Abstract
Background
We investigated the clinical results and early complications after lateral unicompartmental knee arthroplasty (UKA) using the Zimmer unicompartmental high-flex knee (ZUK) prosthesis with a minimum follow-up of 2 years.
Methods
Twenty-seven patients (30 cases) who underwent lateral UKA with the ZUK prosthesis between January 2011 and February 2014 were selected for this study. The mean age of the patients was 63.3 years at the time of surgery, and the mean followup was 3 years and 2 months (range, 24 to 48 months). A retrospective investigation method was used to evaluate the clinical and radiographic results with use of the Knee Society (KS) clinical rating system and plain radiography.
Results
The mean KS pain score was improved from 17.9 points (range, 10 to 30 points) preoperatively to 40.5 points (range, 30 to 45 points) at the final follow-up (p < 0.001). The mean KS knee score and function score significantly increased from 63.2 points (range, 48 to 70 points) and 68.6 points (range, 35 to 80 points), respectively, preoperatively to 86.0 points (range, 74 to 95 points) and 92.4 points (range, 60 to 100 points), respectively, at the final follow-up (p < 0.001). The mean range of motion of the knee was recovered from 127.1° (range, 110° to 135°) preoperatively to 131.6° (range, 120° to 135°) at the final follow-up. The mean tibiofemoral angle changed from 6.2° of valgus (range, 0.1° to 11.4° of valgus) preoperatively to 3.4°of valgus (range, 0.2° to 9.5° of valgus) at the final follow-up. The overall results classified based on the KS knee score were "excellent" in 21 cases and "good" in 8 cases. Revision total knee arthroplasty was required in one case because of consistent pain on the medial side of the knee after surgery.
Conclusions
The early clinical results of lateral UKA using the ZUK prosthesis were satisfactory for improvement of pain, knee score, function score, and recovery of knee motion. Therefore, the lateral UKA could be a useful method in the treatment of osteoarthritis in the lateral compartment of the knee. Long-term survivorship remains to be confirmed through ongoing follow-up.
Lateral unicompartmental osteoarthritis of the knee is rare compared to osteoarthritis of the medial compartment of the knee, and it is much more challenging to treat. Arthroscopy, osteotomy, lateral unicompartmental knee arthroplasty (UKA), and total knee arthroplasty (TKA) are surgical interventions currently available to treat lateral unicompartmental osteoarthritis. Of those, lateral UKA has some advantages such as rapid postoperative recovery, restoration of the joint function with preservation of the anatomical knee shape, and ease of future revision surgery.1) Arthroplasty of the lateral compartment of the knee is more difficult to perform than that of the medial compartment. The surgical approach is more difficult, and there are anatomical and technical differences as well. The lateral ligament is more lax than the medial ligament, and posterior movement of the lateral femoral condyle is deeper than that of the medial femoral condyle.2) Clinical results of lateral UKA have been known to be relatively unsuccessful compared to the those of medial UKA.234) However, it has been recently reported that careful selection of patients and appropriate use of the prosthesis can result in definite pain relief and better long-term survivorship of prosthesis.156)
Lateral UKA accounts for only 5%–10% of all UKAs, and reports on the outcomes of the procedure are scarce.23) The proportion of lateral unicompartmental osteoarthritis of the knee in Korea is relatively smaller than that in the West. So the cases of lateral UKA in Korea are very few, and, to our knowledge, there are no previous reports on lateral UKA on Korean patients. Based on clinical analysis, we intended to evaluate the clinical results and early complications of lateral UKA.
Thirty cases in 27 patients who had undergone lateral UKA between January 2011 and February 2014 were included in this study. A retrospective investigation method was used to evaluate changes in clinical and radiological results. Complications and prosthetic failure rate were analyzed. Thirteen patients (15 cases) were females and 14 patients (15 cases) were males. The mean age of the patients was 63.3 years with a range from 48 years to 80 years. The mean follow-up period was 3 years and 2 months (range, 24 to 48 months).
Osteoarthritis of the lateral compartment of the knee accompanied by pain and impaired mobility was selected as the main indication for lateral UKA. All included patients had Kellgren-Lawrence grade 3 or 4 degenerative changes and they were more than 48 years of age.
