Abstract
Background
Some studies have shown significant functional improvement after rotator cuff (RC) repair in elderly patients. However, few studies have reported the healing potential of RC tears in elderly patients.
Methods
Twenty-five patients aged ≥ 75 years who underwent RC repair were enrolled. The mean age at the time of surgery was 78.3 years (range, 75 to 88 years) while the mean follow-up was 36.3 months (range, 18 to 114 months). We evaluated clinical and structural outcomes after RC repair in the retear and healed groups.
Results
Of 25 patients, 16 (64%) had healed RC lesions and 9 (36%) had retorn cuff lesions. The retear rate increased significantly with increasing initial tear size (small to medium, 13%; large, 60%; massive, 80%; p = 0.024) but not with increasing age (p = 0.072). The mean visual analog scale (VAS), University of California Los Angeles (UCLA), and Constant scores significantly improved from 5.2, 15.8, and 49.3 preoperatively to 1.4, 31.1, and 71.9 in the healed group and from 6.0, 14.4, and 39.5 preoperatively to 2.4, 28.3, and 63.6 in the retear group at the final follow-up (p < 0.05, respectively). There were no significant differences in clinical outcomes between the 2 groups at the final follow-up. Retear was significantly correlated with initial tear size (p = 0.001; odds ratio [OR], 2.771; 95% confidence interval [CI], 1.394 to 5.509 for large to massive tears) (p = 0.001; OR, 0.183; 95% CI, 0.048 to 0.692 for small to medium tears).
Conclusions
There were significant improvements in clinical outcomes after RC repair in patients ≥ 75 years. Structural integrity after cuff repair did not affect the final clinical outcome. Even in elderly patients aged ≥ 75 years, healing of repaired RC can be expected in cases of small to medium tears. Although the retear rate was relatively high for large to massive tears, clinical outcomes still showed significant improvement.
The incidence of rotator cuff tears (RCT) increases with age and tends to occur as part of the degenerative process of aging.12) Studies have reported the prevalence of full-thickness RCT of 28% in patients ≥ 60 years old, 50% in those ≥ 70 years, and 80% in those ≥ 80 years.345) Fifty percent of asymptomatic RCT become symptomatic at a mean of 2.8 years after diagnosis.6) Furthermore, untreated RCT size may increase over time with subsequent tendon retraction and irreversible muscle atrophy.78)
The incidence of RCT increases with age, but the effectiveness and healing potential of cuff repair in elderly patients remains controversial for several reasons. Elderly patients are more likely to have osteoporosis of the greater tuberosity, which may significantly complicate suture anchor fixation, resulting in reduced cellular activity and poorer potential for healing.4) Those aged ≥ 65 years have a larger tear size, which is associated with greater tendon degeneration and potentially increased repair difficulty.1) Elderly patients frequently have comorbidities that may weaken the healing response and complicate surgical management.9) They also tend to have more medical problems and shoulder dysfunction, which are associated with a compromise in an individual's health status similar to that seen in major medical diseases such as congestive heart failure, acute myocardial infarction, and diabetes mellitus.10) These factors can have a negative influence on the healing process of the repaired tendon. Studies have clearly demonstrated that rotator cuff healing failure leads to poorer functional outcome, particularly strength, as well as a decrease in the healing rate related to advanced age and greater rotator cuff degeneration.3111213)
In contrast, successful rotator cuff repair in elderly patients with RCT have been reported.14) Grondel et al.14) reported the effectiveness of rotator cuff repair in an older population, with good or excellent results in 84 of 97 shoulders (87%). Their results indicated that elderly patients continued to improve in function and strength for > 12 months after RC repair with decreased activity and the age of the patient did not appear to be a contributing factor to a successful result. In addition, some elderly patients with RCT desire to remain physically active with high functional demands. Surgeons often consider surgical repair for these patients when severe persistent pain and disability of the shoulder is nonresponsive to conservative treatment. However, a limited number of studies have reported the healing potential of repaired RCT in elderly patients.
The purpose of this study was to evaluate the clinical and structural outcomes of elderly patients aged ≥ 75 years who underwent arthroscopic or open repair of a full-thickness RCT and determine the factors associated with clinical outcome and retear. We hypothesized that rotator cuff repair in elderly patients ≥ 75 years would show inferior clinical outcomes due to the low healing potential and high retear rate of repaired rotator cuff lesions in this age group.
