Abstract
Background
Recurrence of glenohumeral dislocation after arthroscopic Bankart repair can be associated with a large osseous defect in the posterosuperior part of the humeral head. Our hypothesis is that remplissage is more effective to prevent recurrence of glenohumeral instability without a severe motion deficit.
Methods
Engaging Hill-Sachs lesions were observed in 48 of 737 patients (6.5%). Twenty-four patients underwent arthroscopic Bankart repair combined with remplissage (group I) and the other 24 patients underwent arthroscopic Bankart repair alone (group II). Clinical outcomes were prospectively evaluated by assessing the range of motion. Complications, recurrence rates, and functional results were assessed utilizing the American Shoulder and Elbow Surgeons (ASES) score, Rowe score, and the Korean Shoulder Score for Instability (KSSI) score. Capsulotenodesis healing after remplissage was evaluated with magnetic resonance imaging.
Results
The average ASES, Rowe, and KSSI scores were statistically significantly higher in group I than group II. The frequency of recurrence was statistically significantly higher in group II. The average loss in external rotation measured with the arm positioned at the side of the trunk was greater in group II and that in abduction was also higher in group II.
Arthroscopic repair is being widely used as the first-line treatment in the management of recurrent anterior dislocation. A Hill-Sachs lesion, the posterosuperior humeral head bone defect, has been described a common cause of arthroscopic Bankart repair failure.1) The term, engaging Hill-Sachs lesion, was first used by Burkhart and De Beer1) to describe a defect of the humeral head that was large enough for the edge of the humeral head to drop over the anteroinferior glenoid rim during abduction and external rotation when the arm was at the functional position. Previous studies reported that patients with a huge posterolateral bone loss in the humeral head were not good candidates for arthroscopic Bankart repair because of the risk of repair failure when performed alone.2) In 1972, Connolly3) recommended filling of the posterolateral bone defect in the humeral head with the posterior part of the capsule and the infraspinatus tendon to reduce the possibility of postoperative redislocation. As a modification of the Connolly3)'s open infraspinatus tenodesis, Wolf and his associates45) introduced arthroscopic Hill-Sachs remplissage in conjunction with Bankart lesion repair.
In this study, we aimed to compare the outcomes of arthroscopic remplissage with Bankart repair and arthroscopic Bankart repair alone. We hypothesized that (1) the remplissage of the humeral head bone loss performed in combination with arthroscopic Bankart lesion repair would not have any harmful effects on the postoperative shoulder function compared to simple arthroscopic Bankart repair and (2) the remplissage procedure would improve postoperative shoulder stability.
Between March 1998 and May 2012, a total of 737 patients had surgical interventions for recurrent anterior shoulder instability. Of these, 48 patients (6.5%) who met the inclusion criteria underwent the arthroscopic procedure. These patients were randomly divided into two groups: patients who had Hill-Sachs remplissage in conjunction with an anterior labral and capsule repair (Bankart procedure) (group I) and patients who had an anterior labral and capsule repair only (group II). Each group included 24 patients. There were 37 males and 11 females. The average age at the time of surgery was 29.3 ± 4.12 years (range, 21 to 39 years). The dominant arm was involved in 79.1% of the patients (38 patients). All patients had a remarkable history of glenohumeral dislocation, which required reduction at least once in the emergency room, with recurrent shoulder dislocation during sleep at night. The average interval between the onset of shoulder instability and the operation was 79 months (range, 12 months to 30 years). The mean frequency of glenohumeral dislocation was 35 (range, 10 to 90). Preoperative three-dimensional computed tomography (3D-CT) and arthroscopy revealed the presence of humeral head bone defects and recurrent labral tears and preservation of glenoid bone stock of less than 25% in all patients.
All 48 patients underwent preoperative 3D-CT scan along with radiography of the affected shoulder to assess the extent of the humeral head bone loss and glenoid bone loss.12) Complete follow-up was not available for 2 patients in group I and 6 patients in group II. Of the 40 patients, 7 patients (17.5%) experienced surgical failure.
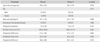
There was no statistically significant difference in baseline characteristics between the groups (Table 1).
The included patients showed recurrent anterior shoulder instability with a large engaging Hill-Sachs lesion at any degrees of abduction/external rotation during diagnostic arthroscopy and imaging studies and a minor but substantial glenoid bone loss (below 25%) on the en face 3D-CT view (Calanda III).
