Abstract
Background
The development of pedicle screw-based posterior spinal instrumentation is recognized as one of the major surgical treatment methods for thoracolumbar burst fractures. However, the appropriate level in posterior segment instrumentation is still a point of debate. To assesses the long-term results of two-level and three-level posterior fixations of thoracolumbar burst fractures that have load-sharing scores of 7 and 8 points.
Methods
From January 1998 to May 2009, we retrospectively analyzed clinical and radiologic outcomes of 45 patients with thoracolumbar burst fractures of 7 and 8 points in load-sharing classification who were operated on using two-level posterior fixation (one segment above and one segment below: 28 patients, group I) or three-level posterior fixation (two segments above and one segment below: 17 patients, group II). Clinical results included the grade of the fracture using the Frankel classification, and the visual analog score was used to evaluate pain before surgery, immediately after surgery, and during follow-up period. We also evaluated pain and work status at the final follow-up using the Denis pain scale.
Results
In all cases, non-union or loosening of implants was not observed. There were two screw breakages in two-level posterior fixation group, but bony union was obtained at the final follow-up. There were no significant differences in loss of anterior vertebral body height, correction loss, or change in adjacent discs. Also, in clinical evaluation, there was no significant difference in the neurological deficit of any patient during the follow-up period.
The development of pedicle screw-based posterior spinal instrumentation is recognized as one of the major surgical treatment methods for thoracolumbar burst fractures. This treatment preserves the range of motion of the segment to the maximum extent possible to reduce substantial fixation and, indirectly, the decompression effect.1) However, the appropriate level in posterior segment instrumentation is still a point of debate.
Parker et al.2) explained that a load-sharing score of 7 points or more indicates the poor transfer of load through the most injured vertebral body and points to the necessity for anterior instrumentation and strut grafting. In contrast, Lee et al.3) reported that posterior instrumentation by transpedicular fixation in thoracolumbar burst fractures of 7 points and 8 into the two vertebrae above and one below the fractured vertebra (in long-segment fixation) showed successful results in their 1-year follow-up study.
The present research focused on follow-up studies completed within a minimum of 5 years period after the procedure and presents a retrospective, comparative analysis of two-level posterior fixation and three-level posterior fixation in thoracolumbar burst fractures with loadsharing scores of 7 and 8 points.
From January 1998 to March 2010, 45 patients at the Bundang Jesaeng General Hospital Orthopedic Outpatient Clinic with thoracolumbar burst fractures of 7 points or above in load-sharing classification were operated on using two-level posterior fixation (one segment above and one segment below: 28 patients, group I) or three-level posterior fixation (two segments above and one segment below: 17 patients, group II). Follow-up studies were completed within time duration of more than 5 years after the procedures were completed.
In group I, there were eight males and 20 females, with an average age of 50.5 years (range, 27 to 64 years) at the time of admission. In group II, there were eight males and nine females, with an average age of 49.0 years (range, 25 to 65 years) at the time of admission. The mean load-sharing score, which was measured using preoperative radiographic images, between the two groups was 7.4 in group I (load sharing score 7, 17 patients; load sharing score 8, 11 patients) and 7.3 in group II (load sharing score 7, 12 patients; load sharing score 8, five patients). We excluded patients who had osteoporotic vertebral fractures (bone mineral density < -2.5), severe burst fractures which also required anterior and posterior surgery.
In group I, the average time for follow-up was 6.9 years (range, 5.1 to 12.2 years), and the fractured levels were T12 (n = 4), L1 (n = 17), and L2 (n = 7). In group II, the average time for follow-up was 6.2 years (range, 5.1 to 10.9 years), and the fractured levels were T12 (n = 3), L1 (n = 9), and L2 (n = 5). Autologous iliac bone grafts were used in all patients.
In two-level posterior fixation, transpedicular screws were inserted into one segment above and one segment below the fractured vertebra. In three-level posterior fixation, transpedicular screws were inserted into the two segments above and one segment below the fractured vertebra. We also inserted transpedicular screws into all the fractured vertebra and harvested autologous iliac bone grafts in all patients.
For the reduction of collapsed vertebral bodies and correction of the segmental kyphotic angle, we inserted monoaxial pedicle screws parallel to the endplate of the adjacent normal vertebrae in a convergent direction. Next, the rods and pedicle screws were tightened at a perpendicular angle. This maneuver resulted in a significant reduction of height loss and the correction of the kyphotic angle (Figs. 1 and 2).
Visual analog score (VAS) was used to evaluate pain before surgery, 1 year after surgery, and in the last follow-up period. Also, we assessed pain and work status before surgery, 1 year after surgery, and in the last follow-up period using the Denis rating scale.4) Also, we used Frankel classification to evaluate neurological changes.
In case of all the patients, anteroposterior, and lateral radiographs were taken and centered on fractured vertebra before surgery, immediately after surgery, and at follow-up periods. We measured the height of the anterior vertebral body, the sagittal kyphotic angle, and the disc spaces adjacent to the fractured vertebra (Fig. 3). The angle of kyphosis was measured from the superior endplate of the intact vertebra above the fracture site to the inferior endplate of the intact vertebra below the fracture site.