Other inclusion criteria included the absence of inflammatory diseases, normally functioning anterior and posterior cruciate ligaments, a valgus deformity of less than 15°, less than 10° of flexion contracture, and above 100° of range of motion of the knee. If a patient expressed no pain in the patellofemoral joint despite observable degenerative changes in the patellofemoral joint, the patient was selected as a subject.
Patients were excluded from the lateral UKA if preoperative evaluation revealed anterior/posterior instability or degenerative changes in the medial compartment. Additionally, patients with degenerative changes in the patellofemoral joint who expressed pain in the anterior region of the knee during ambulation on a flat surface or ascension of stairs were excluded.
The surgery was performed by 2 surgeons (KTK and SL) at a single institution. The fixed-type Zimmer unicompartmental high-flex knee (ZUK; Zimmer, Warsaw, IN, USA) prosthesis was used in all cases, using a minimally invasive procedure. The implants and instruments for the lateral UKA were the same as those for medial UKA.
A lateral short skin incision was made downward from the lateral portion of the proximal pole of the patella to 2 cm inferior to the joint line, and osteophytes were removed after checking the entire joint through the incision on the lateral joint capsule. An intramedullary femoral resection guide was inserted into the medullary canal and the appropriate resection angle predetermined with preoperative radiographs (4° or 6° in most cases) was selected. Resection of the distal femoral condyle was carried out after connection of the distal femoral resector block with the intramedullary femoral resection guide using a slotted holding pin. The aim of postoperative limb alignment was slight undercorrection of the valgus deformity. The extramedullary tibial resector assembly was fixed parallel to the tibial shaft, and the proximal portion of the lateral tibial condyle was resected vertically and horizontally. The level of horizontal saw cut was made 2 mm below the deepest portion of the tibia to reproduce the natural posterior slope, which is around 0° in the lateral compartment. A sagittal cut was aimed at 15°–20° of internal rotation to allow centralization of the tibial plateau under femoral condyle especially in flexion. Implants size was determined by femoral and tibial sizers. Using the femoral sizer/finishing guide, the posterior portion and chamfer of the distal femur were resected, and the anterior and posterior post holes were drilled. Two tibial peg holes were drilled after fixation of the tibial fixation provisional while the knee was flexed. With the femoral provisional and tibial articular provisional inserted, the fit of the provisional components was examined and soft tissue tension in flexion and extension was evaluated using a tension gauge. The thickness of the prosthesis was selected to allow for the joint space to be open approximately 2 mm when a stress was applied with the knee in full extension. Tibial and femoral prostheses were fixed using bone cement and a polyethylene spacer was fixed on the tibial tray by using a locking mechanism. Finally, tracking between the components and stability of the ligaments were confirmed and joint irrigation was done. The knee joint capsule and the skin were sutured with the knee in a flexed position (Fig. 1).
Ambulation was allowed immediately after surgery. From the 3rd postoperative day, after wound care and dressing removal, controlled exercises using a continuous passive motion machine and active motion exercises were initiated.
Clinical and radiographic assessments were carried out preoperatively and at regular intervals postoperatively. The extent of knee pain, range of motion of the knee joint, knee score, and knee function score of the patient were assessed using the Knee Society (KS) clinical rating system.7) The overall results were classified based on the KS score using Insall's criteria4) as excellent (score, 85–100), good (score, 70–84), fair (score, 60–69), and poor (score, ≤ 59). Radiographic assessment was performed using standing weight-bearing anteroposterior and lateral radiographs of the knee, and a long-standing anteroposterior radiograph of the lower extremity to measure the tibiofemoral angle and to observe any bony changes, as well as loosening, wear, or dislocations of the components. Magnetic resonance imaging (MRI) was performed preoperatively to confirm the integrity of the medial compartment and cruciate ligaments.
The preoperative and final follow-up clinical data were compared and analyzed using a retrospective investigation method. The statistical analysis of the data was performed using the paired t-test or Wilcoxon signed-rank test according to the normality of data. A p < 0.05 was considered statistically significant.