This study was retrospective in nature. The Kyung Hee University Medical Center Institutional Review Board approved the study and informed consent requirement was waived (KMC IRB 1508–08).
From March 2003 to July 2013, 59 consecutive patients aged ≥ 75 years underwent arthroscopic or open rotator cuff repair for the treatment of full-thickness RCT that were diagnosed primarily by physical examination and preoperative magnetic resonance imaging (MRI) and confirmed by arthroscopic findings. RCT sizes were measured intraoperatively according to the classification of DeOrio and Cofield15) by assessing the anteroposterior dimension with the use of a calibrated probe introduced through the posterior portal with a view from the lateral portal. The tear sizes were categorized into small (< 1 cm), medium (1–3 cm), large (3–5 cm), and massive (> 5 cm). Patients who had acromioclavicular arthritis that required distal clavicle resection, advanced glenohumeral arthritis, RCT with a Workers' Compensation claim, incomplete medical record, or no postoperative follow-up MRI at least 12 months after surgery were excluded from the study. Patients undergoing revision procedures were also excluded. A total of 25 patients (4 male, 21 female mean age at surgery, 78.3 years [range, 75 to 88 years]; mean follow-up, 36.3 months [range, 18 to 114 months]) who were available for postoperative MRI evaluation at least 12 months after rotator cuff repair were enrolled in this study.
Patients were considered surgical candidates if they had persistent shoulder pain that was unresponsive to at least 6 months of adequate conservative treatments such as anti-inflammatory medication, physical therapy, subacromial corticosteroid injection, and activity modification. Arthroscopic repair was performed when the tears could be repaired without undue tension based on arthroscopic findings. A double-row repair with a suture-bridge technique was used for medium to large tears, while a single-row repair was used for small tears and for massive tears that could be repaired with full coverage of the footprint. Open repair was indicated when: (1) a tear was arthroscopically irreparable because of severe retraction of the tendon; (2) tendon tissue quality was poor; or (3) pullout strength of the anchor was considered weak with accompanying osteoporosis of the greater tuberosity. Repairability was determined based on preoperative MRI. In case of open repair, retraced cuff was mobilized after a full release of proximal region, in which repair was performed by using suture anchor or transosseous suture. The decision to operate on the patient was made by the senior author based on the patient's history, clinical findings, failed conservative management, and persistent pain. All operations were performed by the single senior author with the patient in a beach chair position.
All patients followed a standard postoperative rehabilitation program. From the day of operation, passive exercises including pendulum exercise, passive forward flexion and external rotation exercises were performed. Active exercises were not allowed until postoperative 6th week or until regaining full passive range of motion (ROM). Active assisted exercises were started at postoperative 6th week and muscle strengthening exercises were introduced gradually thereafter.
All patients underwent a physical examination 1 day before the operation. Postoperative evaluations were performed at 3, 6, 9, and 12 months and annually on an outpatient basis, and the results of the last follow-up were analyzed. Postoperative subjective pain scores at rest and during active shoulder motion were measured on the visual analog scale (VAS). Quantitative muscle strength measurements of the rotator cuff were assessed using a portable handheld Nottingham Mecmesin Myometer (Mecmesin Co., Nottingham, UK). Elevation strength was tested with the patient in the seated position with the arm flexed to 90° in the scapular plane. External and internal rotation was tested with the shoulder in a neutral position and the elbow in 90° of flexion. For shoulder ROM, active forward flexion, external rotation at the side, internal rotation to the posterior, and abduction were assessed preand postoperatively. Internal rotation to the posterior was measured at the vertebral level of the hand. The Constant score16) and the Shoulder Rating Scale of the University of California at Los Angeles (UCLA)17) were used for the clinical assessment.
