Abstract
An intraarticular osteoid osteoma of the knee is uncommon, and its treatment is challenging. The authors present a case of arthroscopic excision of an intraarticular osteoid osteoma in the distal femur, which was accessible through the knee joint. After confirming the nidus of the osteoid osteoma by computed tomography, the lesion was completely removed arthroscopically. The patient reported complete pain relief immediately after surgery. This case demonstrates that intraarticular osteoid osteomas in the knee joint can be treated by arthroscopic excision and that good results can be obtained.
An osteoid osteoma is a well-known, relatively uncommon, benign osteoblastic tumor composed of osteoid and atypical woven bone. It is usually located in the metadiaphysis of long bones.1234) However, if the tumor exhibits intraarticular involvement, the diagnosis can be more difficult and atypical clinical and radiologic features may lead to a delayed diagnosis.23567) The treatment is aimed at nidus removal traditionally by en-bloc resection, by curettage, or by various other methods.148) Intraarticular osteoid osteomas are rare and although they may be encountered in any joint, the hip, elbow, and talus are most vulnerable.39) The treatment of an intraarticular osteoid osteoma is very challenging, but arthroscopic removal of intraarticular lesions has been performed in many joints.67910) However, arthroscopic excision of an osteoid osteoma in the distal femur located within the synovial cavity of the knee has been rarely reported.8)
Here, we present clinical features, radiographic and histopathological findings, technical aspects of arthroscopic excision, and results of the surgery in the case of an intraarticular osteoid osteoma in the distal femur in a 20-year-old female with a review of the relevant literature.
A 20-year-old female presented at our outpatient department with a complaint of pain persisting for 12 months in the right knee. The pain that was mild at the time of symptom onset became slightly worse at night without association with knee effusion or swelling. She had no definite history of trauma and denied any medical history of rheumatoid arthritis or any other arthritic diseases. A year before this presentation, she visited another hospital for the same symptom where plain radiography and magnetic resonance imaging (MRI) of the knee were performed. The patient knew plain radiographs showed normal findings but MRI revealed a widespread signal change in the subchondral bone of the lateral femoral condyle. The initial diagnosis was bone bruise of the lateral femoral condyle, and she was treated conservatively using intermittent nonsteroidal anti-inflammatory drug medication and physical therapy, which did not result in pain relief.
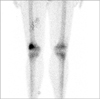
When the patient presented at Dongguk University Gyeongju Hospital, she complained of pain in the anterolateral aspect of the right knee, but joint effusion or tenderness was not evident and the range of knee motion was normal. McMurray and instability tests were negative, and laboratory findings were within normal ranges. Simple radiographs of both knees showed no specific bony abnormality, but the MRI showed a 6 mm × 3.5 mm × 3 mm sized intermediate-low signal intensity nodular lesion on the T1-weighted image and a nodular lesion with central intermediate-low signal intensity surrounded by high signal intensity in the anterosuperior subcortical area of the lateral femoral condyle with adjacent bone marrow edema on the T2-weightedimage (Fig. 1). Computed tomography (CT) of the right knee demonstrated a 5 mm × 3 mm × 3 mm sized lesion with the central nidus and perinidal sclerosis in the anterolateral subcortical area of the distal femur (Fig. 2). Bone scan showed increased uptake at the site corresponding to the lesion in the distal femur (Fig. 3). A diagnosis of osteoid osteoma of the distal femur was established and an arthroscopically assisted excision was scheduled.
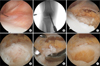
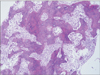
An arthroscopic examination of the knee was carried out through the standard anterolateral and anteromedial portals, which showed normal meniscus, cruciate ligaments, and articular cartilage, but a slightly elevated lesion of synovium at the bottom of the suprapatellar recess near the superior articular margin of the lateral femoral condyle (Fig. 4A). Synovial hyperplasia was minimal. With a 20-gauge needle held in place, C-arm imaging (Fig. 4B) was performed to confirm the correct location of the lesion identified on CT and plain X-ray images using the image tracing technique. Additional superomedial and superolateral portals were made and the synovium over the lesion was then removed using a punch forceps, an electrocautery device, and a shaver (Fig. 4C). The elevated sclerotic rim was removed using small curved osteotomes, and a grossly reddish, dense nidus of osteoid with interconnected trabeculae was observed (Fig. 4D). The lesion was excised using small curved osteotomes and arthroscopic curettes and harvested for histopathologic examination (Fig. 4E). Reactive bone walls were completely removed using a motorized burr, and complete lesion removal was confirmed arthroscopically through the anteromedial, anterolateral, superomedial, and superolateral portals (Fig. 4F). Bone grafting was not performed for the bone defect. Postoperative radiographs and CT confirmed complete removal of the nidus (Fig. 5). Histopathology of the curetted bone specimen confirmed the diagnosis of osteoid osteoma (Fig. 6). The patient recovered uneventfully and pain disappeared immediately after surgery. At the 24 months follow-up, the patient was symptom-free and there was no clinical or radiographic evidence of recurrence of the lesion.
The patient provided consent for publication of this case report and accompanying images.
Osteoid osteomas typically consist of a small yellowish to red pea nidus of osteoid and woven bone with interconnected trabeculae in the background and rim composed of highly vascularized fibrous connective tissue.123) Sclerotic bone reaction may occur to variable degrees around the lesion. Most osteoid osteomas arise in the cortices of long bones usually in the diaphyseal or metadiaphyseal location12) and occur less frequently in the cancellous region and least frequently in the subperiosteal region.2) Intraarticular osteoid osteomas are rare. They may cause atypical joint pain and elude timely diagnosis.2345) Clinically, they may resemble traumatic or degenerative pathologies.367) Intraarticular osteoid osteomas of the knee are commonly misdiagnosed as primary synovitis, medial plica hypertrophy, a meniscal tear, or patellofemoral syndrome and are mistreated accordingly.2) In our patient, the initial diagnosis, that is, a bone bruise of the lateral femoral condyle, was erroneous, and resultantly, a proper treatment was delayed for 1 year. Importantly, a delayed diagnosis may lead to muscle atrophy, tenderness, localized swelling, and possible joint contracture.367) Therefore, in case of joint pain unresponsive to conventional management, a thorough diagnostic workup should be undertaken.
