This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Endoprosthetic reconstruction is widely applied for pathological fractures of the proximal humerus; however, functional impairment is usually unsatisfactory. The aims of the current study are to evaluate the reliability of interlocking intramedullary (IM) nailing with cement augmentation as a fixation method in proximal humeral lesions and to assess functional outcomes.
Methods
We reviewed 32 patients with pathological fractures of the proximal humerus who underwent interlocking IM nailing and cement augmentation. Functional scores and pain relief were assessed as outcomes.
Results
The mean follow-up period was 14.2 months. The mean Musculoskeletal Tumor Society functional score and Karnofsky performance status scale score were 27.7 and 75.6, respectively. Improvement of pain assessed using the visual analogue scale was 6.2 on average. Thirty-one patients (97%) experienced no pain after surgery. The mean ranges of forward flexion and abduction were 115° and 112.6°, respectively. All patients achieved stability and had no local recurrence without failure of fixation until the last follow-up.
Conclusions
Proximal interlocking IM nailing with cement augmentation appears to be a reliable treatment option for pathological or impending fractures of the proximal humerus in selected patients with metastatic tumors, even with extensive bone destruction.
Go to :

Keywords: Humerus, Metastasis, Intrameullary nailing, Pathologic fracture
The humerus is the second most common site for long bone metastases following the femur.
1) Although the humerus is not a weight-bearing bone, patients with skeletal metastasis often have lower extremity involvement resulting in a greater dependence on the arms in transfer and ambulation. Because pathological fractures of the humerus severely restrict the use of the involved arm and hand, surgical stabilization of symptomatic impending or pathological fractures is frequently recommended for patients with a reasonable general condition and long life expectancy.
Various surgical options have been proposed for stabilization of pathological humerus fractures, including flexible nailing, intramedullary (IM) nailing, plating, and prosthesis placement.
2345) Determination of the stabilization method is dependent on several conditions, including the location and extent of the metastatic lesion in the humerus, quality of the bone surrounding the lesion, and the patient's general status and life expectancy.
6) Endoprosthetic reconstruction is usually employed for lesions in the proximal humerus, IM nailing for diaphysis, and plating for the distal humerus.
1578) Endoprosthetic reconstruction has the advantage of providing resistance to bending and rotational forces. In addition, it has shown a notable effect on pain relief, local control of the tumor, and stability. On the other hand, endoprosthetic reconstruction may be accompanied by perioperative morbidity, functional impairment of the shoulder, and especially by sacrifice of the rotator cuff insertion onto the greater tuberosity. Even if rotator cuff tendons are securely attached to the prosthesis using various methods, the joint motion is markedly limited after surgery.
In general, stabilization with IM nailing for pathological fractures of the humeral diaphysis has the advantage of a small incision, less soft tissue dissection, short operative time, and early rehabilitation.
1) However, there is some controversy over the application of IM nailing for fractures of the proximal humerus due to the risk of loss of fixation.
3) Accordingly, IM nailing for pathological fractures has so far been confined to diaphyseal lesions.
146891011) Recently, several reports have been published on IM nail fixation techniques for proximal humerus fractures using devices that provide screw stabilization of the humeral head and tuberosity. They provide rigid fixation without extensive soft-tissue dissection.
1213) In our patients, we applied an IM nailing technique, interlocking IM nailing with additional augmentation of the skeletal defect with bone cement, for pathological fractures of the proximal humerus.
The aims of the current study were to evaluate the reliability of interlocking IM nailing with cement augmentation as a fixation method in proximal humeral lesions and to assess the functional outcomes of the patients.