To assess rotator cuff repair integrity, an anatomical evaluation of the cuff repair was done using MRI as the modality of choice because it allows for multiplanar imaging of the shoulder postoperatively.18) Postoperative MRI was performed on all patients at least 12 month postoperative. All studies were obtained with a 3.0-T MRI using routine pulse sequences. All images were reviewed by an experienced senior radiologist. Integrity failure was assessed on MRI according to established MRI criteria;18) and when a fluid-equivalent signal or non-visualization of the supraspinatus, infraspinatus, or subscapularis tendon was found on at least 1 T2-weighted or proton density-weighted image, the diagnosis of a full-thickness retear or anatomical healing failure was made. We classified the integrity of the tendon into 2 categories with MRI: (1) healed (types I and II) and (2) retear (types III–V) on oblique coronal and oblique sagittal views according to Sugaya classification.19)
The Wilcoxon rank sum test was performed to assess the difference between the preoperative and postoperative results. Comparisons between the 2 groups (healed and retear group) were performed using the Mann-Whitney U-test and the chi-square test for comparing proportions between groups. Correlation analysis using Fisher exact test was used to identify the correlation between various shoulder-specific functional outcome instruments at final follow-up. Significance was set at a level of 0.05 with associated 95% confidence intervals. The IBM SPSS ver 20.0 (IBM Co., Armonk, NY, USA) was used for all the statistical analyses.
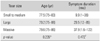
All patients included in this study were normal healthy patients or patients with mild systemic disease without functional limitation who could be controlled by medication. A total of 15 small to medium tears (60%), 5 large tears (20%), and 5 massive tears (20%) were examined in the current study. Nineteen patients (76%) underwent arthroscopic repair (14 small to medium tears, 2 large tears, and 3 massive tears) and 6 (24%) underwent open repair (1 medium tear, 3 large tears, and 2 massive tears). Among the arthroscopic repairs, single-row repair was performed in 13 cases (52%) and suture-bridge repair in 6 cases (24%) (Table 1).
The mean patient age was 77.5 years (range, 75 to 83 years) for the small to medium tear group, 79.2 years (range, 75 to 88 years) for the large tear group, and 79.6 years (range, 75 to 86 years) for the massive tear group. Larger tear size was correlated with increased mean age, but the association was not significant (p = 0.235). The mean symptom duration was 9.9 months (range, 1 to 36 months) for the small to medium tear group, 29.5 months (range, 12 to 85 months) for the large tear group, and 37.9 months (range, 1.6 to 122 months) for the massive tear group. Larger tear size was correlated with longer mean symptom duration, but the association was insignificant (p = 0.472) (Table 2).
The mean VAS of the entire patient cohort improved significantly from 5.4 ± 1.5 (range, 3 to 8) preoperatively to 1.8 ± 1.4 (range, 0 to 6) at the final follow-up (p < 0.001). In the retear group, the mean VAS improved significantly from 6.0 ± 1.1 (range, 4 to 7) preoperatively to 2.4 ± 1.8 (range, 0 to 6) at the final follow-up (p < 0.001). In the healed group, it improved from 5.2 ± 1.6 (range, 3 to 8) preoperatively to 1.4 ± 0.9 (range, 0 to 3) at the final follow-up (p = 0.011). There was no significant difference in the postoperative VAS values between the 2 groups (p = 0.934) (Table 3).
The mean preoperative ROM of the entire patient cohort for active forward flexion (aFF), external rotation at the side (ERs), internal rotation to the posterior (IRp), and abduction (Abd) improved from 130°, 55°, T12, and 128° to 146°, 46°, T11, and 133° at the final follow-up, respectively. The postoperative improvement of aFF was statistically significant (p = 0.038), but there were no significant differences in postoperative ROM of ERs, IRp, or Abd (p = 0.052, 0.443, and 0.952, respectively).
In the retear group, the mean preoperative ROM values for aFF, ERs, IRp, and Abd were 117°, 58°, T12, and 136°, respectively. At the final follow-up, the mean ROM values were 141°, 51°, T11, and 123° (p = 0.037, p = 0.398, p = 0.261, and p = 0.078, respectively). In the healed group, the mean ROM for aFF, ERs, IRp, and Abd improved from 137°, 53°, T12, and 124° to 149°, 44°, T11, and 138° (p = 0.049, p = 0.072, p = 0.944, and p = 0.360, respectively) at the final follow-up. The postoperative improvement in aFF in both groups was statistically significant, but there were no significant differences in postoperative ROM values of aFF, ERs, IRp, and Abd between the 2 groups (Table 3).
The mean muscle strength of the entire patient cohort for forward flexion (FF), external rotation (ER), internal rotation (IR), and Abd improved from the preoperative mean of 4.3, 5.0, 6.0, and 4.2 kg to 6.2, 6.9, 8.1, and 5.9 kg at the final follow-up (p = 0.020, p = 0.023, p = 0.008, and p = 0.001, respectively).
