Abstract
Background
Bisphosphonates are generally known to adversely affect fracture healing because they inhibit osteoclastic bone resorption. However, some authors argue that bisphosphonates have no adverse effect on the restoration of the mechanical integrity of long bones after fractures. It is unclear whether bisphosphonates can be initiated safely in patients with acute proximal humerus fractures. The aim of this study was to determine whether the early use of a bisphosphonate affects healing and outcomes of osteoporotic proximal humerus fractures treated with a locking compression plate.
Methods
Between August 2004 and June 2013, a total of 82 osteoporotic patients who underwent locking plate fixation of proximal humerus fractures were enrolled retrospectively. The patients were divided into two groups according to the timing of the commencement of treatment with alendronate after surgery: group A (n = 34, initiation of the bisphosphonate treatment within two weeks after surgery) and group B (n = 48, control group, initiation of the treatment three months after surgery). Patients were assessed for radiographic union at 2, 6, 10, and 16 weeks, 6 months, and 1 year after surgery. Clinical assessments were performed using the Constant score and American Shoulder and Elbow Surgeons (ASES) score at 1 year after surgery.
Results
No significant differences were observed between the two groups with respect to radiographic and clinical outcomes after locking plate fixation. All patients obtained fracture union, and the mean time to radiographic union was similar in group A and group B (6.3 and 6.6 weeks, respectively; p = 0.67).
Osteoporosis is a systemic skeletal disease characterized by low bone mass and micro-architectural deterioration of bone tissue with a consequent increase in both bone fragility and susceptibility to fractures.1) In addition to vertebral, hip, and distal forearm fractures, humeral fractures are among the most common osteoporotic fractures, and the average lifetime risk in a 50-year-old Caucasian to experience this type of fracture has been estimated at 12.9% for women and 4.1% for men.2) Osteoporotic fractures are associated with significant morbidity, and fractures of the hip, vertebrae, and humerus have been shown to be associated with excess mortality.34) Fractures of the proximal humerus account for 5% of all fractures and are the third most common fracture pattern occurring in individuals over the age of 65.56)
The widely used bisphosphonate (BP) therapy decreases bone resorption and hypercalcemia and reduces osteolysis of bone metastasis.78) A number of randomized clinical trials have shown that BPs increase the bone density and reduce the risk of vertebral, non-vertebral, and hip fractures.89) Nevertheless, BPs are not recommended in patients with acute fractures because they are known to delay the process of fracture healing and suppress remodeling of the callus.1011) However, Kim et al.12) reported that the early administration of BPs does not appear to affect the rate of healing of an intertrochanteric fracture or the incidence of complications. Gong et al.13) argued that the early initiation of a BP treatment did not affect fracture healing or clinical outcomes. Cao et al.11) reported that after a bone fracture, BPs did not appear to interfere with the early phases of repair; rather, continuous BP use resulted in a larger, stronger callus. Recently, Li et al.14) reported that early administration of BPs after surgery did not appear to delay fracture healing time either radiologically or clinically. Furthermore, according to the changes in bone mineral density (BMD) and bone turnover markers, the anti-resorptive efficacy of BPs given immediately after surgical repair should positively affect the rate of subsequent fractures based on a meta-analysis of randomized controlled trials.
It is unclear whether BPs can be initiated safely in patients who have sustained an acute proximal humerus fracture. We hypothesized that the early initiation of a BP treatment for patients treated with a locking compression plate fixation system would not affect fracture healing or clinical outcomes. The aim of this study was to determine whether the early use of a BP affects healing and outcomes of osteoporotic proximal humerus fractures treated with a locking compression plate.