The exclusion criteria included symptomatic recurrent anterior shoulder instability associated with only soft tissue pathologies, major anteroinferior glenoid bone loss of above 25%, primary anterior shoulder instability, multidirectional instability of the shoulder and voluntary posterior shoulder instability, recurrent instability associated with rotator cuff tear, and preexisting severe shoulder arthritis. All patients were informed of the risks and benefits of the surgical procedures before enrollment and signed informed consents. This study was approved by the Ulsan University Hospital Institutional Review Board (IRB no.: 2015-02-018).
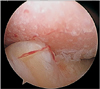
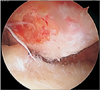
Under general anesthesia, the patient's position was changed from the supine to the lateral decubitus position. The shoulder was examined in abduction and external rotation: dislocation was noted in abduction and external rotation of < 90°, and there was no case of spontaneous reduction. In 30° of posterior tilting of the shoulder, the affected arm was abducted 30° and flexed 15° forward. Then, 8 lbs of longitudinal traction and 4 lbs of vertical side-arm traction were applied to the shoulder. Huge engaging Hill-Sachs lesions were identified in group I and II (Figs. 1 and 2). Dynamic arthroscopic examination was performed with the shoulder externally rotated and the arm abducted 45°. Engagement of the Hill-Sachs lesion was recognized by this dynamic arthroscopic examination. In group I, the surfaces of Hill-Sachs lesions were debrided with a motorized-shaver, a burr, and a ring curette, and then the posterior capsule and the inferior capsule were abraded. The number of anchors used for remplissage was 2 (2 anchors and 4 sutures were used for the remplissage technique). The first bio-cork screw suture anchor (5.0 mm; Arthrex, North Naples, FL, USA) was inserted through the posterior portal from the infraspinatus tendon to the posterior articular capsule until it reached the center of a Hill-Sachs lesion (Fig. 3). Hill-Sachs lesions were filled with the posterior capsule and the infraspinatus tendon. The tendon and the posterior articular capsule were penetrated by a 16-gauge needle 1 cm downward and upward from the posterior portal. The surgeon tied the knots at the end of the operation after completing Bankart repair; tying knots earlier would make further procedures more difficult because the posterior portal is closed by the remplissage. The number of anchors was 4, and the anchor positions were 5, 4, 3, and 2 o'clock for the typical Bankart technique. The surgeon used simple stitches with knot-suture-anchors utilizing suture anchor instruments (3.5 mm; Arthrex). Once classic Bankart repair was successfully completed, remplissage was performed. The surgeon performed bursectomy before suturing the capsule. The remplissage technique was completed by making a knot in the subdeltoid space through the posterior portal (Fig. 4).
In group II, the patient underwent only Bankart repair even in the presence of a huge engaging Hill-Sachs lesion; however, more capsular plication was done to prevent recurrent dislocation and failure after surgery. The inferior capsule was plicated tightly with 2 or 3 sutures, and the anterior capsule was plicated more tightly with 4 or 5 sutures. The number of anchors was five, and the anchor positions were 6, 5, 4, 3, and 2 o'clock. Capsular shift was greater in patients with Bankart repair alone to obtain more stability during shoulder motion.
Postoperatively, an immobilization abduction brace was applied for about 4 to 6 weeks only allowing gentle daily living activities. The pendulum exercise was commenced at1 to 2 weeks postoperatively. Passive and active range of motion was practiced from 6 to 12 weeks postoperatively. Strengthening exercise was started at 12 weeks postoperatively.
Patient data were prospectively collected and assessments were performed by two independent clinicians who were blinded to the study at 3, 6, 9, and 12 months after surgery and yearly thereafter. The mean duration of follow-up was 66 months (range, 24 months to 15 years). The shoulder function was evaluated using the American Shoulder and Elbow Surgeons (ASES) score and Rowe6) score, and stability was assessed preoperatively and postoperatively using the Korean Shoulder Score for Instability (KSSI) score.7) Preoperative and postoperative ranges of shoulder motions in active forward elevation and internal and external rotation in abduction were recorded.
Magnetic resonance imaging (MRI) was performed to evaluate the operated shoulder at 6 months (5.5 to 6.5 months) postoperatively (Fig. 5). All MRI assessments were performed using the same scanner: a 3.0-T closed-type scanner (Achieva 1.5T A-Series MRI system; Philips, Amsterdam, the Netherlands) and a local small-sized flexible coil. The following sequences were collected: oblique sagittal T1-weighted spin-echo sequence without fat saturation (repetition time [TR], 419 ms; echo time [TE], 20 ms; slice thickness, 3 mm) and fat-saturated oblique coronal T1-weighted spin-echo sequence (TR, 433 ms; TE, 20 ms; slice thickness, 3 mm), oblique coronal T2-weighted fast spin-echo sequence (TR, 3,500 ms; TE, 80 ms; slice thickness, 3 mm), and angled axial (perpendicular to the glenoid joint surface) T1-weighted spin-echo sequence (TR, 400 ms; TE, 20 ms; slice thickness, 3 mm). The field of view was 15 cm in all sequences. Accurate assessment in coronal, parasagittal, and axial images of each plane were performed. Two independent radiologists who specialize in musculoskeletal disorders analyzed the MRI scans. The percentage of remplissage defined as the filling of the humeral head defect was classified into four grades8): complete for 100% coverage; nearly complete for 75% to 99% coverage; partial coverage for 50% to 74% coverage; and poor for less than 50%. Interobserver agreement was high with a Cronbach α of 0.919.