In the retear group, the mean muscle strength of FF, ER, IR, and Abd improved slightly but not significantly (p = 0.260, p = 0.214, p = 0.314, and p = 0.139, respectively). On the other hand, in the healed group, postoperative improvement in muscle strength in all directions was significant (p = 0.049, p = 0.044, p = 0.015, and p = 0.002, respectively). The postoperative values between the 2 groups did not show significant differences (p = 0.419, p = 0.388, p = 0.301, and p = 0.890, respectively) (Table 3).
The mean UCLA score increased from 15.3 points (range, 9 to 23 points) preoperatively to 31.9 points (range, 21 to 33 points) at the final follow-up (p < 0.001). The mean Constant score increased from 45.8 points (range, 18 to 62 points) preoperatively to 68.9 points (range, 43 to 80 points) at the final follow-up (p < 0.001).
In the retear group, the mean UCLA score improved from 14.4 (range, 9 to 23) preoperatively to 28.3 (range, 21 to 35) at the final follow-up (p = 0.008). Similarly, it improved from 15.8 (range, 10 to 23) preoperatively to 31.1 (range, 26 to 33) at the final follow-up in the healed group (p = 0.008). The mean Constant score increased from 39.5 (range, 18 to 59) preoperatively to 63.6 (range, 55 to 76) at the final follow-up in the retear group (p < 0.001) and from 49.3 (range, 27 to 62) preoperatively to 71.9 (range, 61 to 80) at the final follow-up in the healed group (p = 0.008). The pre- and postoperative clinical scores of the retear group were inferior to those of the healed group, but there was no significant difference in the UCLA and Constant scores between the 2 groups at the final follow-up (p = 0.388 and p = 0.677, respectively) (Table 3).
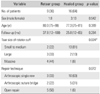
There were 9 patients (36%) in the retear group. The mean age at surgery was 77.3 years (range, 75 to 81 years) for the healed group and 80.0 years for the retear group (range, 75 to 88 years). The mean age at surgery was lower in the healed group, but the difference was insignificant (p = 0.389). There were 2 small to medium tears, 3 large tears, and 4 massive tears in the retear group, as compared with 13, 2, and 1 in the healed group (p = 0.024). There were no significant differences in sex composition, mean follow-up period, or repair technique between the 2 groups (p = 0.542, p = 0.284, and p = 0.072, respectively), but there was a significant difference in initial tear size (p = 0.024, respectively) (Table 4).
Retear was significantly correlated with initial tear size (p = 0.001; odds ratio [OR], 2.771; 95% confidence interval [CI], 1.394 to 5.509 for large to massive tears) (p = 0.001; OR, 0.183; 95% CI, 0.048 to 0.692 for small to medium tears) but not with age (p = 0.177) or sex (p = 1.000; OR, 0.542; 95% CI, 0.048 to 6.144).
RCT have little inherent capacity to heal without operative treatment.78) The surgical repair of RCT in young active patients is a widely accepted therapeutic option. Many studies have shown significant functional improvement and favorable tendon healing after rotator cuff repair.1119) However, there is insufficient evidence to suggest efficacy of operative treatment for RCT in elderly patients.13) In most cases, the first choice remains conservative management, but surgical treatment should be considered for symptomatic rotator cuff lesions that are unresponsive to conservative care. Whether debridement or repair should be considered in elderly patients is still unclear. Several studies have suggested that only subacromial decompression with acromioplasty should be performed in elderly subjects with RCT.20) Acromioplasty alone yields satisfactory short-term results after RCT treatment.21) However, deterioration is subsequently observed over the course of several years.22)
Many studies have reported improved clinical outcomes after rotator cuff repair in elderly patients. Flurin et al.23) reported improvement from a preoperative Constant score of 44 to 76 postoperatively and an American Shoulder and Elbow Surgeons (ASES) score of 35 to 54 postoperatively at 1 year of follow-up in patients ≥ 70 years of age. Robinson et al.24) evaluated the arthroscopic rotator cuff repair of 68 patients ≥ 70 years of age. They reported an improved Constant score from 23 preoperatively to 58 at the final follow-up in patients ≥ 70 years of age. Verma et al.9) evaluated 39 shoulders in patients ≥ 70 years undergoing arthroscopic repair of RCT. They reported that the ASES score improved from 45.8 to 87.5 and that the VAS score improved from 4.6 to 0.5 at final follow-up. Worland et al.25) studied 69 open rotator cuff repairs in patients aged ≥ 70 years. Satisfactory UCLA scores were achieved in 78%. Similarly, the findings of our study showed that the VAS, UCLA, and Constant scores plus muscle strength improved significantly after rotator cuff repair.
