Abstract
Background
Early stage osteonecrosis of the femoral head (ONFH) has many treatment options including core decompression with implantation of a tantalum rod. The purpose of this study was to evaluate clinical and radiological outcomes and potential complications during conversion total hip arthroplasty (THA) in such patients.
Methods
Six male patients (8 hips) underwent THA subsequent to removing a tantalum rod (group I) from April 2010 to November 2011. We retrospectively reviewed the medical records of these patients. We enrolled 12 age- and sex-matched patients (16 hips) during the same period, who had undergone primary THA without a previous operation as the control group (group II). All patients were followed for at least 3 years. We checked the Harris hip score (HHS), operative time, and volume of blood loss. Radiological results, including inclination, anteversion of the acetabular cup, presence of periprosthetic osteolysis, and subsidence of femoral stem were checked at the last follow-up.
Results
The mean preoperative HHS values were 56.5 (range, 50 to 62) and 59.1 (range, 42 to 70) in groups I and II, respectively. The HHS improved to 96.0 (range, 93 to 100) and 97.6 (range, 93 to 100), respectively, at the 3-year follow-up (p = 0.172). Mean operation time was 98.8 minutes (range, 70 to 120 minutes) in group I and 77.5 minutes (range, 60 to 115 minutes) in group II (p = 0.006). Total blood loss volumes were 1,193.8 mL (range, 960 to 1,360 mL) and 944.1 mL (range, 640 to 1,280 mL) in groups I and II, respectively (p = 0.004). No significant differences in inclination or anteversion of acetabular cup and no evidence of osteolysis or subsidence of the femoral stem were reported in either group in radiological follow-up results. However, one case of squeaking occurred in group I during the follow-up.
Nontraumatic osteonecrosis of the femoral head (ONFH) accounts for 8%–12% of all total hip arthroplasty (THA) cases in the USA.1) Various operative treatments are performed to interrupt disease progression. Core decompression with implantation of a tantalum rod is one of the options suggested for patients with early stage of ONFH.234) Implanting a tantalum rod provides bony support by acting as a buttress for the subchondral bone and encouraging bone ingrowth around the rod. However, recent studies have not shown promising outcomes, as compared to those reported previously.5) Some patients operated on with decompression showed worse pain and walking difficulties and had to undergo THA.6) However, conversion to THA for these patients is technically demanding in terms of removing the metallic rod, increased blood loss, extended operative time, bone loss, and potential risk of femoral fracture.7) The outcomes of conversion to THA in patients previously treated with implantation of a tantalum rod have not been analyzed previously. Thus, we evaluated the clinical and radiographical outcomes of conversion THA. We described the removal technique for the implanted rod and potential intraoperative and postoperative complications.
This Institutional Review Board-approved the retrospective review conducted from April 2010 to November 2011. Six patients (8 hips) underwent conversion to THA due to failure of core decompression with an implanted tantalum rod (group I). All patients were referred from other hospitals. All patients in group I were men and their mean age at surgery was 36.3 years (range, 32 to 39 years). We selected 50 male patients who underwent primary THA with the same type of implants during the same period. Exclusion criteria were reoperation, infection, and follow-up loss within 3 years. Accordingly, 12 patients (16 hips) were available for the control group (group II). All patients were diagnosed with ONFH. The initial stage and extent of ONFH assessed by plain radiographs or magnetic resonance imaging according to the Association Research Circulation Osseous (ARCO) classification were described in Table 1.8)
All conversion and primary THA surgeries were performed using the modified minimally invasive two-incision method,9) with a Delta-PF acetabular cup (Lima LTO, Udine, Italy) and fourth-generation ceramic-on-ceramic (CoC; CeramTec, Plochingen, Germany) articulation. The M/L Taper stem (Zimmer, Warsaw, IN, USA) was used in all patients, except 2 hips in group I who received the M/L Taper stem with Kinectiv modular neck (Zimmer).
The anterior incision in group I patients was extended about 1 cm distally to access the entry point for the tantalum rod. All group I patients received the Zimmer Trabecular Metal osteonecrosis screw (Zimmer Trabecular Metal Tech, Allendale, NJ, USA) (Fig. 1). The core diameter of the rod was 10 mm in the porous portion and 14 mm in the threaded portion. Thus, a 15-mm trephine was used to over-ream the rod. Before trephination, we cut the neck in the standard way using an oscillating saw. Once the rod was cut, the remaining portion was extracted in an anterograde fashion using a trephine (Fig. 2). After removing the tantalum rod, the same technique used for primary THA was applied to both groups of patients. The lateral cortical hole was packed with a bone graft from the femoral head. All subjects received the same postoperative physical therapy during their hospital stay.