The data were described as the mean ± standard deviation. The D'Agostino-Pearson test was applied to analyze measured data distribution. Chi-square test and two-sample t-test were used to compare unpaired results. The chi-squared test was applied to compare categorical data. The level of significance for all analyzed data was determined at p < 0.05.
There were 2 cases of follow-up loss in group I with the remplissage procedure (group I). In the remaining patients of group I, no objective evidence of recurrent dislocation was found in clinical tests at the last follow-up. There were 6 cases of follow-up loss in in group II without the remplissage procedure. There were 5 cases of recurrence in group II. In the remaining patients of group II, there was no objective evidence of recurrent dislocation in clinical tests at the last follow-up although severe deficit in external rotation was noted in 1 patient and apprehensive outcome was observed in another patient.
The postoperative mean ASES score was 87.2 ± 6.57 in group I and 83.5 ± 5.13 in group II (p = 0.039). The postoperative mean Rowe score was 91.4 ± 3.97 in group I and 84.8 ± 5.83 in group II (p = 0.000). The postoperative mean KSSI score was 85.8 ± 4.00 in group I and 80.8 ± 4.82 in group II (p = 0.000).
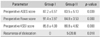
The postoperative average ASES, Rowe, and KSSI scores and frequency of recurrence were significantly different between the two groups (Table 2).
Twenty-two of 24 patients (91.7%) in group I, agreed to undergo postoperative MRI at 6 months after the operation to evaluate capsulotenodesis healing. MRI imaging studies can be useful to assess healing of the capsule and tendon to the bone. There was evidence of healing of the posterior aspect of the capsule and the tendon into the humeral head defect in all 22 patients. Of these 22 patients with postoperative MRI, 19 (86.3%) had a remplissage of > 75%, 2 had a remplissage of > 50%, and 1 had a remplissage of < 50%.
No patient in group I and 5 patients in group II were disappointed with the outcome of the arthroscopic procedure due to postoperative anterior shoulder dislocation. Other patients were satisfied or very satisfied.
Postoperative shoulder mobility was compared between the groups at 6 and 12 months postoperatively and at the last follow-up. Compared with the normal (contralateral) side, the mobility of the affected side in group I showed an average loss of 11.3° ± 5.76° in external rotation and 12.1° ± 7.21° in abduction at the last follow-up. None of the patients expressed dissatisfaction with regard to the slight loss in external rotation. In group II, the affected side exhibited an average loss of 14.4° ± 7.42° in external rotation and 15.2° ± 9.40° in abduction at the last follow-up when compared to the unaffected side. Two patients reported dissatisfaction when the arm was externally rotated at maximum 90° abduction and at the side. In group II, even though only Bankart repair was performed in the presence of a huge engaging Hill-Sachs lesion, more capsular plication was done to prevent recurrent dislocation and postoperative failure. This resulted in the greater loss of abduction and external rotation in the Bankart repair only group compared with the remplissage group (Table 3). The frequency of recurrent dislocation was higher in group II in spite of more capsular plication. Therefore, we suggest that the remplissage procedure will be a better option than capsular plication for huge engaging Hill-Sachs lesions.
Wound infection or iatrogenic nerve injury were not reported in all patients. Recurrence of anterior shoulder instability was noted postoperatively in none of the patients in group I and 5 patients in group II.
The two patients who were lost to the postoperative follow-up in group I were 28 years old and 31 years old, respectively. One had a seizure attack at 14 months after the operation, but the patient did not want further follow-up. The other patient did not want further follow-up, either. In group II, there were 6 patients lost to follow-up. One of them immigrated to a foreign country. Another 2 patients had a seizure attack at 6 months and 9 months postoperatively when seizure medications were discontinued. Seizure medications were recommenced for these patients and they did not agree to have further follow-up. Five patients had a postoperative recurrence in group II. Two patients had a recurrence due to a slip at 6 weeks, and 3 months postoperatively and they did not want a revision operation. The other three patients had a traumatic recurrence of glenohumeral dislocation at 11, 13, and 20 postoperative months, respectively, after a fall by landing on the abducted shoulder while playing sports (1 during badminton and 2 during a volleyball game). One of them had an open Latarjet procedure. The other 2 patients did not want reoperation: this was a single episode and the patient continued to perform activities of daily living until the latest follow-up whereas the other patient had a severe limitation of shoulder motion.
