.

22. Hasegawa Y, Iwase T, Kitamura S, Kawasaki M, Yamaguchi J. Eccentric rotational acetabular osteotomy for acetabular dysplasia and osteoarthritis: follow-up at a mean duration of twenty years. J Bone Joint Surg Am. 2014; 96(23):1975–1982.

23. Yasunaga Y, Ochi M, Yamasaki T, Shoji T, Izumi S. Rotational acetabular osteotomy for pre- and early osteoarthritis secondary to dysplasia provides durable results at 20 years. Clin Orthop Relat Res. 2016; 474(10):2145–2153.

24. Kain MS, Novais EN, Vallim C, Millis MB, Kim YJ. Periacetabular osteotomy after failed hip arthroscopy for labral tears in patients with acetabular dysplasia. J Bone Joint Surg Am. 2011; 93:Suppl 2. 57–61.

25. Kim SD, Jessel R, Zurakowski D, Millis MB, Kim YJ. Anterior delayed gadolinium-enhanced MRI of cartilage values predict joint failure after periacetabular osteotomy. Clin Orthop Relat Res. 2012; 470(12):3332–3341.

26. Millis MB. Congenital hip dysplasia: treatment from infancy to skeletal maturity. In : Tronzo RG, editor. Surgery of the hip joint. 2nd ed. Vol. 1. New York, NY: Springer;1984. p. 329–385.
27. Millis MB, Murphy SB, Poss R. Osteotomies about the hip for the prevention and treatment of osteoarthrosis. Instr Course Lect. 1996; 45:209–226.

28. Shimogaki K, Yasunaga Y, Ochi M. A histological study of articular cartilage after rotational acetabular osteotomy for hip dysplasia. J Bone Joint Surg Br. 2005; 87(7):1019–1023.

29. Yasunaga Y, Ikuta Y, Kanazawa T, Takahashi K, Hisatome T. The state of the articular cartilage at the time of surgery as an indication for rotational acetabular osteotomy. J Bone Joint Surg Br. 2001; 83(7):1001–1004.

30. Kim YJ, Jaramillo D, Millis MB, Gray ML, Burstein D. Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am. 2003; 85(10):1987–1992.

31. Locher S, Werlen S, Leunig M, Ganz R. MR-arthrography with radial sequences for visualization of early hip pathology not visible on plain radiographs. Z Orthop Ihre Grenzgeb. 2002; 140(1):52–57.
32. Watanabe A, Boesch C, Siebenrock K, Obata T, Anderson SE. T2 mapping of hip articular cartilage in healthy volunteers at 3T: a study of topographic variation. J Magn Reson Imaging. 2007; 26(1):165–171.

33. Cunningham T, Jessel R, Zurakowski D, Millis MB, Kim YJ. Delayed gadolinium-enhanced magnetic resonance imaging of cartilage to predict early failure of Bernese periacetabular osteotomy for hip dysplasia. J Bone Joint Surg Am. 2006; 88(7):1540–1548.

34. Garbuz DS, Awwad MA, Duncan CP. Periacetabular osteotomy and total hip arthroplasty in patients older than 40 years. J Arthroplasty. 2008; 23(7):960–963.

35. Hsieh PH, Huang KC, Lee PC, Chang YH. Comparison of periacetabular osteotomy and total hip replacement in the same patient: a two- to ten-year follow-up study. J Bone Joint Surg Br. 2009; 91(7):883–888.
36. Sharifi E, Sharifi H, Morshed S, Bozic K, Diab M. Cost-effectiveness analysis of periacetabular osteotomy. J Bone Joint Surg Am. 2008; 90(7):1447–1456.

37. Teratani T, Naito M, Kiyama T, Maeyama A. Periacetabular osteotomy in patients fifty years of age or older. J Bone Joint Surg Am. 2010; 92(1):31–41.

38. van Bergayk AB, Garbuz DS. Quality of life and sports-specific outcomes after Bernese periacetabular osteotomy. J Bone Joint Surg Br. 2002; 84(3):339–343.

39. McAuley JP, Szuszczewicz ES, Young A, Engh CA Sr. Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004; (418):119–125.

40. Haviv B, Singh PJ, Takla A, O'Donnell J. Arthroscopic femoral osteochondroplasty for cam lesions with isolated acetabular chondral damage. J Bone Joint Surg Br. 2010; 92(5):629–633.

41. Yen YM, Kocher MS. Chondral lesions of the hip: microfracture and chondroplasty. Sports Med Arthrosc. 2010; 18(2):83–89.
42. Pridie KH. A method of resurfacing osteoarthritic knee joints. J Bone Joint Surg Br. 1959; 41(3):618–619.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download