The loss of anterior vertebral height was represented as the percent change in anterior height when compared to the average height of the intact vertebrae above and below the fracture level. The percentage of upper/lower intervertebral disc height was measured from the anterior vertebral body height of the intact vertebra above and below the fracture site.
Statistical analysis was performed using IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA). We used independent t-tests to compare the difference in results in each category. Furthermore, we used compared t-tests at interrelation analysis for radiologic results before and after surgery. In all statistical analyses, a significance level of < 0.05 was chosen.
In our study, all cases showed considerable reduction in vertebral body height. In group I, the mean anterior body height was 62.5%, preoperatively, and it recovered to 87.3% immediately after surgery. After the 1-year, 2-year, and last follow-up, the height was 84.9%, 83.3%, and 82.5%, respectively. In group II, the mean anterior body height was 57.7% preoperatively, and it recovered to 89.5% immediately after surgery. After the 1-year, 2-year, and last followup, the height was 87.5%, 86.1%, and 83.9%, respectively.
In group I, the mean anterior body height was corrected to 24.8% immediately after surgery and the loss of anterior body height was 4.8% at the last follow-up. In group II, the mean anterior body height was corrected 31.8% immediately after surgery, and the loss of anterior body height was 5.6% at the last follow-up, but there were no significant differences between the two groups (p > 0.05) (Table 1).
In group I, the mean sagittal kyphotic angle was 14.6° preoperatively and 7.8° immediately after surgery. After the 1-year, 2-year, and last follow-up, the mean angles were 9.5°, 10.1°, and 11.0°, respectively. In group II, the mean sagittal kyphotic angle was 17.0° preoperatively and 7.6° immediately after surgery. After the 1-year, 2-year, and last follow-up, the mean angles were 9.7°, 10.4°, and 11.2°, respectively.
In group I, the mean correction angle was 6.8° immediately after surgery, and the mean correction loss was 3.2° at the last follow-up. In group II, the mean correction angle was 9.4° immediately after surgery, and the mean correction loss was 3.6° at the last follow-up. There were no significant differences between the two groups (p > 0.05) (Table 1).
In group I, the mean preoperative upper intervertebral disc height was 32.3%, which recovered to 32.7% immediately after surgery, whereas the mean preoperative lower intervertebral disc height was 33.8%, which recovered to 34.9% immediately after surgery. The upper intervertebral disc height was 27.2%, 25.4%, and 23.4% at the 1-year, 2-year, and final follow-up, respectively and the lower intervertebral disc height was 32.0%, 29.8%, and 27.3% at the 1-year, 2-year, and final follow-up, respectively.
In group II, the mean preoperative upper intervertebral disc height was 31.8%, which recovered to 32.1% immediately after surgery, whereas the mean preoperative lower intervertebral disc height was 34.5%, which recovered to 35.5% immediately after surgery. The upper intervertebral disc height was 29.7%, 27.8%, and 25.6% at the 1-year, 2-year, and final follow-up, respectively and the lower intervertebral disc height was 32.6%, 30.9%, and 29.1% at the 1-year, 2-year, and final follow-up, respectively (Table 1).
The mean loss of the upper/lower intervertebral disc height was 9.3%/7.6% at the last follow-up for group I and was 6.5%/6.4% at the last follow-up for group II. There were no significant differences between the two groups (p > 0.05).
Screw breakage occurred in two patients of the two-level fixation group, but all the patients showed solid bony union at the last follow-up (Fig. 4).
Based on the Frankel classification, in group I, 20 patients were of grade E, five patients were of grade D, and three patients were of grade B. At the last follow-up, there was no clinically detected abnormality in any of the patients. In group II, 13 patients were of grade E and four patients were of grade B. At the last follow-up, there was no significant neurological deficit in any of the patients.
Residual back pain was evaluated using VAS and the Denis pain scale. The mean VAS in group 1 was 0.86 and 0.73 in group II at the last follow-up, and there was no significant difference between the two groups (p > 0.05).
On the Denis pain scale, in group I, 16 of the 28 patients were rated P1, 11 patients were rated P2, and one patient was rated P3 at the last follow-up. There was no relation between final sagittal kyphotic angle and the degrees of pain. In group II, 12 of the 17 patients were rated P1, four patients were rated P2, and one patient was rated P3 at the last follow-up, and there was no significant difference between the two groups (p > 0.05) (Table 2).
In 1994, McCormack et al.5) emphasized that the surgical treatment of acute thoracolumbar spine fractures must include load sharing, which is determined by the amount of damaged vertebral body, the spread of the fragments in the fracture site, and the amount of corrected traumatic kyphosis. A load-sharing score of 7 points or more indicates the poor transfer of load through the most injured vertebral body that, in posterior instrumentation, leads to the eventual loss of correction and a high rate of failure. For this reason, anterior instrumentation and strut grafting is necessary in short-segment posterior instrumentation.
Parker et al.2) further explained that a low load-sharing score, of 6 points or less, indicates adequate sharing of load through both the injured vertebral body itself and the implant to permit only posterior pedicle-screw-based short-segment instrumentation and fusion. Likewise McLain et al.6) reported that in the case of early failure of short segment pedicle instrumentation for thoracolumbar fracture, 19 patients (average duration, 15 months) had been managed with short segment pedicle instrumentation, and 10 patients showed failure of fixation by bending of screws (six patients), osseous collapse (three patients), and caudad screw breakage (one patient).