Our results suggest that the remplissage procedure performed in combination with Bankart repair for anterior shoulder instability with a huge engaging Hill-Sachs lesion can produce excellent functional results with little complications, compared to single Bankart repair.
An engaging Hill-Sachs lesion was first described by Burkhart and De Beer1) as a defect in the posterolateral humeral head that was so huge that the edge would drop down over the glenoid rim when the arm was abducted and externally rotated.9)
Boileau et al.8) found that the presence of a huge Hill-Sachs lesion was considerably associated with recurrent instability. Even though the exact indications for the treatment of huge humeral head bone loss are as yet ill-defined,9) Burkhart and De Beer1) reported that recurrent anterior shoulder dislocation was found in 100% of patients with an engaging Hill-Sachs lesion, which could be evaluated with the aid of fluoroscopy preoperatively or with aid of arthroscopy intraoperatively. In the current study, we evaluated the engaging huge Hill-Sachs lesions through physical examination performed under anesthesia and dynamic arthroscopic examination.
The management of bone loss was reassessed as part of the anterior shoulder stabilization procedure by Bushnell et al.10) in 2008 and Lynch et al.9) in 2009. Various methods including rotational oseotomies1112) and filling of the humeral head with allograft,1314) soft tissue,35) and humeral prostheses have been suggested. Weber et al.11) designed a humeral rotational osteotomy to increase retroversion of the proximal humerus, which mostly resulted in severe complications according to Kronberg and Brostrom1215) and Miniaci and Berlet14) reported the results of size-matched structural osteochondral allografts, which carried the risk of nonunion, graft resorption, and hardware failure. Transhumeral impaction grafting eliminates the potential risks unambiguously associated with the humeral rotational osteotomy and other nonanatomic procedures.9) Kazel et al.13) suggested percutaneous impaction grafting of the humeral head, but the procedure failed to sufficiently reduce the bone defect. Re et al.16) explicated a similar transhumeral bone grafting. Chapovsky and Kelly17) reported an all-arthroscopic procedure to fill the bone loss with an osteoarticular allograft. Humeral head resurfacing arthroplasty has also been suggested to manage focal bone loss of the humeral head, and it is considered to be a less prosperous option.18)
Filling the posterolateral humeral head bone loss with transposition of the infraspinatus tendon and posterior capsule is a viable solution for engaging Hill-Sachs lesions.5) Remplissage can be performed by open3) or arthroscopic45) techniques. The procedure described by Connolly3) is essentially the reverse of the McLaughlin procedure, which was the open transfer of the infraspinatus tendon and posterior capsule into the Hill-Sachs lesion. Purchase et al.5) reported a procedure using arthroscopic infraspinatus tenodesis and posterior capsulodesis for huge posterolateral humeral head bone loss. The principles of all arthroscopic remplissage techniques were previously reported by Wolf and his associates.45) In a study by Wolf and Pollack,4) 22 patients were satisfied with a remplissage procedure and 2 patients had poor outcomes. Ko et al.19) started to perform a remplissage procedure for recurrent anterior dislocation involving a huge engaging Hill-Sachs lesion in their patients. In their study, the final decision on the application of the remplissage procedure was made based on intraoperative dynamic arthroscopic evaluation. Elkinson et al.20) reported that the addition of the remplissage to Bankart repair in specimens with a 30% Hill-Sachs defect prevented engagement of the lesion and enhanced stability in their experimental model. The patients in our study also had huge Hill-Sachs defects above 30%.
Franceschi et al.21) described in 2012 that their 25 patients obtained excellent outcomes of arthroscopic remplissage and Bankart repair without any redislocation or resubluxation at 2 years postoperatively.22) In our study, excellent outcomes were obtained in patients who had huge Hill-Sachs lesions with medium glenoid bone defects for up to 10 years. On the intergroup comparison, recurrence was not observed in any of the patients in group I, indicating more significant improvement than group II where five cases of recurrence were noted at the last follow-up. We utilized the Rowe6) score and the KSS score for instability assessment,8) which was previously found to be valid, responsive, and reliable to evaluate functional improvement. In group I, the Rowe score for stability improved from 43.6 preoperatively to 91.4 at the final follow-up (p = 0.0021), which was considered good to excellent in 81% of the patients postoperatively. The KSS score for instability improved from 46.6 preoperatively to 84.9 at the final follow-up (p = 0.0015). On the other