METHODS
Patient Characteristics
We conducted a retrospective review of 46 consecutive patients with an impending or complete pathological fracture involving the proximal humerus between May 2007 and June 2011. All patients consulted with medical oncologists and anesthesiologists regarding life expectancy and perioperative risks. The American Society of Anesthesiologist (ASA) physical status grade was used for evaluation of the general medical condition and tolerance of anesthesia. Patients whose remaining life expectancy was less than 2 months or whose ASA was grade 4 were managed conservatively without surgery. Among the 46 patients, 10 patients did not undergo surgery for the following reasons: 4 patients had short life expectancy; 4 patients had poor general condition; and 2 patients refused surgery. Of the 36 patients who underwent surgery, 4 patients underwent reconstruction with a proximal humeral replacement (tumor prosthesis) because of the extensive lesion of the proximal humerus in which articular surface of the humerus could not be restored. Plate fixation was not used during the study period, and the histology of the primary tumor was not considered when selecting the implant. Consequently, 32 patients were included in the analysis. Of the 32 patients, 5 patients had solitary bone metastases and 27 had multiple bone metastases. Minimum follow-up was 12 months from surgery for the patients who survived. The mean follow-up period was 14.2 months (range, 1 to 62 months). Institutional Review Board approval was obtained for this study. A pathological fracture of the proximal humerus was defined as a fracture with a metastatic lesion of the surgical neck and proximal to the surgical neck. Of the 32 patients, 8 had a lesion confined to the humeral head, 12 in the surgical neck, and 11 in the humeral head and neck, and 1 had an extensive lesion of the neck and shaft. The study included 18 men and 14 women with a mean age of 59.8 years (range, 36 to 86 years). The most common primary tumor was hepatocellular carcinoma (HCC) (9), followed by multiple myeloma (7), lung cancer (5), renal cell carcinoma (3), and breast cancer (2). Twenty-one patients presented with pathological fractures and the other 11 had impending fractures that fulfilled Mirel's criteria. The mean Mirel's score for the 11 patients was 9.5 points (range, 9 to 10 points). Lesion size was defined as the longest length of the lesion on the magnetic resonance imaging scan. The mean size of bone lesions was 7.1 cm (range, 3.0 to 14.2 cm).
Surgical Treatment
Metastatic lesions from hypervascular tumors such as HCC or renal cell carcinoma were devascularized by embolization prior to surgery. The basic principles of surgery included (1) removal of all gross tumors; (2) local adjuvant therapies; (3) choice of IM nails of sufficient length for coverage of the entire humerus; (4) unreamed fashion; (5) multiple proximal and distal interlocking screw fixation; and (6) bone cement augmentation for bone defect. As an exception,
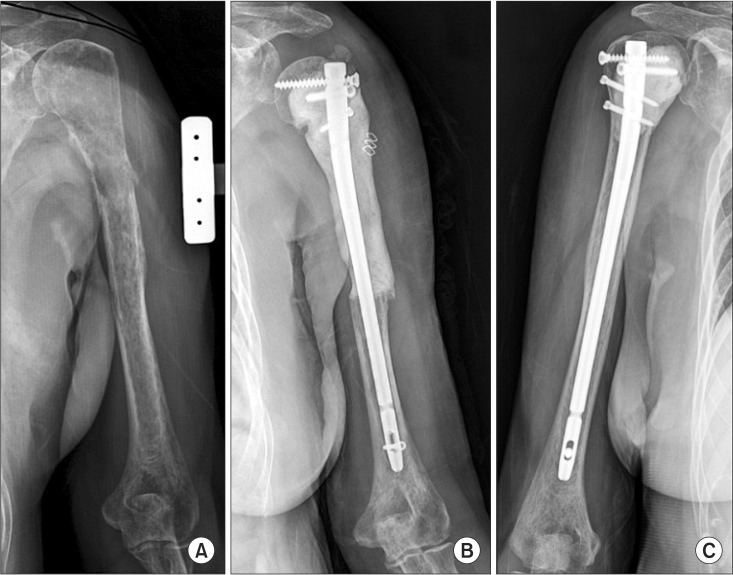
in situ fixation without curettage of the tumor was performed when the general condition of the patient was unacceptable for an aggressive surgical approach and the metastatic lesion was expected to be radiation-sensitive (5 patients). With respect to the surgical approach for curettage, limited deltopectoral approach was preferred. However, for cases with definite soft extension or bone defect, direct approach through the deltoid muscle was performed. When there was an overt fracture, curettage was performed through the fracture gap. Meticulous curettage of the tumor usually necessitated removal of cortical bone, which resulted in a cortical window large enough to put in bone cement. For the impending fracture, a cortical window was made at the anterolateral surface of the humerus or at the thinnest wall of the cortex. After curettage, one or two local adjuvant therapies were employed, such as additional burring, anhydrous alcohol irrigation, and thermal cauterization. Then, an IM nail (Polarus; Acumed, Beaverton, OR, USA) was inserted antegrade in an unreamed fashion in order to avoid IM or systemic spreading of cancer. The nail was inserted carefully with special attention to avoid the proximal end of the nail impinging the rotator cuff tendons or the acromion. The Polarus Plus Locking Humeral Rod, which was approved by the United States Food and Drug Administration (FDA), contains four proximal holes and two distal holes for interlocking screws. Two proximal screws are designed to be inserted into the humeral head and the other two are inserted into the surgical neck (
Fig. 1). We usually inserted four proximal screws and one or two distal interlocking screws in our patients. Bone cement (CMW; DePuy International Ltd, Leeds, UK) was used to fill the skeletal defect after nail fixation to augment fixation. Early motion of the shoulder was allowed from the day after surgery. Passive stretching and gravity-resistance exercise were allowed from 1 week postoperatively. A sling was applied for the first 2 weeks. Adjuvant external beam radiotherapy with 3,000–3,500 Gy was performed in 21 patients (65.6%). Radiotherapy was administered when additional local control was deemed necessary because of the extensive tumor or incomplete removal of the tumor.