Clinical results were graded using the Harris hip score (HHS) and assessed by operative time and volume of blood loss.10) Preoperative and final follow-up radiographs were evaluated to determine inclination and anteversion of the acetabular component. The classification of femoral stem osteolysis suggested by Gruen et al.11) and classification of stem subsidence proposed by Callaghan et al.12) were used to evaluate femoral stem stability. Furthermore, we used the DeLee and Charnley13) classification of acetabular osteolysis to evaluate the acetabular components.
Data were analyzed between the two groups using the Mann-Whitney U-test and IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). The p-value < 0.05 was considered significant.
The mean HHS values were 56.5 (range, 50 to 62) prior to surgery and 96.0 points (range, 93 to 100) at the 3-year follow-up in group I. The mean preoperative HHS in group II improved from 59.1 (range, 42 to 70) to 97.6 (range, 93 to 100) postoperatively. No differences were observed between each group pre- or postoperatively (p > 0.05).
Mean operation time was 98.8 minutes (range, 70 to 120 minutes) in group I and 78 minutes (range, 60 to 115 minutes) in group II (p = 0.006). Total blood loss, including intraoperative loss and postoperative drainage, were 1,193.8 mL (range, 960 to 1,360 mL) and 944.1 mL (range, 640 to 1,280 mL) in groups I and II, respectively (p = 0.004).
The mean acetabular inclination angle was 39.9° (range, 35.6° to 46.9°) and the mean acetabular anteversion angle was 21.1° (range, 15.0° to 30.9°) in group I. The inclination angle was 39.0° (range, 30.3° to 46.8°), and the anteversion angle was 20.5° (range, 9.4° to 31.3°) in group II (p > 0.05). All patients had radiographically stable implants at the last follow-up. No evidence of periprosthetic osteolysis or subsidence of the femoral stem was observed in any of the patients.
One case of an intraoperative femoral calcar crack was detected in group I, which was treated using a cerclage cable (Dall-Miles; Stryker Inc., Mahwah, NJ, USA). Additionally, 6 hips in group I shed metallic debris and one case of squeaking was reported among them. The clinical and radiographical outcomes, as well as complications were outlined in Table 2. The mean acetabular inclination and anteversion angles were 36.9° and 23.6°, respectively, in the squeaking hip. Thus, no relationship between orientation of the acetabular component and squeaking was apparent.
Core decompression and implanting a metallic rod is one of several head-preserving options for patients with ONFH. Some proponents of tantalum rod implantation advocate its advantages including core decompression, enhanced bone in-growth due to the porous surface of the rod and prevention of further collapse of the femoral head.3) However, other studies show that these procedures are primarily advocated for early, precollapse stages of ONFH, such as ARCO stage I or II. The results for these patients are not always promising and are poorer than in patients with a subchondral collapse lesion.14) Varitimidis et al.5) reported an endpoint of 70% overall survivorship with revision to THA of at 71 months. Liu et al.2) reported a 72.49% overall survival rate at 60 months postoperatively. Thus, some patients treated with core decompression eventually may need to undergo conversion THA.
Extracting a rod is technically demanding due to strong osseointegration of the porous tantalum rod.1516) Challenges include increased blood loss, longer operative time, bone loss along the trajectory of the rod, and the subsequent potential increased risk of femoral fracture. Retrograde extraction using a trephine may require accurate orienting and maintaining trajectory from end to end, which is difficult even with a C-arm guide. Additionally, some cases showed bone overgrowth at the screw insertion orifice, so the bone had to be removed with a burr. Repeated extraction attempts led to increased bone loss, particularly at the lateral femoral cortex, and generated metallic particles. Bone loss may result in trochanteric fracture while removing hardware or broaching the femoral canal could cause an unstable prosthesis (Fig. 3).1718) Generating metallic debris is inevitable during any removal method, so we performed standard neck cutting before removing the rod to minimize bone loss and the generation of metallic particles. The modulus of elasticity of a porous tantalum is similar to that of subchondral bone.19) In our cases, an oscillating saw was suitable to cut the rod without difficulty. The remnant portion of the rod was subsequently extracted using the anterograde method, and we did not experience any trochanteric fractures during rod removal. The remnant portion can be extracted in a retrograde fashion, but it was impossible because we used the two-incision technique. All subjects in group I received a bone graft acquired from the femoral head for lateral trochanteric bone defects.