hand, Nourissat et al.23) reported that their patients showed no significant difference in different planes of range of motion between groups divided according to the additional application of the remplissage procedure.22) Patients in the study, however, did not report any posterosuperior pain at the final follow-up. Park et al.24) described that 3 out of 20 patients reported recurrence of instability. In our study, recurrence of instability was noted in two patients. Park et al.25) reported that there was evidence of tendon incorporation and filling into the Hill-Sachs defect following an arthroscopic remplissage, and patients were satisfied with the procedure and demonstrated minimal loss of external rotation (average, 5.8°) at an early follow-up. We also observed infraspinatus tendon was incorporated into the Hill-Sachs defect after the remplissage procedure and there was slight loss of external rotation. Boileau et al.8) reported that healing of the posterior aspect of the capsule and the infraspinatus tendon into the humeral defect was observed in all patients: 74% of the patients had a remplissage of ≥ 75% and 98% of their patients had a stable shoulder at the time of the last follow-up. In our study, except for the 2 patients who did not agree to further follow-up after the remplissage procedure, patients in group I were satisfied or very satisfied with the outcomes. In a study by McCabe et al.,26) aggressive capsulolabral reconstruction with a remplissage in traumatic instability patients with moderate bone loss and engaging humeral Hill-Sachs lesions yielded acceptable outcomes. Koo et al.27) and Haviv et al.18) reported that their remplissage procedure was advantageous in that (1) it was a minimally invasive procedure for changing an intraarticular lesion into an extra-articular one; (2) there was no need for any additional graft materials; (3) complications associated with an open approach could be avoided; and (4) the procedure was simple and easy to perform. We also agree with these advantages described in the studies. Patients in group II underwent Bankart repair alone even though there were huge engaging Hill-Sachs lesions. However, more capsular plication was done to prevent redislocation in these patients, which could be the cause of greater loss of abduction and external rotation compared with the remplissage group. The incidence of redislocation was higher in group II in spite of the greater capsular plication. Therefore, we suggest that the remplissage procedure is a better option than extensive capsular plication in the presence of a huge engaging Hill-Sachs lesion.
In spite of the risk of the transferred infraspinatus and posterior capsules limiting external rotation of the shoulder, it was judged that the benefits of the procedure would outweigh the risk, and none of the patients reported interference with daily living activities. Because of the potential abridgement of the arc of motion of the humeral head associated with the remplissage, one could anticipate a greater limitation of motion of the operated shoulder.28) However, the extent of restricted motion of the operated shoulder was relatively small in a study of Boileau et al.8): an average of 8° in external rotation with the arm at the side and 9° in external rotation with the arm in abduction. Furthermore, the study showed a small limitation of below 10° in external rotation did not significantly affect return to overhead activities8): 90% of their patients could return to sports activities involving overhead activities, suggesting that there may be a functional adaptation of the shoulder joint after the remplissage through rebalancing of scapulothoracic and glenohumeral motion.8)
There were a few limitations to this study. First, the sample size was small although it was determined based on a power analysis. This was because of the relative rarity of huge engaging Hill-Sachs lesions and the recent introduction of the remplissage technique. Second, all procedures were performed by the same surgeon; therefore, the results of this study may not reflect general surgical outcomes of the procedure. Nevertheless, the study included unique postoperative care and follow-up assessments and the same operative indications and consistent surgical technique were applied in all patients. The follow-up period was also relatively long. We hope that the results of our study will be confirmed in further studies involving a large cohort of patients.
In conclusion, compared to the single arthroscopic Bankart repair, the remplissage procedure combined with arthroscopic Bankart repair showed superior efficacy for prevention of the recurrence of anterior shoulder instability and had no significant impact on shoulder mobility. Therefore, the remplissage procedure performed in combination with arthroscopic Bankart repair can be a potential solution for engaging Hill-Sachs lesions without considerable anteroinferior glenoid bone defects.
Figures and Tables
 | Fig. 5(A) Postoperative magnetic resonance imaging: the infraspinatus and posterior capsule are well attached to Hill-Sachs lesion. (B) Oblique sagittal view. |
Table 1
Demographic Data of the Study Population
References
1. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000; 16(7):677–694.