 | Fig. 1(A) The anteroposterior (AP) radiograph of the humerus shows a lytic destructive lesion (arrow) with an impending fracture. (B) The coronal view of a T2-weighted magnetic resonance imaging scan shows a metastatic lesion extending to the humeral head. (C) The AP radiograph shows intramedullary rod fixation with cement augmentation and multiple proximal screws are used as a scaffold of cement.
|
Postoperative Course and Measurements
Pain and functional status were evaluated before and 1 month after surgery. Follow-up evaluations were performed every 2 months in the outpatient clinic. Visual analogue scale (VAS) was used to assess the improvement of pain. Musculoskeletal Tumor Society rating scale (MSTS) score was measured for assessment of the functional status. The seven-item MSTS is rated by a clinician and evaluates clinical measures such as pain, range of motion, strength, joint stability, joint deformity, overall function, and general acceptance of the treatment.
14) Karnofsky performance status scale was applied for quantification of general status and activities of daily life. Range of motion (ROM) of the shoulder joint was determined by forward flexion and abduction. Five patients who died within 3 months after surgery were excluded from evaluation of function. Adjuvant chemotherapy and radiation therapy were administered for 22 and 21 patients, respectively. Adjuvant chemotherapy was frequently applied for patients with multiple myeloma and HCC. Adjuvant radiation was commonly used for HCC.
Statistical Analysis
Kaplan-Meier survival analysis was used to evaluate the reliability of the interlocking IM nails and overall survival of patients. Paired t-test was used to evaluate the change of the VAS pain score. Statistical analysis was performed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA).
Go to :

RESULTS
Reliability of Fixation
All 32 cases showed secured rigid fixation until the last follow-up. Follow-up radiographs showed no interval change of the hardware. None of the patients complained of newly developed pain or instability. In 1 patient, loosening of a proximal interlocking screw was observed at 5 months after surgery, which caused disturbance of the shoulder motion. After removal of the screw, the patient recovered full range of motion and was free of pain. There was no incidence of systemic perioperative morbidity such as embolism or aggravation of general status.