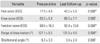
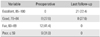
Of the total 30 cases (27 patients), 29 cases available for the minimum 2-year follow-up (mean follow-up, 3 years and 2 months; range, 24 to 48 months) were included in the analysis. The mean KS pain score was significantly improved from 17.9 points (range, 10 to 30 points) preoperatively to 40.5 points (range, 30 to 45 points) (p < 0.001) at the final follow-up. The mean KS knee score was increased from 63.2 points (range, 48 to 70 points) preoperatively to 86.0 points (range, 74 to 95 points) at the final followup. The mean KS knee function score was improved from 68.6 points (range, 35 to 80 points) preoperatively to 92.4 points (range, 60 to 100 points) at the final follow-up. Both the KS knee scores and the KS knee function scores at the final follow-ups were significantly improved compared to the preoperative scores (p < 0.001). The mean range of motion of the knee joint was improved from 127.1° (range, 110° to 135°) preoperatively to 131.6° (range, 120° to 135°) at the final follow-up (p < 0.01). The tibiofemoral angle measured on weighting-bearing radiographs changed from a mean of 6.2° of valgus (range, 0.1° to 11.4° of valgus) preoperatively to a mean of 3.4° of valgus (range, 0.2° to 9.5° of valgus) at the final follow-up (p < 0.001) (Table 1). The overall results of the lateral UKA based on the KS knee scores were classified as "excellent" in 21 cases and "good" in 8 cases (Table 2).
There was a case of failure due to consistent pain in the medial compartment after surgery, which was treated with additional surgical interventions (high tibial valgus osteotomy and revision TKA) performed at 6 and 10 months after the initial surgery (Fig. 2). The failure rate of the prosthesis was 3.3%.
More than 1,800 cases of UKA have been performed at our institution since 2002, of which lateral UKA accounts for only less than 3%. The purpose of this study was to investigate the clinical results and early complications after lateral UKA using the ZUK prosthesis with a minimum follow-up of 2 years. The results of the study demonstrated that the early clinical results of lateral UKA using the ZUK prosthesis were satisfactory for improvement of pain, knee score, function score, and recovery of knee motion for the mean follow-up of 3 years and 2 months. Despite the relatively short follow-up, the significance of this study is that it is, to the best of our knowledge, the first domestic report on lateral UKA conducted in Korea involving a relatively large number of cases of lateral UKA from a single institution.
The primary indications for lateral UKA include lateral unicompartmental osteoarthritis, osteonecrosis, traumatic arthritis with severe pain, and radiographic evidence of excessive joint space narrowing.389) A patient with an intact anterior cruciate ligament, preoperative valgus deformity of less than 15°, more than 100° of knee flexion, and no restriction on knee extension is considered suitable for a lateral UKA. Contraindications of lateral UKA include inflammatory arthritis accompanied by degenerative changes of the medial compartment and symptomatic patellofemoral arthritis.38) In particular, lateral UKA should not be performed when soft tissue release is required to treat fixed valgus deformity, since the release could cause coronal femorotibial subluxation after the surgery.310) We selected patients with osteoarthritis of the lateral compartment of the knee who complained of pain and impairment of mobility as candidates for lateral UKA. Our inclusion criteria were the absence of inflammatory diseases, normally functioning anterior and posterior cruciate ligaments, a valgus deformity of less than 15°, a flexion contracture of less than 10°, and above 100° of range of motion of the knee. We excluded patients from the lateral UKA if preoperative evaluation revealed anterior/posterior instability or degenerative changes in the medial compartment. Additionally, patients with symptomatic degenerative changes in the patellofemoral joint were excluded.