Following Dankook University Hospital Institutional Review Board exempt approval (IRB no.: DKUH IRB 2013-10-011), a total of 127 patients over the age of 50 years who had undergone locking compression plate fixation of proximal humerus fractures and had been diagnosed with osteoporosis were enrolled retrospectively from August 2004 to June 2013. All patients were recommended BMD examinations preoperatively.
Fracture pattern grading was accomplished radiographically using the Neer classification system: a part/segment was considered displaced if it was separated from its neighboring segment by more than 1 cm or angulated by more than 45°.1516)
The inclusion criteria were: (1) preoperative BMD confirming osteoporosis with a T-score of < −2.5; (2) no BP therapy during two years preceding the fracture; and (3) 2-, 3-, or 4-part displaced fractures (including surgical neck fractures) of the proximal humerus treated with locking compression plate fixation. The exclusion criteria were: (1) refusal to take or a contraindication for BP medication; (2) a condition capable of affecting BMD or bone metabolism, such as renal or adrenal insufficiency, diabetes, rheumatoid arthritis, or thyroid disease; (3) fractures treated with another method (conservative treatment, Kirschner wire fixation, screw fixation, intramedullary nailing, or prosthesis); (4) open fractures; (5) stable fractures; (6) isolated tuberosity fractures; (7) head split fractures and fracture dislocations; and (8) fractures with significant ipsilateral injuries that could prevent early rehabilitation. All patients received an oral BP (alendronate, 70 mg) weekly. In group A (34 patients), the BP treatment was started within 2 weeks after surgery, whereas in group B (48 patients), it was initiated 3 months after surgery, as fractures usually heal within 3 months. For an effective comparison, patients who started to receive the BP treatment between 2 weeks and 3 months after surgery were excluded. A total of 45 patients were excluded, leaving a study sample of 82 patients.
The investigators examined the sex, age, type of fracture, BMD, body mass index, and American Society of Anesthesiologists (ASA) scores and found no statistically significant difference between the groups (Table 1).
All patients underwent surgery for proximal humerus fracture fixation using a proximal humeral internal locking system (PHILOS) plate (Synthes; Stratec Medical Ltd., Mezzovico, Switzerland). All the operations were performed by the same surgeon (JBS) with the patient placed in the beach chair position on a radiolucent table under general anesthesia with the aid of intraoperative fluoroscopy. An anterior deltopectoral approach was chosen for the exposure of all fractures. The biceps tendon was identified and retracted, and with the fracture exposed between the tuberosities and behind the bicipital groove, transosseous sutures were occasionally used to assist with the reduction of tuberosity fragments. The fracture was reduced and held temporarily with K-wires. Reduction was checked fluoroscopically and the PHILOS plate was then applied using a minimum of four proximal locking screws. The plate was positioned with the aid of an aiming device 5 to 8 mm distal to the upper end of the greater tuberosity and 2 to 4 mm posterior to the bicipital groove. Five to six locking angularly stable screws were placed into the humeral head and three to four standard cortical screws were placed in the shaft. Final intraoperative images were taken to verify correct screw placement, and the range of motion (ROM) was assessed to minimize the risk of any postoperative impingement (Fig. 1).
The wound was closed over a suction drain, which was removed 24 hours later. Postoperatively, the arm was supported in a sling. Pendular movements were started from the first postoperative day and the shoulder was mobilized with active assisted exercises, which was followed by active exercises three weeks later.
The patients were routinely followed at 2, 6, 10, 16 weeks, 6 months, and 1 year after surgery. Standard anteroposterior and axillary radiographs were obtained at each visit. Radiogrpahic union was defined as the presence of bridging of trabeculae or osseous bone in three of four (medial, lateral, anterior, and posterior) cortices (Fig. 2). In each evaluation of the union of proximal humerus fractures, the images were interpreted by two orthopedic surgeons (JSY and JWR). In cases where no agreement could be reached on the union by the two observers, the mean union times were used as a representative value.