Meanwhile, Lee et al.3) reported that short-segment fixation is inappropriate for the treatment of burst fractures and long-segment pedicle screw fixation could effectively treat burst fractures of the thoracolumbar and lumbar spine in patients with a load-sharing score of 7 points or above. Kim et al.7) also reported that there were significant differences in the loss of correction angle between long-segment and short-segment posterior fixations, indicating that short-segment posterior instrumentation is insufficient in cases with a load-sharing score of 7 points or above.
However, Altay et al.8) recommend that, especially in patients who need more mobility and who have load-sharing scores of 7 or less and who have Magerl type A31 or A32 fractures, and who do not have neurological deficit, short-segment posterior fixation achieves adequate fixation that does not result in implant failure or correction loss. Yet in Magerl type A33 fractures with a load-sharing score of 7 or above without severe neurologic deficit, long-segment posterior fixation is favorable. In our study, we inserted a pedicle screw into the fractured vertebra in all patients to increase construct stiffness and reduce the level of fixation. Therefore, we used short-segment pedicle fixation for some of the thoracolumbar burst fractures with load-sharing scores of 7 points or above.
Using "intermediate" screws at the level of the fracture is a novel technique to increase the fixation strength of a posterior short segment construct. Biomechanical studies have shown that addition of a screw at the level of the fracture, in a short segment fixation, increases the stiffness of the construct and protects the anterior column during loading.91011)
Chung and Rhym12) reported the easy indirect reduction of fractured vertebrae and improved segmental stability by inserting the pedicle screw at the level of the fractured vertebra. Furthermore, Jeong et al.13) compared the clinical and radiological results between short-segment and long-segment pedicle fixation while inserting the pedicle screw at the level of the fractured vertebra in the thoracolumbar burst fracture.
Recently, Lee et al.3) and Mahar et al.14) reported that segmental fixation with additional screws at the level of the fracture increases construct stiffness and shields the fractured vertebral body from anterior loads, so the technique of limited posterior segmental instrumentation may be useful for the treatment of thoracolumbar burst fractures.
Kanna et al.15) reported that reduction of unstable thoracolumbar burst injuries even with load sharing score of 7 points or more can be achieved and maintained with use of short segment pedicle screw fixation including the fractured vertebra, thus avoiding the need for anterior reconstruction.
In our study, we tried to achieve good sagittal alignment immediately after surgery. Initially, little reduction was obtained by the lordotic prone position. Subsequently, we tried to reduce this using correcting force by tightening the rods and monoaxial pedicle screws, which were inserted parallel to the end plate of the adjacent vertebral body in a perpendicular direction. Furthermore, we tried to achieve early bony union through decortication and autogenous iliac bone grafts. In this way, we achieved satisfactory reduction and bony union in all the patients except for the case of two patients, who experienced screw breakage in two-level posterior fixation group. However, these screw breakages did not affect the clinical and radiological results. We conclude that the proposed method achieves relatively sufficient stability, as there was no loss of bony union and no massive loss of correction kyphotic angle.
Our study is associated with certain limitations. Initially, this study was designed retrospectively and surgical technique was decided by two spine surgeons on their preference, hence we didn't randomize in the assignment of groups. Besides, we reviewed 45 patients, so the statistical power of this study is limited
In our study, we used monoaxial pedicle screws to enhance correction of kyphotic angle, but further studies are required to obtain comparative analysis with respect to polyaxial pedicle screw fixation. Also, we are in the process of initiating a direct comparison study between load sharing score of 6 points or less and 7 points or more.
In conclusion, in our study, there was no significant difference in the clinical or radiologic results of long-term follow-up between two-level and three-level posterior fixation. This means that two-level posterior fixation was used successfully in the selected cases of thoracolumbar burst fractures with a load-sharing score of 7 and 8 points.
Figures and Tables
 | Fig. 1(A) A 19-year-old man with an L1 burst fracture; load-sharing score is seven. (B) Axial computed tomography image shows comminution and canal encroachment. (C) Two-level posterior fixation was done from T12 to L2. (D) Follow-up X-ray shows minimal loss of correction. |
 | Fig. 2(A) A 46-year-old man with an L2 burst fracture; load-sharing score is 7. (B) Axial computed tomography image shows comminution and canal encroachment. (C) Three-level posterior fixation was done from T12 to L3. (D) Follow-up X-ray shows minimal loss of correction. |
 | Fig. 4(A) A 33-year-old man with L2 burst fracture; load-sharing score is 7. (B) Axial computed tomography image shows comminution and canal encroachment. (C) Two-level posterior fixation was done from L1 to L3. (D) The radiograph at 6 months after surgery (left) shows pedicle screw breakage, but the radiograph at 70 months after surgery (right) shows solid bony union and minimal loss of correction. |
Table 1
Comparison of Radiologic Results
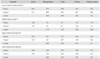
Table 2
Comparison of Back Pain