Lateral UKA procedures can differ slightly according to the type of prosthesis and instrument used. Fixed-type prostheses are particularly preferred in lateral UKA that is more difficult to perform and raises the possibility of dislocation of a mobile component compared to medial UKA.9) In general, it is known that lateral UKA is technically more challenging than medial UKA due to some anatomical and technical differences such as the relatively lax lateral ligament compared to the medial ligament and the more posterior movement of the lateral femoral condyle than that of the medial femoral condyle during knee flexion.2) The following factors should be considered in lateral UKA.2811) Incisions on the skin and knee joint capsule should be made using a minimally invasive surgical method, but the incision should also be sufficiently large to allow for examination of the entire joint, osteophyte removal, and verification of the long and anteroposterior axis of the femur and tibia.12) Bony resection of the lateral condyle of the proximal tibia should be kept to a minimum. Care should be taken to avoid excessive posterior tibial slope for achieving ligament balance after measuring the flexion gap and the extension gap using a gap spacer. A correct ligament balance is especially important during extension, but slight laxity can be acceptable during flexion. The tibial component should be internally rotated by 15°–20° on the sagittal plane and should be aligned with the patient's natural posterior slope as much as possible. The natural divergence of the lateral femoral condyle in flexion should be taken into consideration during fixation of the femoral component to avoid impingement on the tibial spine eminence in extension.2) Overcorrection of a valgus deformity to varus can cause medial compartmental arthritis; therefore, slight undercorrection of a deformity is recommended.
Lateral UKA is performed 10 times less frequently than medial UKA, and reports on its clinical results are relatively few.2,3) In a clinical study by Servien et al.10) on lateral UKA with a mean follow-up of 43 months, the mean KS knee score and function score improved from 67.7 and 68.1 to 92.5 and 86.7, respectively. The range of motion of the knee improved from 129° to 130°. Over 90% of the patients showed satisfactory results. Smith et al.13) also reported in 2014 that the mean KS knee score and function score improved from 44.1 and 56.0 to 81.7 and 76.7 at a mean follow-up of 5 years. The mean range of motion increased from 108° to 112°. Our study also showed relatively good results. In the present study, the mean KS knee score and function score significantly improved from 63.2 and 68.0, respectively, preoperatively to 86.0 and 92.4, respectively, at the final follow-up, indicating statistically significant improvement (p < 0.001). The average range of motion improved from 127.1° preoperatively to 131.6° at the final follow-up. The overall results based on knee scores were "excellent" in 21 cases and "good" in 8 cases.
Based on our review of the literature on clinical results of lateral UKA according to implant type, the short- to mid-term results of lateral UKA were satisfactory regardless of the implant type in most studies. A study by Volpi et al.14) on 23 cases of lateral UKA using the Miller-Galante prosthesis showed that the Hospital for Special Surgery (HSS) knee score improved from 59 to 88 and outstanding results were obtained in terms of pain, function, and range of knee motion during 12 to 60 months of follow-up. Liebs and Herzberg4) reported that the mean the Western Ontario and McMaster Universities Osteoarthritis index (WOMAC) pain score was 33.7 while the mean knee function score was 33.6 at 6 years after lateral UKA using the mobile-type Preservation prosthesis. A study of Altuntas et al.,15) in which lateral UKA was performed on 64 cases by using the domed mobile-bearing tibial prosthesis, also showed that the mean Oxford knee score was improved from 24 to 42 and 92% of the patients achieved satisfactory results at 38 months after surgery.
On the long-term clinical results of lateral UKA, Pennington et al.5) reported that the mean HSS knee score improved from 60 to 93 and outstanding results were observed in all cases at 12.4 years after surgery. A study by Lustig et al.,6) which used a fixed-type all-poly prosthesis in UKA and had an mean follow-up of 14.2 years, reported in 2014 that the KS knee score was 98.1, the knee function score was 82.2, and the range of knee motion was 132.6° at the final follow-up. Satisfactory results were observed in 94.4% of their patients. However, there is a controversy over the long-term survivorship of lateral UKA depending on the type of implant. In case of the mobile-type Oxford knee, Gunther et al.,16) reported that the results were unsatisfactory with 82% survival rate and 10% mobilebearing dislocation at a mean follow-up of 5 years after lateral UKA using the Oxford phase 1. Pandit et al.17) reported that a newly-developed mobile-type domed tibial prosthesis designed to reduce wear and dislocation of the polyethylene bearing with the dome-shaped surface of the tibia, improved the 4-year survival rate from 82% (phases 1 and 2 of the Oxford Knee) to 98%. According to a study by Altuntas et al.,15) in which lateral UKA performed on 64 cases using the domed mobile-type tibial prosthesis was evaluated for a mean follow-up of 3 years and 2 months, although dislocation of the mobile-bearing was not observed in any case, revision arthroplasty was needed in 2 cases (3.1%) due to instability and pain on the medial side of the knee. A study by Liebs and Herzberg,4) which used the mobile-type Preservation prosthesis, reported a 9-year survival rate of 83% in 2013.