To evaluate loss of fixation, the cervicodiaphyseal angle (formed by the intersection between a line perpendicular to the anatomical neck and a line parallel to the axis of the humeral diaphysis) was measured on true shoulder anteroposterior view radiographs by two orthopedic surgeons (JSY and JWR) immediately postoperatively and at the last follow-up (Fig. 3). To minimize interobserver bias, the mean difference of the cervicodiaphyseal angle between immediate postoperative and last follow-up measurements was used as a representative value. Fixation failure was defined as more than 10° of difference of the cervicodiaphyseal angle between immediate postoperative and last follow-up measurements.
Clinical outcomes were assessed at 1 year after surgery using the American Shoulder and Elbow Surgeons (ASES) scoring system, Constant score (CS),17) and the ROM of the shoulder. The ROMs of the shoulder assessed were the forward flexion, external rotation, and internal rotation.
The reliability of agreement in determining radiological fracture healing between two observers who were blinded to the treatment was assessed using Kappa coefficients. Kappa coefficients were interpreted as follows: < 0 denoting poor agreement, 0 to 0.2 slight agreement, 0.2 to 0.4 fair agreement, 0.4 to 0.6 moderate agreement, 0.6 to 0.8 substantial agreement, and > 0.8 almost perfect agreement.18)
Group results were compared using the Pearson chi-square and the Student t-test for continuous variables. Correlation analyses were conducted to identify the relationships between the variables. Statistical analyses were performed with use of SPSS ver. 21.0 (IBM Co., Armonk, NY, USA), and p-values of < 0.05 were considered statistically significant.
All patients showed evidence of fracture healing. In group A, radiographic fracture union was obtained at six weeks in 28 patients (82%) and at ten weeks in 6 patients (18%). In group B, radiographic fracture union was achieved at 6 weeks in 38 patients (79%) and at 10 weeks in 10 patients (21%). The average time to radiographic union was similar (6.3 weeks; range, 6 to 10 weeks) between group A and group B (6.6 weeks; range, 6 to 10 weeks) (p = 0.65). There was no significant intergroup difference in the proportion of patients who obtained healing at 6 weeks after surgery (p = 0.81) (Table 2). Interobserver reliability reached the level of “almost perfect agreement” with a weight kappa coefficient of 0.82.
Five patients in group A (14.7%) and 4 patients in group B (8.3%) showed fixation failure with more than 10° of difference in the cervicodiaphyseal angle measured on radiographs immediately postoperatively and at the last follow-up. The mean difference of the cervicodiaphyseal angle was not significantly different between group A (average, 3.7°; range, 0° to 24°; standard deviation, 6.1°) and group B (average, 2.2°; range, 0° to 17°; standard deviation, 7.3°) (p = 0.238) (Table 2).
At 1 year after surgery, the ASES score averaged 80.2 points (range, 62 to 92 points) in group A and 78.6 points (range, 58 to 94 points) in group B. No significant difference was observed in the mean ASES score between the two groups (p = 0.61). In addition, the mean CS at 1 year after surgery was 71.6 points (range, 54 to 90 points) in group A and 73.1 points (range, 58 to 92 points) in group B, indicating no significant difference between the groups (p = 0.63). The respective mean values of the ROM of the shoulder were 130.5° (forward flexion), 44.2° (external rotation), and the eleventh thoracic level (internal rotation) in group A and 128.4°, 46.2°, and the tenth thoracic level in group B (p = 0.89) (Table 3).
In this study, all patients showed evidence of fracture healing without any statistically differences between two groups. Moreover, clinical results based on the ASES score were satisfactory in both groups.