2. Balg F, Boileau P. The instability severity index score: a simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007; 89(11):1470–1477.
3. Connolly JF. Humeral head defects associated with shoulder dislocations: their diagnostic and surgical significance. Instr Course Lect. 1972; 21:42–54.
4. Wolf EM, Pollack ME. Hill-Sachs "Remplissage": an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy. 2004; 20:Suppl 1. e14–e15.
5. Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-Sachs "remplissage": an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy. 2008; 24(6):723–726.

6. Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978; 60(1):1–16.
7. Tae SK, Rhee YG, Park TS, et al. The development and validation of an appraisal method for rotator cuff disorders: the Korean Shoulder Scoring System. J Shoulder Elbow Surg. 2009; 18(5):689–696.

8. Boileau P, O'Shea K, Vargas P, Pinedo M, Old J, Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am. 2012; 94(7):618–626.

9. Lynch JR, Clinton JM, Dewing CB, Warme WJ, Matsen FA 3rd. Treatment of osseous defects associated with anterior shoulder instability. J Shoulder Elbow Surg. 2009; 18(2):317–328.

10. Bushnell BD, Creighton RA, Herring MM. Bony instability of the shoulder. Arthroscopy. 2008; 24(9):1061–1073.

11. Weber BG, Simpson LA, Hardegger F. Rotational humeral osteotomy for recurrent anterior dislocation of the shoulder associated with a large Hill-Sachs lesion. J Bone Joint Surg Am. 1984; 66(9):1443–1450.