In knees with fixed-type UKA prostheses, a small contact area is created between the metallic femoral component and the polyethylene tibial component, which results in high contact pressure per area. Consequently, failure rates after UKA using this type of prostheses are higher due to wear and loosening of the components, but early complications such as dislocation of bearing are relatively less frequent. Survival rates of fixed-type lateral UKA were reported in the past by Scott and Santore18) in 1981 (3.5-year survival rate of 83.3%) and Marmor19) in 1984 (7.4-year survival rate of 85.7%). In the 2000s, a lot of authors reported better results than those of the mobiletype prostheses including Argenson et al.1) (10-yearsurvival rate of 92% and 16-year survival rate of 84%), Servien et al.10) (10-year survival rate of 98%), and Pennington et al.5) (12.4-year survival rate of 100%). Recently, Lustig et al.6) reported a 10-year survival rate of 94% and a 15-year survival rate of 91% after all-poly fixed-bearing lateral UKA in 2014. In general, fixed-type prostheses are preferred in lateral UKA, because they have been proven to have higher survival rates than mobile-type prostheses that have be associated with higher early failure rates due to dislocation of the bearing.239)
Possible complications after lateral UKA include progression of arthritis in the medial compartment, aseptic loosening of the femoral or tibial component, periprosthetic fracture, valgus malalignment, wear or dislocation of polyethylene, deep infection, limitation of the knee motion, and unexplained severe pain.492021) A study by Citak et al.20) reported that the most common reason for failure after lateral UKA was the progression of arthritis in the medial compartment or the patellofemoral joint (43.8%) followed by aseptic loosening of the components (18.8%). Liebs and Herzberg4) reported complications occurred in 14 of 128 cases of lateral UKA performed using the mobile-type Preservation prosthesis. In their study, the most frequent complication was aseptic loosening of the prosthesis (6 cases) followed by the progression of arthritis in the medial compartment (2 cases) and fracture (2 cases). In this study, a complication was observed in 1 of the total 30 cases. A 56-year-old male patient who received lateral UKA for osteoarthritis of the lateral compartment of the knee with severe pain in the lateral knee showed no improvement until postoperative 6 months. High tibial valgus osteotomy and revision TKA were performed at 6 and 10 months, respectively, after the initial arthroplasty because of newly developed pain on the medial side of the knee joint (Fig. 2). It was discovered that the patient preoperatively had tibia vara deformity of the proximal tibia and degenerative changes in the medial compartment of the knee joint; the UKA procedure aggravated the pain by increasing the weight-bearing load on the medial compartment through overcorrection of the deformity. This case was supposed to represent a misinterpretation of the indications for the primary UKA. Therefore, careful patient selection is essential for prevention of early complications.
The limitations of this study include the relatively small number of cases and short follow-up period compared to previous studies on medial UKA. However, it should be taken into consideration that the incidence of diseases that require a lateral UKA is low and the history of lateral UKA is short in Korea. Further follow-up is warranted to investigate the long-term results of the lateral UKA.
In conclusion, the early clinical results of lateral UKA using the ZUK prosthesis were satisfactory for improvement of pain, knee score, and function score and recovery of knee motion for a mean follow-up of 3 years and 2 months. Therefore, lateral UKA could be a useful surgical modality for the treatment of osteoarthritis of the lateral compartment of the knee. For prevention of early complications after lateral UKA, care should be taken regarding patient selection. Long-term survivorship remains to be confirmed through ongoing follow-up.
Figures and Tables
Fig. 1
(A–C) Preoperative radiographs of a 60-year-old woman showing lateral osteoarthritis of both knees. (D, E) Follow-up radiographs taken 3 years after the Zimmer unicompartmental high-flex knee (Zimmer) arthroplasty.