Pain Relief and Functional Recovery
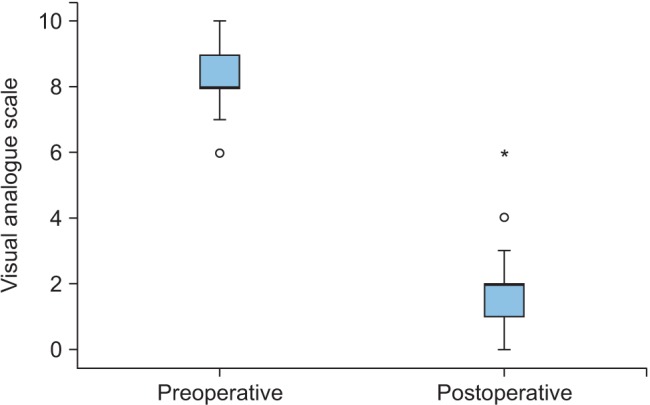
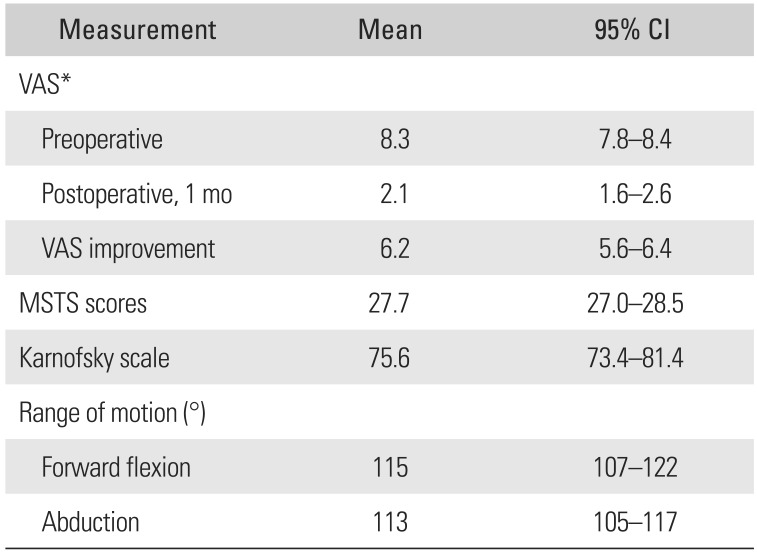
Relief of pain was determined by the change of VAS score. The mean improvement of VAS score was 6.2, and 31 patients (97%) reported pain relief at 1 month after surgery (
Fig. 2). Improvement of VAS score was statistically significant (
p < 0.001). One patient with radial nerve palsy complained of pain for 3 postoperative months until its spontaneous recovery. Evaluation of functional recovery was performed at 3 months after surgery in 27 patients (
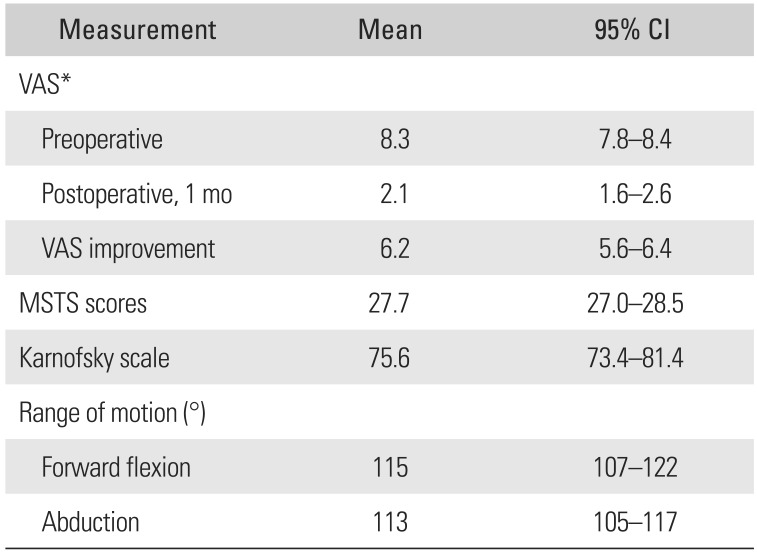
Table 1). The mean MSTS score of the entire cohort at 3 months after surgery was 27.7 (92%). Karnofsky score (mean, 75.6) showed that most of the patients were able to take care of themselves and perform normal activities with some difficulty. Limitation of motion (forward flexion or abduction < 90°) was observed in 1 patient with brain metastasis, whereas most patients showed at least 110° of flexion and abduction, respectively. There was no patient with impingement symptoms. One case of superficial infection was controlled successfully with antibiotics. There was no wound problem. No revision surgery was needed for the humerus until the final follow-up or death.