Traditionally, open en-bloc resection of the tumor with the surrounding bone is the surgical treatment of choice for osteoid osteomas. However, this approach necessitates excessive resection of the normal bone due to the wide resection margin and difficulties associated with localizing the nidus, especially in the case of intraarticular osteoid osteomas. The treatment definitely focuses on excision of the nidus of the lesion; however, there are several treatment options including nidus removal and graded removal of the surrounding bone, MRI or CT guided coredrill excision, and destruction of the nidus by radiofrequency, laser, or ethanol ablation.1) Sluga et al.4) compared curettage and en-bloc resection and concluded that curettage could be as effective as en-bloc resection and less invasive. Intralesional excision and percutaneous techniques are the most commonly used treatment methods.1)
Arthroscopically-assisted excision techniques are becoming increasingly popular for both the diagnosis and treatment of intraarticular osteoid osteomas and have produced satisfactory results for the lesions in the ankle,6) hip,7) shoulder,9) and elbow.10) Franceschi et al.3) performed CT-guided en-bloc antegrade and retrograde resection under arthroscopic control in order to remove juxta- or intraarticular osteoid osteomas (the arthroscopic technique was needed to detect and remove all remaining bone tumor particles). Under arthroscopic control, it is even possible to work in a small surgical field and avoid destruction associated with efforts to access hidden lesions during open surgery.3) Even in arthroscopic techniques, it is important to identify the exact location of the lesion because it is located in the subcortical area. In our patient, the exact location of the lesion was preoperatively identified on two-dimensional and three-dimensional CT dynamic scout navigation images. The CT image was traced to preoperative plain X-ray, which was then traced to the C-arm image taken with a 20-guage needle marking the lesion during the arthroscopic procedure (Fig. 4B). So we could confirm the exact location of the lesion during surgery with this image tracing technique.
A small number of case reports on the osteoid osteoma of the knee have been published. Abnousi et al.2) reported a case of an intraarticular osteoid osteoma within the anterior aspect of the medial femoral condyle and described arthroscopic findings. On arthroscopy, the tumor was a broad, raised, well demarcated, firm bony tumor on the anterosuperior medial femoral condyle with redness and hypervascularity of the synovium surrounding the lesion. However, they performed en-bloc resection via miniature arthrotomy, not full arthroscopy.
Complete arthroscopic excision of an osteoid osteoma located within the synovial cavity of the knee has been rarely reported.58) Gunes et al.8) reported a case of arthroscopic excision of an intraarticular osteoid osteoma of the distal femur as in our case. In their report, arthroscopic findings were of a hyperemic area in the synovium and red-purple colored soft tissue after cortical bone lesion removal by arthroscopic curettage.8) In our case, synovial hyperemia was minimal and the slightly elevated lesion was found in the synovial area of the superior aspect of the lateral femoral condyle. After cortical wall removal, a reddish dense nidus of the osteoid with inter-connected trabeculae was observed.
During arthroscopic removal of the lesion, obtaining adequate specimen for histopathological examination can be difficult. For this reason, most authors recommend avoiding the use of a motorized instrument prior to sampling.5810) We did not use any motorized instrument until adequate material was obtained.
Arthroscopic treatment allows the patient to begin early rehabilitation because of the minimal soft tissue damage and bone resection, which also obviates the need for bone grafting.8) In our case, bone grafting was not performed because the extent of bone resection was small and the lesion was considered stable. The advantages of arthroscopic excision include minimal invasiveness, complete nidus removal under direct visualization, maximization of retained normal tissues, the acquisition of adequate specimens for pathologic examination, and rapid postoperative recovery.
We presented the case of a 20-year-old female patient with an intraarticular osteoid osteoma in the right distal femur that was successfully treated by arthroscopically-assisted complete excision. Arthroscopic treatment of an osteoid osteoma around the knee, which is accessible through the joint, can be an effective, minimally invasive method.
Figures and Tables
Fig. 1
(A) Sagittal T1-weighted magnetic resonance imaging (MRI) showing a 6 mm × 3.5 mm × 3 mm sized intermediate-low signal intensity nodular lesion. (B) Sagittal T2-weighted MRI showing a high signal intensity lesion with central intermediate-low signal intensity in the anterosuperior area of the lateral femoral condyle (arrowheads) with adjacent bone marrow edema.
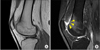
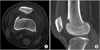
Fig. 2
Axial (A) and sagittal (B) computed tomography images showing a 5 mm × 3 mm × 3 mm sized lesion with a central nidus and perinidal sclerosis in the anterolateral subcortical area of the distal femur.
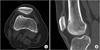
Fig. 4
(A) Arthroscopic image demonstrating a slightly elevated bony lesion at the bottom of the suprapatellar recess near the superior articular margin of the lateral femoral condyle with surrounding minimal hypertrophic synovium. (B) C-arm image taken with a 20-gauge needle held in place to confirm the correct position of the lesion. (C) Removal of the synovium over the lesion using a punching forceps and an electrocautery device. (D) Grossly reddish dense nidus of the osteoid with interconnected trabeculae observed after removal of the sclerotic rim. (E) Excision of the lesion using a small osteotome and curettes. (F) Arthroscopic confirmation of the complete removal of the reactive bone walls performed using a motorized burr.
References
1. Campanacci M, Ruggieri P, Gasbarrini A, Ferraro A, Campanacci L. Osteoid osteoma: direct visual identification and intralesional excision of the nidus with minimal removal of bone. J Bone Joint Surg Br. 1999; 81(5):814–820.
2. Abnousi F, Saliman JD, Fanton GS. Arthroscopic visualization and assisted excision of osteoid osteoma at the knee: a case report and review. Am J Sports Med. 2008; 36(2):375–378.

