This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Severe forefoot deformities, particularly those involving the dorsum of the foot, cause inconvenience in daily activities of living including moderate pain on the dorsal aspect of the contracted foot while walking and difficulty in wearing nonsupportive shoes due to toe contractures. This paper presents clinical results of reconstruction of severe forefoot deformity using the anterolateral thigh (ALT) free flap.
Methods
Severe forefoot deformities were reconstructed using ALT flaps in 7 patients (8 cases) between March 2012 and December 2015. The mean contracture duration was 28.6 years.
Results
All the flaps survived completely. The size of the flaps ranged from 8 cm × 5 cm to 19 cm × 8 cm. The mean follow-up period was 10 months (range, 7 to 15 months). There was no specific complication at both the recipient and donor sites. There was one case where the toe contracture could not be completely treated after surgery. All of the patients were able to wear shoes and walk without pain. Also, the patients were highly satisfied with cosmetic results.
Conclusions
The ALT flap may be considered ideal for the treatment of severe forefoot deformity.
Go to :

Keywords: Forefoot, Foot deformities, Acquired, Microsurgical free flaps
Severe forefoot deformities, particularly those involving the dorsal aspect of the foot, cause musculoskeletal discomfort, restricted range of motion, and disturbance in walking, which makes performance of activities of daily living inconvenient.
1) Severe deformities of the dorsal forefoot exhibit specific characteristics depending on the site of occurrence. They are known to occur most frequently in the toes.
2) Patients with dorsal contractures of the forefoot experience difficulty in wearing a shoe and walking. In addition, those patients develop wounds around the toes that are deformed by the contractures.
3) Moreover, functional disturbances in joint areas such as the ankle may affect posture and gait and lead to distortion of the pelvis and spinal curvature.
4)
Severe forefoot deformities commonly give rise to contact ulcers and secondary inflammation.
23) In spite of appropriate treatment, severe forefoot deformities in children can aggravate skeletal deformities as they grow.
56) Therefore, timely aggressive treatment is required for pediatric patients.
For reconstruction of a severe forefoot deformity, an appropriate treatment method should be determined in relation to the location and extent of the area involved. Treatment options are largely divided into skin grafts, local flaps, and free flaps. The basic principle for the reconstruction of severe forefoot deformity is wide release and
en bloc resection. However, skin grafts and local flaps provide limited soft tissue, making the reconstruction challenging in many cases.
78910) Although soft-tissue defects of the dorsum of the foot can be difficult to treat, free flaps provide extensive soft tissue and are, therefore, advantageous compared to other flaps in the reconstruction of the foot.
1112131415) The use of anterolateral thigh (ALT) flaps also allows simultaneous flap harvest and recipient site preparation, thus reducing operating time and enabling the patient to rest in a supine position during the procedure.
1516) And the color and texture of the ALT flap are optimal for lower extremity reconstructions.
12) Although many reports have been published on the use of ALT free flaps in the treatment of foot dorsum damages caused by injury,
111718) no report has discussed the treatment of severe forefoot deformity. Therefore, we report the treatment results of the application of ALT flaps for severe forefoot deformity.
METHODS
Patients and Methods
Between March 2012 and October 2015, 7 patients who had severe forefoot deformity were selected as subjects in this study. According to the classification of forefoot deformities,
21920) contractures are divided into three types: mild type is hypertrophic scar formation with very mild forefoot plantar flexion contracture of some toes; moderate type is involvement of less than three toes in forefoot plantar flexion contracture; and severe type is involvement of three to five toes in significant forefoot plantar flexion contractures. The forefoot deformities in the study population were classified as severe type. Patients were excluded if they had substantial brain injury (Glasgow Coma Scale score of < 15 at 21 days after injury or at the time of discharge) or spinal cord deficit.
There were 4 women and 3 men (6 unilateral and 1 bilateral involvement). Among the various free flaps, we chose the ALT flap that had skin color and texture similar to those of the dorsal foot and allowed the patient to maintain the same posture during surgery. The mean age of the patients was 47 years (range, 11 to 61 years). The mean duration of severe forefoot deformity was 28.6 years (
Table 1).