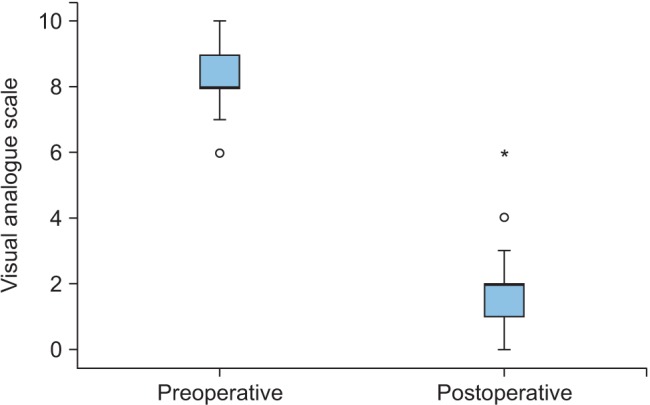 | Fig. 2Change of preoperative and postoperative visual analogue scale (VAS) scores in proximal humerus metastasis. The mean improvement of VAS score (*) after surgery was 6.2.
|
Table 1
Pain Relief and Functional Recovery
|
Measurement |
Mean |
95% CI |
|
VAS*
|
|
|
|
Preoperative |
8.3 |
7.8–8.4 |
|
Postoperative, 1 mo |
2.1 |
1.6–2.6 |
|
VAS improvement |
6.2 |
5.6–6.4 |
|
MSTS scores |
27.7 |
27.0–28.5 |
|
Karnofsky scale |
75.6 |
73.4–81.4 |
|
Range of motion (°) |
|
|
|
Forward flexion |
115 |
107–122 |
|
Abduction |
113 |
105–117 |

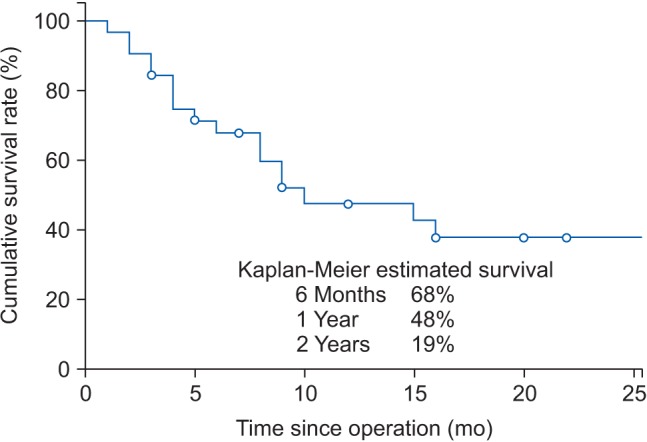
Survival
Survival rates at 6 months and 1 year after surgery were 68% and 48%, respectively (
Fig. 3). The median survival after surgery was 8.0 months (95% confidence interval [CI], 5.0 to 12.0). Two patients died within 1 month due to abrupt aggravation of pulmonary metastasis. Patients with HCC showed the shortest mean survival after surgery (5.4 months). Multiple myeloma patients had the longest mean survival (28 months). There was no radiological evidence of local recurrence until the last follow-up.
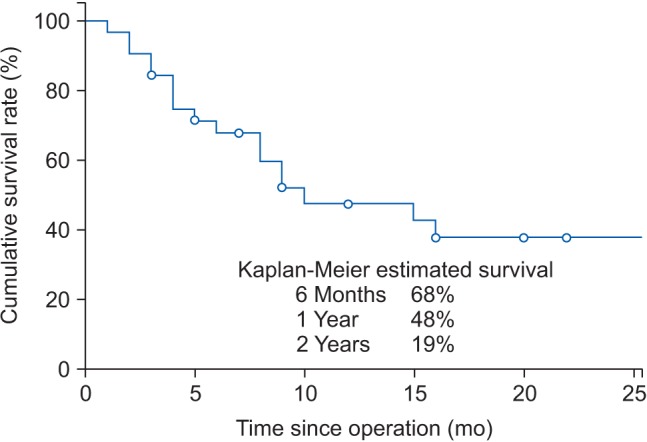 | Fig. 3Kaplan-Meier survival analysis. Forty-eight percent of patients survived more than 1 year after surgical treatment of metastasis.
|
Go to :

DISCUSSION
Prolonged survival of patients with metastasis has justified the necessity of adequate and durable treatment of metastatic lesions despite being palliative in general.
6) Recent studies have reported that nearly half of the patients with pathological fractures could survive more than 1 year.
