Abstract
Background
Shoichi Kokubun introduced his successful experience with local anesthetic injection at the occipital insertion of the sternocleidomastoid muscle in K-point syndrome. The purpose of this study was to evaluate the short-term and long-term effectiveness of K-point injection and investigate factors affecting treatment results.
Methods
K-point injection was performed in 58 patients with K-point syndrome at Yeungnam University Medical Center. The syndrome was associated with cervical whiplash injury in 10 patients and was of nonspecific origin in the rest. One milliliter of 2% lidocaine mixed with 1 milliliter of dexamethasone was injected in 50 patients and 2 milliliters of 1% lidocaine alone in the rest. Initially, the severity of local tenderness at the K-point and other tender points was examined and the degree of immediate pain relief effect was assessed within 1 hour after injection. Early effect within 1 month after the injection and current effect were evaluated in 27 patients using a modified Kim's questionnaire with regard to the duration of improvement, degree of improvement in pain and daily living activities, and satisfaction.
Results
Of the total 58 patients, 44 (75.8%) apparently had immediate pain relief after K-point injection. The only factor associated with successful immediate pain relief was the whiplash injury associated with traffic accident (TA). The early pain control effect was associated with the immediate effect. The current effect was associated with the early effect alone. Satisfaction with the K-point injection was related to early successful pain relief.
Disc herniation, spinal stenosis, and facet syndrome have been clearly identified as the pathological causes of chronic neck pain. However, in case the cause of chronic neck pain is not detected, pain management can be especially challenging for both patient and physician. Nonspecific pain in multiple sites including the cervical spine is a major complaint among patients with myofascial syndrome, fibromyalgia, Barré-Liéou syndrome, and whiplash injury. Evan after an appropriate treatment, these conditions sometimes progress for over 6 months and develop into chronic neuromuscular pain. Patients with nonspecific pain syndrome present with not only neck pain but also multiple pain in various sites and central nervous system (CNS) as patients who suffer from somatoform disorders.1) This is why there have been a diversity of suggestions regarding the diagnostic criteria and treatment methods. Nowadays, efforts have been made to establish diagnostic criteria for fibromyalgia; however, there are no universal criteria for the other pain syndromes to evaluate the efficacy of treatment methods, except for the trigger point injection or nerve root block for symptom relief.2)
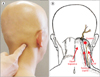
Recently, Shoichi Kokubun referred to the area of cranial musculotendinous junction on the cleido-occipital head of the sternocleidomastoid (SCM) muscle as "K-point" and introduced K-point syndrome that can be characterized primarily by musculotendinous junction pain, followed by tenderness at muscle ends, squeezing pain at muscle bellies, and stretching pain on the related muscle group. Local injection of anesthetics at the K-point was reported to result in successful pain relief in the study. We could also experience successful results with K-point injection using local anesthetics with or without steroid in patients diagnosed with K-point syndrome.
In this study, we assessed the clinical efficacy of K-point injection based on the short-term and long-term clinical evaluation and investigated factors associated with successful results.
Of the 71 patients who were treated for K-point syndrome at our institution and followed from January 2009 to December 2013 on an outpatient basis, 58 patients who received a K-point injection for treatment were enrolled in this study. There were 28 males and 30 females with a mean age of 53.9 years (range, 22 to 78 years). The condition was related to whiplash injury in 10 patients and primary idiopathic syndrome in the rest.
According to the Kokubun's criteria, K-point syndrome was diagnosed in patients with a chief complaint of neck pain if tenderness and squeezing pain were present at the musculotendinous junction of both upper and lower limbs as well as at the K-point at the cranial insertion of the cleido-occipital head of the SCM. A mixture of 1 mL of 2% lidocaine and 1 mL of dexamethasone was injected at the K-point except in 8 diabetics who received 2 mL of 1% lidocaine alone (Fig. 1).
We reviewed the clinical chart describing the patient's age, gender, chief complaint, past medical history, whether the K-point pain was bilateral, the distribution of multiple tenderness sites in the upper and lower extremities, and the severity of pain. The following muscles are known as associated muscle groups of K-point syndrome: the pectoralis minor muscle, the 1st dorsal part of the interosseous muscle of the hand, the 1st rib interosseous muscle, infraspinatus muscle, and the 1st dorsal part of the interosseous muscle of the foot. The severity of tenderness of these muscles was rated as none, light, moderate, and severe, respectively. The degree of immediate pain relief assessed within 1 hour after K-point injection was classified as follows: no effect (no pain relief), unclear (ambiguous pain relief), clear (partial pain relief), and dramatic (complete pain relief). The clinical chart was also reviewed to assess the patient's general condition, steroid use, severity and distribution of muscle pain in the upper and lower extremities. Correlations of these parameters were investigated in statistical analysis.
A telephone survey was conducted using Kim's questionnaire introduced in the Journal of Korean Society of Spine Surgery,3) and 27 of the 58 patients answered the questionnaire in the survey. In advance of the survey, we modified the original questionnaire to meet the purpose of this study. The modified questionnaire included questions such as the degree of early pain relief at < 1 month and final current pain relief at ≥ 1 year after K-point injection, improvement of daily living activity performance, satisfaction with the injection, and intent of retrial for a recurrent pain (Table 1).
Statistical analysis was performed using SPSS ver. 18 (SPSS Inc., Chicago, IL, USA). Correlation between immediate pain relief after K-point injection and traffic accident (TA) was assessed with chi-square test. Correlation between immediate pain relief after K-point injection and the answers of the questionnaire was investigated through cross analysis. Fisher exact test and chi-square test were used to identify differences between groups divided according to the cause (nonspecific cause vs. TA-related). A multiple regression analysis was conducted to evaluate correlations among improvement of ability to perform daily living activities, pain relief, satisfaction, and intent of retrial of K-point injection.
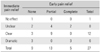
The immediate pain relief after K-point injection was rated as no effect in 1, unclear in 13, clear in 24, and dramatic in 20 of all 58 patients; therefore, 44 of 58 patients (75.8%) apparently had immediate pain relief after K-point injection (Table 2). In the group where the condition was associated with TA, 7 of 10 patients apparently had immediate pain relief after K-point injection and the other 3 showed dramatic improvement. Patients with TA-related K-point syndrome better responded to the K-point injection than the other patients with nonspecific causes. With regard to the patient's satisfaction and need for repeated injection, there was no statistically significant difference between groups; however, the regression analysis on factors related to immediate pain relief showed the group with TA-related syndrome obtained more satisfactory immediate pain relief (p = 0.007).