3. Franceschi F, Marinozzi A, Papalia R, Longo UG, Gualdi G, Denaro E. Intra- and juxta-articular osteoid osteoma: a diagnostic challenge: misdiagnosis and successful treatment: a report of four cases. Arch Orthop Trauma Surg. 2006; 126(10):660–667.

4. Sluga M, Windhager R, Pfeiffer M, Dominkus M, Kotz R. Peripheral osteoid osteoma: is there still a place for traditional surgery? J Bone Joint Surg Br. 2002; 84(2):249–251.
5. Heuijerjans W, Dandy DJ, Harris D. Arthroscopic excision of an intra-articular osteoid osteoma at the knee. Arthroscopy. 1986; 2(4):215–216.

6. Rizzello G, Longo UG, Maffulli N, Denaro V. Arthroscopic removal of an intraarticular osteoid osteoma of the distal tibia. J Foot Ankle Surg. 2010; 49(4):398.e17–398.e21.

7. Nehme AH, Bou Ghannam AG, Imad JP, Jabbour FC, Moucharafieh R, Wehbe J. Arthroscopic excision of intraarticular hip osteoid osteoma: a report of 2 cases. Case Rep Orthop. 2012; 2012:820501.

8. Gunes T, Erdem M, Bostan B, Sen C, Sahin SA. Arthroscopic excision of the osteoid osteoma at the distal femur. Knee Surg Sports Traumatol Arthrosc. 2008; 16(1):90–93.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download