46) The mean survival of the patients in the current study was more than 1 year (14.2 months) and even the deceased patients lived more than 9 months after surgery. In particular, pathological fractures of the dominant arm significantly impairs the function and quality of life.
IM nailing for the proximal humerus has been considered inappropriate due to the thin cortex and bony defect after curettage.
7) A number of recent clinical series on IM nailing using specially designed nails have reported high union rates and satisfactory functional outcomes of treatment of proximal humeral fractures.
1315) However, the use of IM nails for pathological proximal humeral fractures has not been reported. The findings of the current study suggest that interlocking IM nailing would be an effective and reliable treatment option for pathologic fractures of the proximal humerus.
IM nailing and cement could be a pertinent option not only for the diaphyseal humeral lesion but also for extended metastasis involving the proximal humerus. Our priority has been restoration rather than replacement of the joint for the purpose of preservation of joint motion. Therefore, we expanded the indication of IM nailing for most of the proximal humeral lesions except for cases with extensive destruction of the shoulder joint. Even in cases with a shallow cortical wall after curettage, cement augmentation could successfully deal with the problem of thin cortex and bone defect. Multidimensional screws and interdigitated cement allowed stable fixation even in extensive osteolytic lesions of the humeral head (
Fig. 1). The current study has demonstrated that the well-known concerns related to longevity, local recurrence, and violation of the rotator cuff could be overcome with the combined use of an interlocking proximal humeral nail and cement. All patients who underwent interlocking nailing obtained rigid fixation during the follow-up that surpassed 5 years in some cases. In this series, no radiological local recurrence was observed until the last follow-up. We postulate that there was complete local control owing to the principles of treatment, such as meticulous excision, local adjuvant therapy, and aggressive application of postoperative radiation.
Recent studies on IM nailing have shown that the occurrence of complications caused by violation of the rotator cuff is not a frequent occurrence. Although residual pain and limited motion have been regarded as inevitable problems associated with the use of IM nails, recent studies have reported remarkable improvements. In a study by Blum et al.,
16) pain associated with rotator cuff injury was observed in less than 10% of patients after IM nailing for proximal humeral fractures (n = 151). Studies on pathological fracture of the humeral shaft reported good functional outcomes.
410) In the current study, persistent pain and shoulder stiffness occurred in only 1 and 2 patients, respectively.
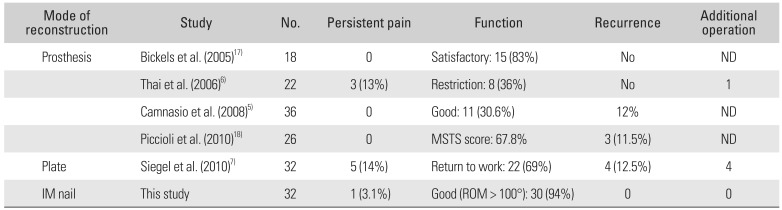
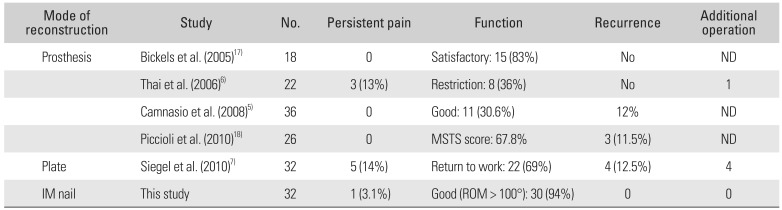
To date, many authors have recommended the use of a prosthesis for the proximal humerus and IM nailing for diaphysis in case of pathologic fractures.
578) Prosthesis is helpful for pain relief and rigid fixation, whereas recovery of function is delayed or inferior to other options (
Table 2).
5671718) In addition, excessive sacrifice of the muscles and tendons during resection results in the inevitable impairment of function.
17) Surgeons should also consider the economic burden and the rehabilitation period that lasts for six to eight weeks in a sling.
1) Some authors have asserted that the locking plate and cement can be a good option for preservation of the rotator cuff.
17) However, plate fixation has many weaknesses, such as extensive soft tissue stripping, potential for nerve injury, and short length of protection.
91215) A local recurrence can result in the loss of fixation and additional surgery.