Table 1
Summary of Patient Data
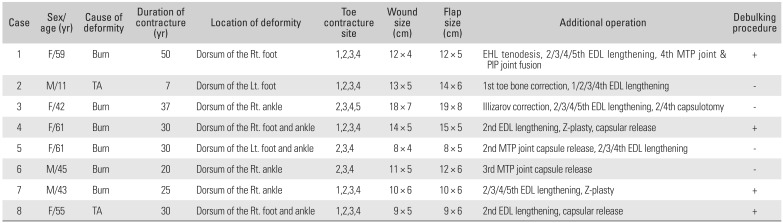
|
Case |
Sex/age (yr) |
Cause of deformity |
Duration of contracture (yr) |
Location of deformity |
Toe contracture site |
Wound size (cm) |
Flap size (cm) |
Additional operation |
Debulking procedure |
|
1 |
F/59 |
Burn |
50 |
Dorsum of the Rt. foot |
1,2,3,4 |
12 × 4 |
12 × 5 |
EHL tenodesis, 2/3/4/5th EDL lengthening, 4th MTP joint & PIP joint fusion |
+ |
|
2 |
M/11 |
TA |
7 |
Dorsum of the Lt. foot |
1,2,3,4 |
13 × 5 |
14 × 6 |
1st toe bone correction, 1/2/3/4th EDL lengthening |
- |
|
3 |
F/42 |
Burn |
37 |
Dorsum of the Rt. ankle |
2,3,4,5 |
18 × 7 |
19 × 8 |
Illizarov correction, 2/3/4/5th EDL lengthening, 2/4th capsulotomy |
- |
|
4 |
F/61 |
Burn |
30 |
Dorsum of the Rt. foot and ankle |
1,2,3,4 |
14 × 5 |
15 × 5 |
2nd EDL lengthening, Z-plasty, capsular release |
+ |
|
5 |
F/61 |
Burn |
30 |
Dorsum of the Lt. foot and ankle |
2,3,4 |
8 × 4 |
8 × 5 |
2nd MTP joint capsule release, 2/3/4th EDL lengthening |
− |
|
6 |
M/45 |
Burn |
20 |
Dorsum of the Rt. ankle |
2,3,4 |
11 × 5 |
12 × 6 |
3rd MTP joint capsule release |
− |
|
7 |
M/43 |
Burn |
25 |
Dorsum of the Rt. ankle |
1,2,3,4 |
10 × 6 |
10 × 6 |
2/3/4/5th EDL lengthening, Z-plasty |
+ |
|
8 |
F/55 |
TA |
30 |
Dorsum of the Rt. foot and ankle |
1,2,3,4 |
9 × 5 |
9 × 6 |
2nd EDL lengthening, capsular release |
+ |

Operative Techniques
All of the patients had a hyperextension deformity at the metatarsophalangeal (MTP) joint, but the severity of deformity differed in each case. All the contractures were debrided thoroughly. Basic procedures such as extensor tendon lengthening, joint capsule release, and capsulotomy were performed. In severe cases with more than 90° of contracture, extensor lengthening and capsule release procedure was not sufficient to correct deformity. Thus, bone fixation with a plate was performed to obtain proper correction and prevent joint instability after capsulotomy.
Additional reconstructive procedures, including arthrodesis and tenodesis, were performed according to the severity of the contracture. In some cases, joint instability was observed and hence tenodesis or K-wire/plate fixation was performed (
Table 1).
Contractures were resolved such that the normal positions of the toes were restored and the flap was designed. Before the flap was elevated, the recipient site was completely reorganized and was marked by more than 0.5 to 1.0 cm larger than the desired flap size (
Table 1). The principle of connecting the flap was to anastomose two available veins after artery anastomosis. When discomfort remained unchanged after surgery due to the flap thickness, a debulking procedure was performed 6 weeks after surgery.
We evaluated the postoperative outcomes in each patient by conducting a questionnaire survey on aesthetic satisfaction (excellent: strongly satisfied, good: satisfied, fair: unsatisfied, and poor: strongly unsatisfied), degree of comfort when wearing shoes (excellent, discomfort has completely disappeared; good, discomfort occasionally remains; fair, discomfort level is the same as the preoperative level; poor, discomfort level is worse than the preoperative level), and possibility of walking. Also, we assessed changes between the preoperative and postoperative toe pain and range of motion of the ankles and toes.