Although successful results after cuff repair have been reported, others reported that age and initial tear size are a negative factor associated with poorer tendon healing. Charousset et al.12) reported healing in 52% of patients aged ≥ 65 years. Boileau et al.11) found that patients aged ≥ 65 years had only a 43% chance of tendon healing and patients ≥ 65 years with delamination of the subscapularis or the infraspinatus had an even lower rate of healing. Liu and Baker26) reported a retear rate of 32% and that tear size at the time of the repair was a major determinant of cuff integrity after repair. Cole et al.27) reported a retear rate of 22% in 47 patients and showed that the presence of a recurrent tear was significantly correlated with patient age and initial tear size. In the current study, the retear rate was 36% of 25 patients and the cuff lesion healing rate in elderly patients with a mean age of 78.3 years was 64% (16 patients). In addition, among the 9 patients with retears, most (7 patients; 78%) had large to massive initial tears, while the healing rate in elderly patients with small to medium initial tears (15 patients) was 87%. These results are similar to the previously reported healing rate of 78%–88% in patients aged ≤ 60 years.2728) The mean age at surgery was 77.3 years (range, 75 to 81 years) for the healed group and 80.0 years for the retear group; hence, the mean age of the retear group was higher, as compared to that of the healed group, but without significance. The initial tear size was the only factor affecting the retear rate.
Klepps et al.29) reported that postoperative cuff integrity did not have a significant effect on outcome, as compared with intact cuffs in 32 patients. Another report suggested that rotator cuff repair significantly decreased pain and improved function and strength, despite repair failure on MRI.28) They also reported that patients with a retear still showed significant improvement in all clinical assessments, including strength.28) Liu and Baker26) also demonstrated that repair integrity did not influence functional outcome. On the contrary, Flurin et al.23) reported that retorn cuffs had worse overall Constant and ASES scores. Cole et al.27) reported that ROM and muscle strength in aFF were inversely correlated with a recurrent tear. Yoo et al.30) reported that physical component summaries of the Short Form-36 as well as on the UCLA and ASES were significantly higher in the healed group, even though there was no significant difference in mental component summary scores. Thus, controversy persists about whether structural repair integrity affects functional outcome. In the current study, there was no significant difference in Constant and UCLA score, ROM, and muscle strength at the final follow-up between the retear and healed groups. It is likely that structural integrity after cuff repair did not affect clinical outcome.
The current study had a few limitations. First, we analyzed short-term results with a mean follow-up of 30 months. Further long term follow-up studies with larger groups of patients are needed. However, our study provides valuable information about clinical outcomes and structural integrity after rotator cuff repair in patients aged ≥ 75 years. Second, with regard to postoperative imaging evaluation, the postoperative repair integrity was not analyzed by arthrography, but images were obtained for all included patients by MRI at a minimum of 12 months postoperatively. We did not measure the retear size or tendon retraction. However, partial-thickness tears or those with 50% of the normal rotator cuff thickness as documented by MRI were defined as retears to reduce the false-positive results rate in the present study. Third, the patient groups were heterogeneous regarding operative technique (arthroscopic or open repair procedures). Open repair was performed when arthroscopic repair was considered extremely challenging or rotator cuff tendon tissue or bone quality was poor. This selection bias may have contributed to the higher retear rate in the open repair group. In addition, the data of the patients' medical comorbidities were not described. Finally, our study had limitations similar to other retrospective studies. Nevertheless, it also had several strengths. First, all surgeries were performed by 1 senior author. Second, there are currently only a few published articles on the evaluation of clinical and anatomical results in elderly patients. And finally, we focused only on elderly patients and subdivided them into the retear and healed groups for comparison.
In conclusion, we demonstrated significant improvements in clinical outcomes after rotator cuff repair in patients aged ≥ 75 years. Structural integrity after rotator cuff repair did not affect final clinical outcome. Even in elderly patients aged ≥ 75 years, high healing rate of a repaired RCT over 85% was shown in cases of small to medium tears. Although the retear rate was relatively high for large to massive tears, clinical outcomes were still significantly improved. Therefore, healing potential can be expected in elderly patients aged ≥ 75 years who have RCT and in whom surgical repair can be attempted.
Figures and Tables
Table 1
Patient Demographics