Eriksen et al.19) reported that the administration of zoledronic acid for more than two weeks after surgical treatment for low-energy hip fractures increased hip BMD scores and significantly reduced the risks of subsequent vertebral and hip fractures, while also decreasing mortality. Dirschl et al.20) reported that the loss of femoral neck BMD in patients with a hip fracture was five times greater than that found in a normal population. They recommended pharmacological or some other forms of intervention during the first critical year following a hip fracture to prevent accelerated bone loss and reduce the risk of subsequent fractures during this period.
Although the BP therapy reduces the risks of a secondary fracture and mortality,2122) the optimal timing of BP administration following a proximal humerus fracture in osteoporotic patients remains unclear. Several animal studies have demonstrated that BPs can delay callus remodeling.1123) Clinically, Odvina et al.24) observed significantly delayed healing of fractures in patients on long-term alendronate. Rozental et al.25) compared 43 distal radius fracture patients who were taking a BP with 153 controls: the time to union in the BP group was 55 days compared to 49 in the control group. However, these clinical studies did not evaluate the effect of BP medication on fracture healing in patients who had no history of taking BPs.
In contrast, some authors have reported that BPs promote fracture healing. Amanat et al.26) demonstrated that a single dose of zoledronic acid significantly increased the callus volume and mechanical strength. Fleisch27) reported that the callus size was either not influenced or was increased by BPs, and it never decreased due to the slowing of callus resorption. Moreover, this resulted in a paradoxical increase in the mechanical strength.
In the present study, there was no delay in the healing of proximal humerus fractures fixed by locking plate fixation. Recently, several authors have reported that the early initiation of BPs does not delay the healing of fractures fixed by a plate or by nailing.1213) One possible explanation is the healing mechanism of proximal humerus fractures treated with locking plate fixation. Gong et al.13) noted that fractures treated by means of plate fixation involve primary bone healing between fragments rather than bridging due to external callus formation. The difference between cancellous and cortical bone could be another reason. In a fracture of compact long bones, where fracture bone debris must be absorbed to allow room for new bone formation,28) a resorption process is critical initially. However, proximal humerus fractures involve cancellous bone, in which the space for new bone formation is larger than that in compact bones. Therefore, we speculate that the healing of proximal humerus fractures stabilized by a locking plate may not be suppressed by a reduction in the resorption process by BPs owing to the spacious environment offered by cancellous bone.
Our study had several limitations. First, we defined radiographic fracture union as bridging of trabeculae or osseous bone across fracture lines, but a quantitative assessment of this type of union may be necessary by, for instance, measuring the callus size on computed tomography scans. Second, in order to evaluate the influence of BP administration on fracture healing, it would have been better to compare the effects on the BMD and bone metabolism under the same condition. Third, the sample size was not large enough to evaluate the outcomes between two groups. Finally, the duration of follow-up was short; a longer follow-up is needed to determine the prevalence of complications and the long-term effects of an early osteoporosis treatment. Nevertheless, the significance of this this lies in the fact that it attempted to analyze the influence of early BP administration in osteoporotic proximal humerus fractures.
In conclusion, early initiation of BP treatment in patients with an osteoporotic proximal humerus fractures treated by locking compression plate fixation did not affect fracture healing or clinical outcomes, although our sample size was too small to detect a rare complication of non-union.
Figures and Tables
 | Fig. 2Radiographs taken at 6 weeks after operation showing union of the proximal humerus fracture. (A) Anteroposterior view to confirm the medial and lateral cortices. (B) Axillary view to confirm the anterior and posterior cortices. |
Table 1
Demographic Data
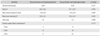
Table 2
Radiologic Outcomes
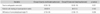
Table 3
Clinical Outcomes at 24 Weeks after Operation