Go to :

RESULTS
In all 8 cases, the flaps for reconstruction were elevated from the contralateral thigh, and the dorsalis pedis artery was used for anastomosis. All the flaps survived. The size of the flaps ranged from 8 cm × 5 cm to 19 cm × 8 cm (wound size: 8 cm × 4 cm to 18 cm × 7 cm) (
Table 1). The arteries were repaired by an end-to-end anastomosis in 7 cases. All but 1 case had an end-to-side anastomosis because of the two-fold increase in the size of the artery. Two veins were repaired in 7 cases; however, in 1 case, 1 of the 2 veins from the flap was too small and thus only one vein was successfully anastomosed.
Tendon lengthening was additionally conducted in all of the cases. In 4 cases where the contractures were not completely resolved, capsule release was additionally performed. In 4 cases, a debulking procedure focused on the toes was performed. The mean follow-up period was 10 months (range, 7 to 15 months).
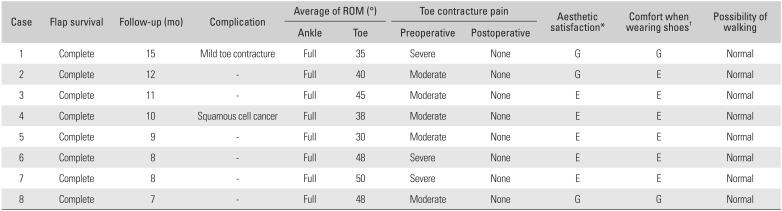
There was no specific complication at both the recipient and donor sites. All of the patients were able to wear shoes and walk without pain. In one case, however, toe contractures were not found to be completely treated after surgery. The ankle range of motion was normal in all of the patients, and the mean toe angle was 42° (range, 35° to 50°) after surgery. In the survey on aesthetic satisfaction conducted 3 months after surgery, aesthetic satisfaction was excellent in 5 patients and good in 3; none of the patients were dissatisfied with the results. Regarding comfort when wearing shoes, 6 patients reported excellent comfort and 2 reported good comfort; none of the patients reported discomfort (
Table 2).
Table 2
Summary of Results
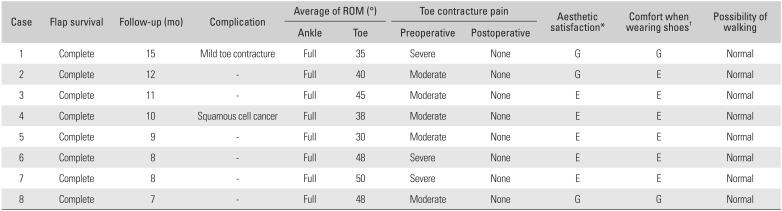
|
Case |
Flap survival |
Follow-up (mo) |
Complication |
Average of ROM (°) |
Toe contracture pain |
Aesthetic satisfaction*
|
Comfort when wearing shoes†
|
Possibility of walking |
|
Ankle |
Toe |
Preoperative |
Postoperative |
|
1 |
Complete |
15 |
Mild toe contracture |
Full |
35 |
Severe |
None |
G |
G |
Normal |
|
2 |
Complete |
12 |
- |
Full |
40 |
Moderate |
None |
G |
E |
Normal |
|
3 |
Complete |
11 |
- |
Full |
45 |
Moderate |
None |
E |
E |
Normal |
|
4 |
Complete |
10 |
Squamous cell cancer |
Full |
38 |
Moderate |
None |
E |
E |
Normal |
|
5 |
Complete |
9 |
- |
Full |
30 |
Moderate |
None |
E |
E |
Normal |
|