Fig. 2
(A, B) Preoperative radiographs of a 56-year-old man showing lateral osteoarthritis of the left knee with tibia vara deformity of both knees. (C) Follow-up radiograph taken 6 months after Zimmer unicompartmental high-flex knee arthroplasty. (D) Follow-up radiograph taken 4 months after additional high tibial osteotomy. (E) Radiograph of the left knee after conversion total knee arthroplasty.

Table 1
Clinical and Radiographic Results
References
1. Argenson JN, Parratte S, Bertani A, Flecher X, Aubaniac JM. Long-term results with a lateral unicondylar replacement. Clin Orthop Relat Res. 2008; 466(11):2686–2693.

2. Ollivier M, Abdel MP, Parratte S, Argenson JN. Lateral unicondylar knee arthroplasty (UKA): contemporary indications, surgical technique, and results. Int Orthop. 2014; 38(2):449–455.

3. Heyse TJ, Tibesku CO. Lateral unicompartmental knee arthroplasty: a review. Arch Orthop Trauma Surg. 2010; 130(12):1539–1548.

4. Liebs TR, Herzberg W. Better quality of life after medial versus lateral unicondylar knee arthroplasty. Clin Orthop Relat Res. 2013; 471(8):2629–2640.

5. Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Lateral unicompartmental knee arthroplasty: survivorship and technical considerations at an average follow-up of 12.4 years. J Arthroplasty. 2006; 21(1):13–17.
6. Lustig S, Lording T, Frank F, Debette C, Servien E, Neyret P. Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee. 2014; 21:Suppl 1. S26–S32.

7. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989; (248):13–14.

8. Scott RD. Lateral unicompartmental replacement: a road less traveled. Orthopedics. 2005; 28(9):983–984.

9. Lombardi AV Jr, Berend KR, Berend ME, et al. Current controversies in partial knee arthroplasty. Instr Course Lect. 2012; 61:347–381.
10. Servien E, Aitsiselmi T, Neyret P, Verdonk P. How to select candidates for lateral unicompartmental prosthesis. Curr Orthop Pract. 2008; 19(4):451–458.

11. Panni AS, Vasso M, Cerciello S, Felici A. Unicompartmental knee replacement provides early clinical and functional improvement stabilizing over time. Knee Surg Sports Traumatol Arthrosc. 2012; 20(3):579–585.

12. Whiteside LA. Making your next unicompartmental knee arthroplasty last: three keys to success. J Arthroplasty. 2005; 20:4 Suppl 2. 2–3.
13. Smith JR, Robinson JR, Porteous AJ, et al. Fixed bearing lateral unicompartmental knee arthroplasty: short to midterm survivorship and knee scores for 101 prostheses. Knee. 2014; 21(4):843–847.

14. Volpi P, Marinoni L, Bait C, Galli M, Denti M. Lateral unicompartimental knee arthroplasty: indications, technique and short-medium term results. Knee Surg Sports Traumatol Arthrosc. 2007; 15(8):1028–1034.

15. Altuntas AO, Alsop H, Cobb JP. Early results of a domed tibia, mobile bearing lateral unicompartmental knee arthroplasty from an independent centre. Knee. 2013; 20(6):466–470.

16. Gunther TV, Murray DW, Miller R, et al. Lateral unicompartmental arthroplasty with the Oxford meniscal knee. Knee. 1996; 3(1-2):33–39.

17. Pandit H, Jenkins C, Beard DJ, et al. Mobile bearing dislocation in lateral unicompartmental knee replacement. Knee. 2010; 17(6):392–397.

18. Scott RD, Santore RF. Unicondylar unicompartmental replacement for osteoarthritis of the knee. J Bone Joint Surg Am. 1981; 63(4):536–544.

19. Marmor L. Lateral compartment arthroplasty of the knee. Clin Orthop Relat Res. 1984; (186):115–121.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download