References
1. Consensus development conference: prophylaxis and treatment of osteoporosis. Osteoporos Int. 1991; 1(2):114–117.
2. Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005; 16:Suppl 2. S3–S7.

3. Johnell O, Kanis JA, Oden A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004; 15(1):38–42.

4. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006; 17(12):1726–1733.

5. Helmy N, Hintermann B. New trends in the treatment of proximal humerus fractures. Clin Orthop Relat Res. 2006; 442:100–108.

6. Baron JA, Barrett JA, Karagas MR. The epidemiology of peripheral fractures. Bone. 1996; 18:3 Suppl. 209S–213S.

7. Silverman S, Christiansen C. Individualizing osteoporosis therapy. Osteoporos Int. 2012; 23(3):797–809.

8. Reginster JY, Burlet N. Osteoporosis: a still increasing prevalence. Bone. 2006; 38:2 Suppl 1. S4–S9.

9. Osugi K, Miwa S, Marukawa S, Marukawa K, Kawaguchi Y, Nakato S. Diaphyseal femoral fatigue fracture associated with bisphosphonate therapy: 3 more cases. Acta Orthop. 2011; 82(1):112–113.

10. Li C, Mori S, Li J, et al. Long-term effect of incadronate disodium (YM-175) on fracture healing of femoral shaft in growing rats. J Bone Miner Res. 2001; 16(3):429–436.

11. Cao Y, Mori S, Mashiba T, et al. Raloxifene, estrogen, and alendronate affect the processes of fracture repair differently in ovariectomized rats. J Bone Miner Res. 2002; 17(12):2237–2246.

12. Kim TY, Ha YC, Kang BJ, Lee YK, Koo KH. Does early administration of bisphosphonate affect fracture healing in patients with intertrochanteric fractures? J Bone Joint Surg Br. 2012; 94(7):956–960.

13. Gong HS, Song CH, Lee YH, Rhee SH, Lee HJ, Baek GH. Early initiation of bisphosphonate does not affect healing and outcomes of volar plate fixation of osteoporotic distal radial fractures. J Bone Joint Surg Am. 2012; 94(19):1729–1736.

14. Li YT, Cai HF, Zhang ZL. Timing of the initiation of bisphosphonates after surgery for fracture healing: a systematic review and meta-analysis of randomized controlled trials. Osteoporos Int. 2015; 26(2):431–441.

15. Neer CS 2nd. Displaced proximal humeral fractures: I. classification and evaluation. J Bone Joint Surg Am. 1970; 52(6):1077–1089.
16. Neer CS 2nd. Displaced proximal humeral fractures: II. treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970; 52(6):1090–1103.
17. Constant CR, Gerber C, Emery RJ, Sojbjerg JO, Gohlke F, Boileau P. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008; 17(2):355–361.

18. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33(1):159–174.

19. Eriksen EF, Lyles KW, Colon-Emeric CS, et al. Antifracture efficacy and reduction of mortality in relation to timing of the first dose of zoledronic acid after hip fracture. J Bone Miner Res. 2009; 24(7):1308–1313.

20. Dirschl DR, Henderson RC, Oakley WC. Accelerated bone mineral loss following a hip fracture: a prospective longitudinal study. Bone. 1997; 21(1):79–82.

21. Beaupre LA, Morrish DW, Hanley DA, et al. Oral bisphosphonates are associated with reduced mortality after hip fracture. Osteoporos Int. 2011; 22(3):983–991.

22. Harrington JT, Ste-Marie LG, Brandi ML, et al. Risedronate rapidly reduces the risk for nonvertebral fractures in women with postmenopausal osteoporosis. Calcif Tissue Int. 2004; 74(2):129–135.

23. Li J, Mori S, Kaji Y, Mashiba T, Kawanishi J, Norimatsu H. Effect of bisphosphonate (incadronate) on fracture healing of long bones in rats. J Bone Miner Res. 1999; 14(6):969–979.

24. Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005; 90(3):1294–1301.

25. Rozental TD, Vazquez MA, Chacko AT, Ayogu N, Bouxsein ML. Comparison of radiographic fracture healing in the distal radius for patients on and off bisphosphonate therapy. J Hand Surg Am. 2009; 34(4):595–602.

26. Amanat N, McDonald M, Godfrey C, Bilston L, Little D. Optimal timing of a single dose of zoledronic acid to increase strength in rat fracture repair. J Bone Miner Res. 2007; 22(6):867–876.

27. Fleisch H. Can bisphosphonates be given to patients with fractures? J Bone Miner Res. 2001; 16(3):437–440.

28. Bindra RP. Basic pathology of the hand, wrist, and forearm: bone and joint. In : Berger RA, Weiss AP, editors. Hand surgery. Philadelphia, PA: Lippincott Williams & Wilkins;2004. p. 1–21.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download