12. Kronberg M, Brostrom LA. Proximal humeral osteotomy to correct the anatomy in patients with recurrent shoulder dislocations. J Orthop Trauma. 1991; 5(2):129–133.

13. Kazel MD, Sekiya JK, Greene JA, Bruker CT. Percutaneous correction (humeroplasty) of humeral head defects (Hill-Sachs) associated with anterior shoulder instability: a cadaveric study. Arthroscopy. 2005; 21(12):1473–1478.

14. Miniaci A, Berlet G. Recurrent anterior instability following failed surgical repair: allograft reconstruction of large humeral head defects [Abstract]. J Bone Joint Surg Br. 2001; 83:Suppl 1. 19–20.
15. Kronberg M, Brostrom LA. Rotation osteotomy of the proximal humerus to stabilise the shoulder: five years' experience. J Bone Joint Surg Br. 1995; 77(6):924–927.

16. Re P, Gallo RA, Richmond JC. Transhumeral head plasty for large Hill-Sachs lesions. Arthroscopy. 2006; 22(7):798.e1–798.e4.

17. Chapovsky F, Kelly JD 4th. Osteochondral allograft transplantation for treatment of glenohumeral instability. Arthroscopy. 2005; 21(8):1007.

18. Haviv B, Mayo L, Biggs D. Outcomes of arthroscopic "remplissage": capsulotenodesis of the engaging large Hill-Sachs lesion. J Orthop Surg Res. 2011; 6:29.

19. Ko SH, Shin SM, Jo BG. Outcomes of minimally 1 year follow-up for the arthroscopic Remplissage technique with Hill-Sachs lesion. J Orthop. 2013; 10(1):41–45.

20. Elkinson I, Giles JW, Faber KJ, et al. The effect of the remplissage procedure on shoulder stability and range of motion: an in vitro biomechanical assessment. J Bone Joint Surg Am. 2012; 94(11):1003–1012.

21. Franceschi F, Papalia R, Rizzello G, et al. Remplissage repair: new frontiers in the prevention of recurrent shoulder instability: a 2-year follow-up comparative study. Am J Sports Med. 2012; 40(11):2462–2469.

22. Wolf EM, Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg. 2014; 23(6):814–820.

23. Nourissat G, Kilinc AS, Werther JR, Doursounian L. A prospective, comparative, radiological, and clinical study of the influence of the "remplissage" procedure on shoulder range of motion after stabilization by arthroscopic Bankart repair. Am J Sports Med. 2011; 39(10):2147–2152.

24. Park MJ, Tjoumakaris FP, Garcia G, Patel A, Kelly JD 4th. Arthroscopic remplissage with Bankart repair for the treatment of glenohumeral instability with Hill-Sachs defects. Arthroscopy. 2011; 27(9):1187–1194.

25. Park MJ, Garcia G, Malhotra A, Major N, Tjoumakaris FP, Kelly JD 4th. The evaluation of arthroscopic remplissage by high-resolution magnetic resonance imaging. Am J Sports Med. 2012; 40(10):2331–2336.

26. McCabe MP, Weinberg D, Field LD, O'Brien MJ, Hobgood ER, Savoie FH 3rd. Primary versus revision arthroscopic reconstruction with remplissage for shoulder instability with moderate bone loss. Arthroscopy. 2014; 30(4):444–450.

27. Koo SS, Burkhart SS, Ochoa E. Arthroscopic double-pulley remplissage technique for engaging Hill-Sachs lesions in anterior shoulder instability repairs. Arthroscopy. 2009; 25(11):1343–1348.

28. Barlow B, Peace W, Metzger PK, Leonardelli D, Solomon DJ. Clinical grading of Hill-Sachs injuries: association with glenoid bone loss and clinical application of the "glenoid track" concept: when is there humeral head engagement? In : Proceedings of the American Orthopaedic Society for Sports Medicine 2010 Annual Meeting; 2010 Jul 15-18; Providence, RI. Rosemont, IL: American Orthopaedic Society for Sports Medicine;2010.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download