Table 2
The Mean Age and Duration of Symptoms according to the Tear Size of Rotator Cuff
| Tear size | Age (yr) | Symptom duration (mo) |
|---|---|---|
| Small to medium | 77.5 (75–83) | 9.9 (1–36) |
| Large | 79.2 (75–88) | 29.5 (12–85) |
| Massive | 79.6 (75–86) | 37.9 (1.6–122) |
| p-value | 0.235* | 0.472† |
Table 3
Clinical Outcomes of Patients in Retear Group and Healed Group
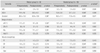
Values are presented as mean ± standard deviation.
VAS: visual analogue scale for pain, UCLA: University of California at Los Angeles shoulder score, Constant: Constant score, aFF: active forward flexion, ERs: external rotation at side, IRp: internal rotation to the posterior, Abd: abduction, FF: forward flexion, ER: external rotation, IR: internal rotation.
*Differences in postoperative values between the 2 groups. †Statistically significant (p < 0.05).
Table 4
The Influencing Factors in Retear and Healed Groups
References
1. Hattrup SJ. Rotator cuff repair: relevance of patient age. J Shoulder Elbow Surg. 1995; 4(2):95–100.

2. Rhee YG, Cho NS, Yoo JH. Clinical outcome and repair integrity after rotator cuff repair in patients older than 70 years versus patients younger than 70 years. Arthroscopy. 2014; 30(5):546–554.