6 |
Complete |
8 |
- |
Full |
48 |
Severe |
None |
E |
E |
Normal |
|
7 |
Complete |
8 |
- |
Full |
50 |
Severe |
None |
E |
E |
Normal |
|
8 |
Complete |
7 |
- |
Full |
48 |
Moderate |
None |
G |
G |
Normal |

Case Reports
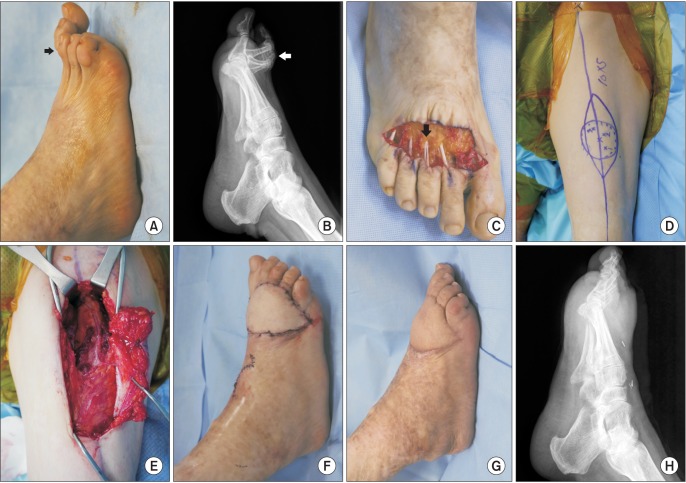
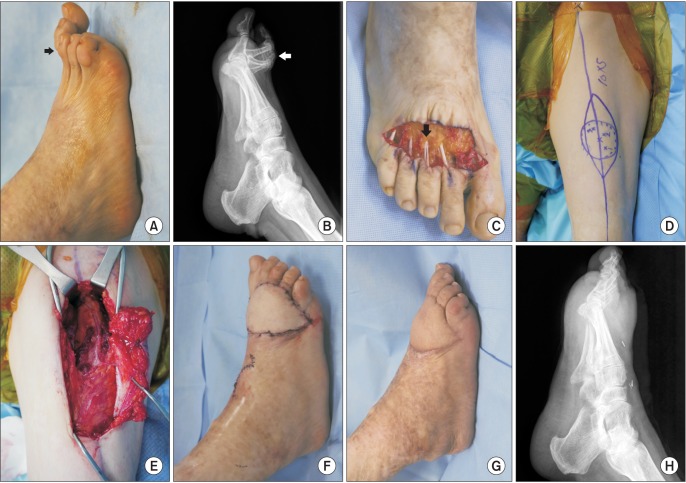
Case 1
A 59-year-old woman experienced a burn injury to the dorsum of her right foot at the age of 9 years. After undergoing appropriate treatment of the injury, she developed contracture of the skin and tendon and pain at the base of the metatarsal head (
Fig. 1A–C). Examination of the contracted right foot revealed adhesiolysis and tenodesis from the extensor hallucis longus to the first metatarsal bone and lengthening of the extensor digitorum longus (EDL) from the second to the fifth toes. By means of contracture release, the fourth toe was relocated and stabilized with a plate at the MTP and proximal interphalangeal joints. The size of the wound was 12 cm × 4 cm (
Fig. 1D). A 12 cm × 5 cm ALT flap was designed on the contralateral thigh (
Fig. 1E). The ALT flap was harvested with 1 perforating artery and 2 veins and the pedicle length was 7 cm (
Fig. 1F). End-to-side anastomosis was performed to the dorsalis pedis artery, and end-to-end anastomosis was performed between the concomitant veins. The donor site was closed with primary closure (
Fig. 1G).
 | Fig. 1Case 1. (A–C) Dorsal post-burn scar contractures led to the development of dorsiflexion contractures of the toes (arrows). (D) All the contractures were debrided, and lengthening of the extensor digitorum longus was performed from the second to the fifth toes (black arrow). (E) The anterolateral thigh (ALT) flap was designed on the contralateral thigh. (F) The ALT flap was harvested in an oval shape and the pedicle length was 7 cm. (G) The skin defect was covered with a 12 cm × 5 cm ALT flap. (H–J) The radiograph and photographs obtained at 9 months after surgery show that the metatarsophalangeal and proximal interphalangeal joints of the fourth toe were stabilized with a plate (black arrow), and the flap survived well.
|
The flap survived, and a debulking procedure was performed on the 4th postoperative week. At the 9-month follow-up, the patient did not report any complications. The patient was satisfied with the aesthetic outcome and did not feel pain while walking after surgery (
Fig. 1H–J).