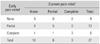
According to the telephone survey, 18 of 27 respondents answered they had early pain relief at 1 month after K-point injection and 5 patients responded complete pain relief, whereas 9 patients answered they had no experience of early pain relief. One patient reported that there was neither early pain relief nor immediate pain relief after injection. Two of 8 with unclear efficacy immediately after K-point injection answered no to the question of early pain relief, 4 of 8 answered they had partial early pain relief, and the other 2 answered they had complete early pain relief. Three of 12 with clear efficacy immediately after K-point injection answered they had temporary pain relief without early pain relief and the other 9 answered they had partial early pain relief. Three of 6 with dramatic efficacy immediately after K-point injection soon experienced recurrence of the pain without early pain relief, but the other 3 answered they had complete early pain relief (p = 0.010) (Table 3).
At the final follow-up, 9 patients with no early pain relief after K-point injection showed no current pain relief. Also, 3 of 5 patients with complete early pain relief reported complete current pain relief (p = 0.001) (Table 4).
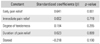
According to the results of the stepwise method of multiple linear regression analysis, current pain relief was related to early pain relief only (p = 0.001). The degree of tenderness, duration of pain relief, immediate pain relief, steroid use, and others were not statistically significant factors (Table 5). Patients with no effect in early pain relief tended to show no current pain relief, and patients with early pain relief in 1 month after injection tended to show pain relief in the long-term. Also, there was no correlation between steroid use and pain relief, which seems to allow repeated use of local anesthetics.
Since the introduction of Kokubun's K-point injection at the Congress of the Korean Orthopedic Association in 2012 and 2015, many Korean orthopedic surgeons have experienced successful results with adaptations of the procedure advantageous for its simplicity and cost-effectiveness. However, K-point syndrome has not been fully understood in terms of its pathomechanism, diagnostic criteria, and treatment. Furthermore, the efficacy of K-point injection has not been well established.
Barré-Liéou syndrome was characterized by ischemic symptoms such as tinnitus, dizziness, and pain in the head and cervical region caused by pressure on the sympathetic nervous system. Some insist that Barré-Liéou syndrome is not an appropriate diagnostic name, because it can be observed when the vestibular organ has a problem even though the name has historical meaning.45) Recently, cervicogenic headache has been defined as headache originating from the cervical spine accompanying sympathetic nervous system symptoms and vomiting. A diagnosis of cervicogenic headache can be confirmed by disappearance of such symptoms with blockage of a suspicious lesion; however, practical diagnostic criteria have yet to be established.67) In 1949, Jackson8) found that compression of C2 and C3 nerve roots due to damage to the upper cervical spine could result in headache. This mechanism is believed to be the reason of pain in the head, cervical region, and upper and lower extremities after soft tissue damage in a whiplash injury. Several recent studies have reported successful results of C2 and C3 nerve root block in headache syndrome of the cervical region; however, the mechanism is still not obvious.9) Kokubun thought K-point syndrome as a kind of cervicogenic headache caused by aponeurosis inflammation of the SCM muscle. This was because the pain was relieved by injection of a local anesthetic into the cranial musculotendinous junction of the SCM muscle. So, Kokubun infer this syndrome from Barré-Liéou syndrome.
Tenderness on pinching of the 1st dorsal interosseous muscle of the hand was considered as a characteristic diagnostic feature of K-point syndrome. In this study, we could observe most patients had tenderness in the 1st dorsal interossei of the hands and a group of muscles related to the K-point in a variable pattern. Muscle stiffness on palpation of other muscles including the 1st dorsal interossei is partially similar to the symptom of myofascial pain syndrome (MPS) that has a sensitive response point known as the trigger point located in a strained striped taut band in the skeletal muscle.1011) Another disorder that has a similar symptom is fibromyalgia. It is a relatively subjective condition accompanied by fatigue, sleep disorder, cognitive and affective disorders without specific cause, and diffuse musculoskeletal pain. Fibromyalgia has tenderness points at specific regions, but there is no inflammation in the soft tissue.12) Both MPS and fibromyalgia do not have apparent causes and show diverse aspects, so it is difficult to develop objective diagnostic criteria. Efforts have been made to set objective standards by the American College of Rheumatology (ACR) in 1990 and 2010.13) Trigger point injection has been used as a representative method to improve MPS. In contrast, fibromyalgia pain might be relieved by physical therapy, antidepressant medication, cognitive behavioral therapy, or kinesiotherapy14) because it appears to result from dysfunction of the CNS and the muscular tenderness point is different from the trigger point.
In this study, K-point injection was quite effective in all cases related to the whiplash injury as was the trigger point injection in most MPS cases. Thus, the K-point could be considered as the primary active trigger point and the other regions of tenderness as the secondary latent trigger points, which means the local injection would be ineffective in fibromyalgia syndrome.1) However, the K-point syndrome of unknown origin showed 75.8% of immediate pain relief rate but only 28.3% of current pain relief rate. This might indicate K-point syndrome is similar to fibromyalgia that has a nonspecific cause. White introduced the concept of sub-injury as one of the causes of spinal instability. Although the injury at the soft tissue could not be detected by the conventional diagnostic method, it could provoke sustained high stress or strain on the soft tissue and joints according to his theory. In a whiplash injury, muscular spam due to such a sub-injury could be considered to be relieved by the K-point injection and the pain is thought to be controlled even if there is no spinal instability by trauma or structural abnormality.151617)
There are some limitations to this study. First, it is a retrospective exploratory study based on a survey of patients who visited the outpatient department of the institution of the authors. It was difficult to monitor the changes in pain and assess correlation among various variables. Second, the interpretation of medical records on pain level and efficacy immediately after the K-point injection could have been affected by the authors' subjective judgment. In addition, the survey was primarily dependent on the individual patients' memory. Third, the reliability of the results is limited; 58 of 71 patients received K-point injection and only 26 of them participated in the survey, and there was no control group in this study. This is just an exploratory study with such limitations. It is desired that a prospective randomized multicenter study needs to be conducted to assess the efficacy of K-point injection after classification according to clinical aspects.
In conclusion, K-point injection would be useful for early pain relief, but not for current pain relief, in the non-specific neck pain syndrome so called K-point syndrome. The method was especially effective for early pain control in whiplash injury related to TA.
Figures and Tables
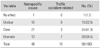
Table 1
Modified Kim's Questionnaire