References
1. Lee CS, Chung SS, Jung HW, Kim ES. Decision of posterior fixation level by load-sharing classification in thoracolumbar and lumbar burst fracture. J Korean Soc Spine Surg. 2001; 8(1):27–38.

2. Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine (Phila Pa 1976). 2000; 25(9):1157–1170.

3. Lee KY, Sohn SK, Kim CH, Song CK. Posterior short-segment instrumentation of thoracic and lumbar bursting fractures: retrospective study related with load-sharing classification. J Korean Soc Spine Surg. 2001; 8(4):497–503.

4. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 8(8):817–831.

5. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994; 19(15):1741–1744.

6. McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures: a preliminary report. J Bone Joint Surg Am. 1993; 75(2):162–167.

7. Kim CH, Hwang JK, Choi YJ, Kim KH, Song JS, Kang JH. Treatment of thoraco-lumbar bursting fractures according to load-sharing classification. J Korean Fract Soc. 2005; 18(1):69–75.

8. Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan O, Tabak AY. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in magerl type a fractures. Eur Spine J. 2007; 16(8):1145–1155.

9. Anekstein Y, Brosh T, Mirovsky Y. Intermediate screws in short segment pedicular fixation for thoracic and lumbar fractures: a biomechanical study. J Spinal Disord Tech. 2007; 20(1):72–77.

10. Dick JC, Jones MP, Zdeblick TA, Kunz DN, Horton WC. A biomechanical comparison evaluating the use of intermediate screws and cross-linkage in lumbar pedicle fixation. J Spinal Disord. 1994; 7(5):402–407.

11. Guven O, Kocaoglu B, Bezer M, Aydin N, Nalbantoglu U. The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech. 2009; 22(6):417–421.

12. Chung JY, Rhym IS. Short segment transpedicular Cotrel-Dubousset instrumentation including involved vertebra for fractures of thoracic and lumbar spine. J Korean Orthop Assoc. 1994; 29(3):940–948.

13. Jeong ST, Cho SH, Song HR, Koo KH, Park HB, Chung UH. Comparison of short and long-segment fusion in thoracic and lumbar fractures. J Korean Soc Spine Surg. 1999; 6(1):73–80.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download