711) Studies on plating showed 6%–8% of revision rates due to local recurrence followed by the loss of fixation.3,7) Therefore, the use of plates in metastatic lesions is restrictive. Some authors have proposed the use of a modular prosthesis and reattachment of the rotator cuff or a cemented megaprosthesis for extended proximal lesions.
58) However, the modular prosthesis or megaprosthesis, which requires considerable sacrifice of the rotator cuff and ligament, could present worse clinical outcomes and higher risk of complications than the conventional prosthesis.
19) In the current study, the mean length of lesions was 7.1 cm and seven cases required segmental reconstruction with cement due to the long bony defect (> 10 cm). Six patients immediately achieved good range of motion (> 90°) and stable fixation. One patient took 3 months to recover the function of the hand because of the postoperative radial nerve palsy. All patients maintained a functional painless limb until the last follow-up (mean, 17.9 months; range, 3 to 62 months) (
Fig. 4).
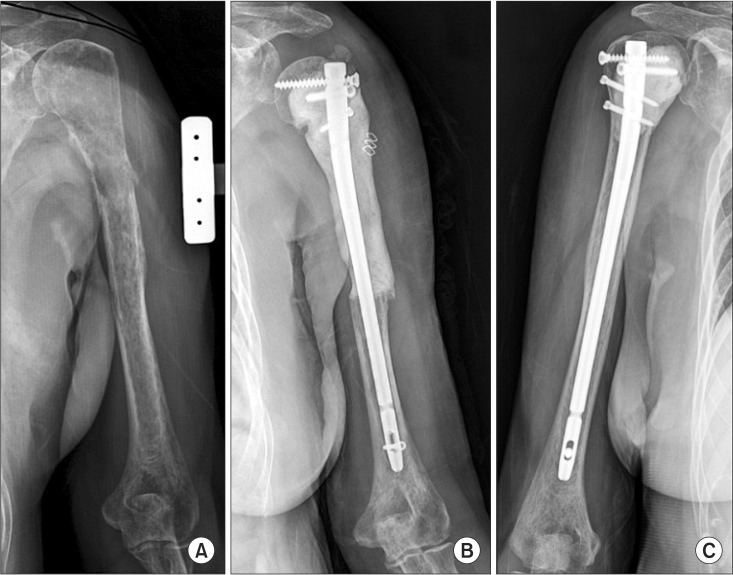 | Fig. 4Reconstruction of a long metastatic lesion using an intramedullary nail and cement. (A) A 69-year-old female with multiple myeloma presented with a long metastatic lesion ranging from the humeral head to the diaphysis. (B) The segmental defect was reconstructed using an intramedullary nail and cement. (C) Stable fixation was maintained for 18 months after reconstruction.
|
Table 2
Review of Literature
|
Mode of reconstruction |
Study |
No. |
Persistent pain |
Function |
Recurrence |
Additional operation |
|
Prosthesis |
Bickels et al. (2005)17)
|
18 |
0 |
Satisfactory: 15 (83%) |
No |
ND |
|
Thai et al. (2006)6)
|
22 |
3 (13%) |
Restriction: 8 (36%) |
No |
1 |
|
Camnasio et al. (2008)5)
|
36 |
0 |
Good: 11 (30.6%) |
12% |
ND |
|
Piccioli et al. (2010)18)
|
26 |
0 |
MSTS score: 67.8% |
3 (11.5%) |
ND |
|
Plate |
Siegel et al. (2010)7)
|
32 |
5 (14%) |
Return to work: 22 (69%) |
4 (12.5%) |
4 |
|
IM nail |
This study |
32 |
1 (3.1%) |
Good (ROM < 100°): 30 (94%) |
0 |
0 |

There are some limitations of this study. First, this is a retrospective review and the number of patients (32) is relatively small. However, considering the rarity of surgical reconstruction of the pathological humerus, 32 is not a small number. The current study is the first report on IM nailing for pathological fractures of the proximal humerus. Second, this study has no control group for comparison of the results. Outcomes of function and pain relief were compared with those of recent studies on prostheses and plates as historical control groups (
Table 2).
In conclusion, proximal interlocking nailing with bone cement augmentation appears to be a reliable treatment option for pathological or impending fractures of the proximal humerus in selected patients with metastatic tumors, even with extensive bone destruction.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download