Table 2
Distribution of Immediate Pain Relief after K-Point Injection
| Variable | Nonspecific cause | Traffic accident-related | No. (%) |
|---|---|---|---|
| No effect | 1 | 0 | 1 (1.7) |
| Unclear | 13 | 0 | 13 (22.5) |
| Clear | 21 | 3 | 24 (41.3) |
| Dramatic | 13 | 7 | 20 (34.5) |
| Total | 48 | 10 | 58 (100) |
Table 3
Distribution of Early Pain Relief and Immediate Pain Relief after K-Point Injection
| Immediate pain relief | Early pain relief | |||
|---|---|---|---|---|
| None | Partial | Complete | Total | |
| No effect | 1 | 0 | 0 | 1 |
| Unclear | 2 | 4 | 2 | 8 |
| Clear | 3 | 9 | 0 | 12 |
| Dramatic | 3 | 0 | 3 | 6 |
| Total | 9 | 13 | 5 | 27 |
Table 4
Distribution of Current Pain Relief and Early Pain Relief after K-Point Injection
| Early pain relief | Current pain relief | |||
|---|---|---|---|---|
| None | Partial | Complete | Total | |
| None | 9 | 0 | 0 | 9 |
| Partial | 8 | 5 | 0 | 13 |
| Complete | 1 | 1 | 3 | 5 |
| Total | 18 | 6 | 3 | 27 |
References
1. Staud R. Peripheral pain mechanisms in chronic widespread pain. Best Pract Res Clin Rheumatol. 2011; 25(2):155–164.

2. Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). 2010; 62(5):600–610.

3. Kim HS, Min HJ, Yoon US, Seo JS, Kim YJ, Jo SM. Efficacy of epidural steroid injection in lumbar spinal stenosis. J Korean Soc Spine Surg. 2005; 12(4):310–315.

4. Foster CA, Jabbour P. Barré-Lieou syndrome and the problem of the obsolete eponym. J Laryngol Otol. 2007; 121(7):680–683.

5. Longbottom J. A case report of postulated 'Barré Liéou syndrome'. Acupunct Med. 2005; 23(1):34–38.

6. Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol. 2009; 8(10):959–968.

7. Hong JP, Lai CH, Lin YC, Chou SW. Clinical assessment of patients with cervicogenic headache: a preliminary study. Chang Gung Med J. 2010; 33(1):58–66.
8. Jackson R. The classic: the cervical syndrome. 1949. Clin Orthop Relat Res. 2010; 468(7):1739–1745.
9. Panjabi MM. The stabilizing system of the spine. Part II: neutral zone and instability hypothesis. J Spinal Disord. 1992; 5(4):390–396.

10. Simons DG, Travell JG, Simons LS. Travell & Simons' myofascial pain and dysfunction: the trigger point manual. Volume 1: upper half of body. 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins;1999.
11. Giamberardino MA, Affaitati G, Fabrizio A, Costantini R. Myofascial pain syndromes and their evaluation. Best Pract Res Clin Rheumatol. 2011; 25(2):185–198.

12. Glass JM. Cognitive dysfunction in fibromyalgia and chronic fatigue syndrome: new trends and future directions. Curr Rheumatol Rep. 2006; 8(6):425–429.

13. Salaffi F, Sarzi-Puttini P. Old and new criteria for the classification and diagnosis of fibromyalgia: comparison and evaluation. Clin Exp Rheumatol. 2012; 30:6 Suppl 74. 3–9.
14. Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA. 2004; 292(19):2388–2395.

15. Herren-Gerber R, Weiss S, Arendt-Nielsen L, et al. Modulation of central hypersensitivity by nociceptive input in chronic pain after whiplash injury. Pain Med. 2004; 5(4):366–376.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download