The proximal-fitting type femoral stem was probably affected by bone loss at the proximal femur in the group I. However, we had no case of subsidence of the femoral stem during the follow-up.
However, several complications occurred in group I. One patient developed an intraoperative femoral calcar fracture during broaching and required an additional cable. One case of squeaking was encountered in group I but no case of noise was reported in group II. The squeaking was due to breakdown of the lubrication mechanism within the articular surface and occurs more commonly in hard bearing couplings, such as CoC articulation. A polyethylene liner is not considered optimal in shed metallic debris. Metal-on-metal bearing is hard, but complications such as a pseudotumor or elevated serum metal ions limit usage. We selected stiffer material, such as that with a CoC articulation, which is extremely resistant to wear and biologically inert. Several studies have suggested a strong association between squeaking and edge-loading.20) Several studies have reported squeaking in CoC articulations. The incidence of squeaking is 0%–12% (Table 3).2122232425) However, the incidence of squeaking in group I was higher than that in group II or other studies.
Two main factors are suggested to generate a squeak, such as edge-loading and a third body. Edge-loading is related to micro-lateralization of the head relative to the cup during gait, as the hip allows microseparation.26) Glaser et al.27) suggested that squeaking is related to microseparation, which generates edge-loading and strip-wear. We hypothesized that squeaking was associated with disseminated metallic particles around the prosthesis. Spreading particles could enter the articular interface and cause microseparation of the head to the cup and generate squeaking by edge-loading.
Several limitations in our study should be mentioned. We used the minimally invasive two-incision technique for all cases. This approach may have relevance to intraoperative femoral fracture.28) Acetabular components were used in conjunction with a femoral stem manufactured by a different company. Some authors contraindicate such usage.29) Last, the minimum 3 years follow-up duration was relatively short. Thus, we could not evaluate the long-term effects of disseminated metallic particles, which could possibly cause osteolysis around the prosthesis. Long-term studies of these patients could resolve this issue.
The clinical scores and radiographical results of the group I patients were not different from those in group II. However, group I showed significantly greater mean blood loss, extended operative time, and incidence of squeaking (1 of 8 hips). Hence, technical difficulty and preparedness to reduce potential complications including trochanteric fracture, fixation failure of the femoral stem, and squeaking due to metallic debris, should be considered.
Figures and Tables
 | Fig. 1(A) A 32-year-old male patient with a tantalum rod showed Association Research Circulation Osseous (ARCO) stage III osteonecrosis of femoral head. (B) The postoperative radiograph showed remaining metallic particles (arrowhead) and bone loss at the lateral femoral cortex. (C) Last follow-up plain radiograph. |
 | Fig. 2(A) Removal device for over-reaming the rod. (B) Cutting into the rod and trephination from the lateral femoral cortex. (C) Removing the remaining rod in an antegrade fashion. (D) Postoperative radiograph showing bone loss in the lateral cortex. |
 | Fig. 3(A) Retrograde rod extraction. (B) Over-reaming the bone through the rod and particles around the track (arrowhead). (C) Postoperative radiograph showing disseminated metallic debris around the left hip implant. A trochanteric fracture during broaching was treated with a cerclage cable. |
Table 1
Demographic Characteristics of the Patients
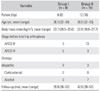
Table 2
Outcomes and Complications in the Two Groups at the 3-Year Follow-up
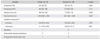
Table 3
Reports of Noise Including Squeaking in Patients with Total Hip Arthroplasty
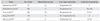
| Study | No. of hips | Mean follow-up (mo) | Liner-Head articulation | Incidence of squeaking |
|---|---|---|---|---|
| Hamilton et al. (2010)21) | 177 | 24 | 4th generation CoC | 0 |
| McDonnell et al. (2013)22) | 208 | 21 | 4th generation CoC | 26 (12.6) |
| Tai et al. (2015)23) | 206 | 28 | 4th generation CoC | 15 (7.3) |
| Kang et al. (2014)24) | 94 | 77 | 4th + 3rd generation CoC | 0 |
| Park et al. (2015)25) | 577 | 71 | 3rd generation CoC | 8 (1.4) |
References
1. Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995; 77(3):459–474.