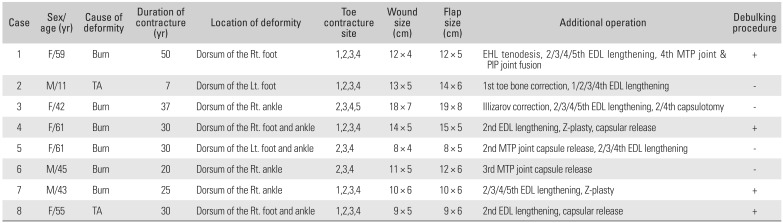
Case 2
A 55-year-old woman sustained a burn injury to the right foot and ankle 30 years before her presentation at our hospital Medical Research Institute. A progressive foot contracture resulted in pain in the right foot during walking. All of the toes exhibited a dorsal flexion deformity (
Fig. 2A, B).
 | Fig. 2Case 2. (A, B) A 61-year-old woman experienced a skin contracture on the right foot dorsum due to a chronic post-burn scar. All the toes exhibited a dorsal flexion deformity in the photograph and radiograph (arrows). (C) All the contracted tissues were debrided, and capsulotomy of the second metatarsophalangeal joint and extensor digitorum longus lengthening from the second to fourth toes were performed (black arrow). (D) The anterolateral thigh (ALT) flap was designed on the thigh. (E) The root of a perforating artery and a vein were ligated, and the ALT flap was raised. (F) The skin defect was covered with a 10 cm × 5 cm ALT flap. (G, H) Photograph and radiograph showing the recipient site at 7 months after surgery.
|
The right foot was treated with skin contracture debridement and the second MTP with joint capsulotomy. EDL lengthening was performed from the second toe to the fourth toe. The size of the wound was 9 cm × 5 cm (
Fig. 2C). A 10 cm × 5 cm ALT flap was designed on the left thigh (
Fig. 2D). With the root of the perforating artery and vein ligated, the ALT flap was raised (
Fig. 2E). End-to-end anastomosis was performed between the perforating and dorsalis pedis arteries and to the veins (
Fig. 2F). The donor site was closed immediately.
The flap survived, and at the 7-month follow-up, a debulking procedure was performed. No complications were reported at the final follow-up. The patient was satisfied with the aesthetic outcome and did not feel pain while walking after surgery (
Fig. 2G, H).
Go to :

DISCUSSION
In general, postburn scar excision and split skin grafting are mainly performed to treat acute burns in the lower extremities.
10) Immediate treatment is essential when a burn injury is sustained. If wounds are cleaned and covered appropriately for early physical therapy, the incidence and severity of long-term sequelae would be reduced. In some cases, however, scar contractures may occur even if wide and complete release and full-thickness skin grafting are performed at the initial stage.
21) When the postburn scar matures and contractures begin to form, patients experience several problems. Burn scars around joints limit range of motion, affect posture and gait, and cause pain among other difficulties. In many cases, secondary inflammations caused by ulcers that persist around postburn scars require surgery. In this study, one patient had persisting ulcer, and it was identified as a squamous cell cancer in the postoperative histological examination.
As were the cases in this report, postburn scar contractures of the dorsal foot usually lead to the development of dorsiflexion contractures in the toe and ankle, restricting patients' ability to wear a shoe or walk. Thus, it is necessary to eliminate contractures and release the toe and ankle in their neutral positions. Contractures in the dorsal foot often lead to hyperextension of the MTP joint, and in severe cases, subluxation or dislocation may occur. Since excessive lengthening may weaken extension strength, the tendon length should be maintained to the extent that allows placement of the hyperextended phalanges in their neutral positions.
2223) In addition, in the present report, the authors performed lengthening to the extent that allowed positioning of the hyperextended phalanges parallel to the plantar aspect of the foot when the ankle was in a neutral position during surgery. The results of this study indicate that the location of the toes after surgery is important for patients' functional satisfaction or elimination of pain after surgery.