3. Fehringer EV, Sun J, VanOeveren LS, Keller BK, Matsen FA 3rd. Full-thickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elbow Surg. 2008; 17(6):881–885.

5. Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999; 8(4):296–299.

6. Yamaguchi K. Mini-open rotator cuff repair: an updated perspective. Instr Course Lect. 2001; 50:53–61.
7. Gerber C, Meyer DC, Schneeberger AG, Hoppeler H, von Rechenberg B. Effect of tendon release and delayed repair on the structure of the muscles of the rotator cuff: an experimental study in sheep. J Bone Joint Surg Am. 2004; 86(9):1973–1982.

8. Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001; 10(3):199–203.

9. Verma NN, Bhatia S, Baker CL 3rd, et al. Outcomes of arthroscopic rotator cuff repair in patients aged 70 years or older. Arthroscopy. 2010; 26(10):1273–1280.

10. Gartsman GM, Brinker MR, Khan M. Early effectiveness of arthroscopic repair for full-thickness tears of the rotator cuff: an outcome analysis. J Bone Joint Surg Am. 1998; 80(1):33–40.

11. Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005; 87(6):1229–1240.

12. Charousset C, Bellaiche L, Kalra K, Petrover D. Arthroscopic repair of full-thickness rotator cuff tears: is there tendon healing in patients aged 65 years or older? Arthroscopy. 2010; 26(3):302–309.

13. Downie BK, Miller BS. Treatment of rotator cuff tears in older individuals: a systematic review. J Shoulder Elbow Surg. 2012; 21(9):1255–1261.

14. Grondel RJ, Savoie FH 3rd, Field LD. Rotator cuff repairs in patients 62 years of age or older. J Shoulder Elbow Surg. 2001; 10(2):97–99.

15. DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984; 66(4):563–567.

16. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987; (214):160–164.

17. Ellman H, Hanker G, Bayer M. Repair of the rotator cuff: end-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986; 68(8):1136–1144.

18. Magee TH, Gaenslen ES, Seitz R, Hinson GA, Wetzel LH. MR imaging of the shoulder after surgery. AJR Am J Roentgenol. 1997; 168(4):925–928.

19. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am. 2007; 89(5):953–960.

20. Kempf JF, Gleyze P, Bonnomet F, et al. A multicenter study of 210 rotator cuff tears treated by arthroscopic acromioplasty. Arthroscopy. 1999; 15(1):56–66.

21. Rockwood CA, Lyons FR. Shoulder impingement syndrome: diagnosis, radiographic evaluation, and treatment with a modified Neer acromioplasty. J Bone Joint Surg Am. 1993; 75(3):409–424.
22. Zvijac JE, Levy HJ, Lemak LJ. Arthroscopic subacromial decompression in the treatment of full thickness rotator cuff tears: a 3- to 6-year follow-up. Arthroscopy. 1994; 10(5):518–523.

23. Flurin PH, Hardy P, Abadie P, et al. Arthroscopic repair of the rotator cuff: prospective study of tendon healing after 70 years of age in 145 patients. Orthop Traumatol Surg Res. 2013; 99:8 Suppl. S379–S384.
24. Robinson PM, Wilson J, Dalal S, Parker RA, Norburn P, Roy BR. Rotator cuff repair in patients over 70 years of age: early outcomes and risk factors associated with re-tear. Bone Joint J. 2013; 95(2):199–205.
25. Worland RL, Arredondo J, Angles F, Lopez-Jimenez F. Repair of massive rotator cuff tears in patients older than 70 years. J Shoulder Elbow Surg. 1999; 8(1):26–30.

26. Liu SH, Baker CL. Arthroscopically assisted rotator cuff repair: correlation of functional results with integrity of the cuff. Arthroscopy. 1994; 10(1):54–60.

27. Cole BJ, McCarty LP 3rd, Kang RW, Alford W, Lewis PB, Hayden JK. Arthroscopic rotator cuff repair: prospective functional outcome and repair integrity at minimum 2-year follow-up. J Shoulder Elbow Surg. 2007; 16(5):579–585.

28. Cho NS, Rhee YG. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg. 2009; 1(2):96–104.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download