The appropriate treatment method for severe forefoot deformity should be determined according to the location and extent of the involved area. The treatment methods are largely divided into skin grafts, local flaps, and free flaps. Skin grafting is a simple technique, but when split- or full-thickness skin grafting is performed after contracture elimination, joint range of motion is limited for a longer duration, and contractures often recur after reconstruction.
A large number of local flap methods related to reconstruction of the foot dorsum have been presented.
24) Local flaps incorporating Z-plasty or V-Y plasty may also be applied, but these methods are not effective in the treatment of wide contractures. In the presence of chronic wide contractures, another method is required to reconstruct defects after elimination of contractures. Traditionally, local fasciocutaneous flaps have been used as patients prefer a simple technique resulting in smaller defects at the donor site. In burns involving the foot, however, there is no adjacent skin laxity because of tissue loss and scarring caused by the burns. In such cases, free flaps of an appropriate size are required.
Previous studies have reported that the recurrence of ulceration and scar contractures, known as the most serious problem in postburn contractures, was not observed when postburn contractures were reconstructed with free flaps.
25) To obtain good results, it is important to prevent further damage to the remaining tissues while achieving a biological coverage so that joints and ligaments can move freely. Free flaps serve this purpose as the skin is covered with extensive soft tissue. Treatment of postburn scar contractures with free flaps after complete maturation of postburn scars is recommended. However, early contraction release is preferred if the postburn scar contracture around the joint causes loss of function.
26)
Unlike in cases of reconstruction using the ALT flap to prevent damages to the foot dorsum,
17) in cases where the ALT flap reconstruction is performed after burn scar resection, the following aspects should be taken into consideration. In particular, several factors should be considered when performing micro-vascular anastomoses for the treatment of postburn scar contractures. The overlying tight skin is often hypertrophic and may be thick, and recipient vessels are placed below the dermal layer, which contains the contraction bands of the scar. Thus, care should be taken not to damage the vessels during dissection. In addition, ALT flaps that allow a long pedicle are advantageous, as it is essential to divide all contraction bands down to healthy tissue. When micro-vascular anastomoses are required in the postburn skin, it is desirable that recipient vessels be placed in the subcutaneous fat or between the muscles during skin closure not to disturb the blood flow.
25)
Particularly, in forefoot reconstruction, a thin flap is important for postoperative ambulation with shoes. After ALT flap operation, our patients were able to wear a shoe and ambulate with only an additional debulking procedure. They obtained good cosmetic and functional outcomes.
The advantages of treating severe forefoot deformity using ALT flaps are as follows: (1) in severe postburn scar contractures with a poor skin condition, a long pedicle is better connected to suitable recipient vessels;
27) (2) ALT flaps have extensive soft tissue for the reconstruction of joints such as the ankle that otherwise require wide excision and well-vascularized tissues for successful results;
1) (3) ALT flaps allow sufficient soft tissue coverage after eliminating postburn scar contractures, preventing the recurrence of skin contractures;
25) and (4) when severe contractures of the dorsal hand occur, flaps covered with the fascia have been reported to be ideal for reconstruction of the extensor tendon after removing scars, and ALT flaps are useful for extensor tendon movements of the foot, as patients can take the tensor fascia lata.
28)
In this study, patients reported that the pain they experienced in their toes before surgery disappeared 1 week after surgery and that they could wear any shoes from 4 weeks after surgery. They also reported that the discomfort of wearing shoes decreased markedly. The remaining discomfort could be completely eliminated after the debulking procedure in the toe area. Furthermore, for vascular connection by the ALT flap, some reports suggest that dual venous anastomosis is beneficial for the safety of the flap.
29) Some authors have argued that the outcomes of single and dual venous anastomoses do not significantly differ and that single venous anastomosis is sufficient.
30) However, as we prefer dual venous anastomosis based on our experience, we anastomosed two available veins, and the result was satisfactory despite the absence of statistical significance due to the small number of cases. And during surgery, the ligaments required lengthening due to significant shortening along with the skin, but other structures such as the bones demonstrated normal growth. Abnormal growth was observed only in pediatric patients who required subsequent correction.
In conclusion, ALT flaps may be considered ideal for the treatment of severe forefoot deformity that causes pain and inconvenience during the performance of activities.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download