2. Liu Y, Su X, Zhou S, Wang L, Wang C, Liu S. A modified porous tantalum implant technique for osteonecrosis of the femoral head: survivorship analysis and prognostic factors for radiographic progression and conversion to total hip arthroplasty. Int J Clin Exp Med. 2015; 8(2):1918–1930.
3. Marker DR, Seyler TM, Ulrich SD, Srivastava S, Mont MA. Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin Orthop Relat Res. 2008; 466(5):1093–1103.

4. Floerkemeier T, Lutz A, Nackenhorst U, et al. Core decompression and osteonecrosis intervention rod in osteonecrosis of the femoral head: clinical outcome and finite element analysis. Int Orthop. 2011; 35(10):1461–1466.

5. Varitimidis SE, Dimitroulias AP, Karachalios TS, Dailiana ZH, Malizos KN. Outcome after tantalum rod implantation for treatment of femoral head osteonecrosis: 26 hips followed for an average of 3 years. Acta Orthop. 2009; 80(1):20–25.

6. Papapietro N, Di Martino A, Niccoli G, et al. Trabecular metal screw implanted for avascular necrosis of the femoral head may complicate subsequent arthroplasty surgery. Eur J Orthop Surg Traumatol. 2014; 24(6):931–938.

7. Owens JB, Ely EE, Guilliani NM, Suarez JC, Patel PD. Removal of trabecular metal osteonecrosis intervention implant and conversion to primary total hip arthroplasty. J Arthroplasty. 2012; 27(6):1251–1253.

8. ARCO (Association Research Circulation Osseous). Committee on Terminology and Classification. ARCO News. 1992; 4:41–46.
9. Yoon TR, Bae BH, Choi MS. A modified two-incision minimally invasive total hip arthroplasty: technique and short-term results. Hip Int. 2006; 16:Suppl 4. 28–34.

10. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51(4):737–755.

11. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.
12. Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982: a two to five-year follow-up. J Bone Joint Surg Am. 1985; 67(7):1074–1085.

13. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.

14. Kim JO, Noh KJ, Park HS, Do NH, Kim TH, Son HS. Early clinical results in the use of a tantalum trabecular metal system for osteonecrosis of the femoral head. J Korean Hip Soc. 2009; 21(2):141–147.

15. Tsao AK, Roberson JR, Christie MJ, et al. Biomechanical and clinical evaluations of a porous tantalum implant for the treatment of early-stage osteonecrosis. J Bone Joint Surg Am. 2005; 87:Suppl 2. 22–27.

16. Tanzer M, Bobyn JD, Krygier JJ, Karabasz D. Histopathologic retrieval analysis of clinically failed porous tantalum osteonecrosis implants. J Bone Joint Surg Am. 2008; 90(6):1282–1289.

17. Papapietro N, Di Martino A, Niccoli G, et al. Trabecular metal screw implanted for avascular necrosis of the femoral head may complicate subsequent arthroplasty surgery. Eur J Orthop Surg Traumatol. 2014; 24(6):931–938.

18. Aluisio FV, Urbaniak JR. Proximal femur fractures after free vascularized fibular grafting to the hip. Clin Orthop Relat Res. 1998; (356):192–201.

19. Meneghini RM, Ford KS, McCollough CH, Hanssen AD, Lewallen DG. Bone remodeling around porous metal cementless acetabular components. J Arthroplasty. 2010; 25(5):741–747.

20. Walter WL, Kurtz SM, Esposito C, et al. Retrieval analysis of squeaking alumina ceramic-on-ceramic bearings. J Bone Joint Surg Br. 2011; 93(12):1597–1601.

21. Hamilton WG, McAuley JP, Dennis DA, Murphy JA, Blumenfeld TJ, Politi J. THA with Delta ceramic on ceramic: results of a multicenter investigational device exemption trial. Clin Orthop Relat Res. 2010; 468(2):358–366.

22. McDonnell SM, Boyce G, Bare J, Young D, Shimmin AJ. The incidence of noise generation arising from the largediameter Delta Motion ceramic total hip bearing. Bone Joint J. 2013; 95(2):160–165.

23. Tai SM, Munir S, Walter WL, Pearce SJ, Walter WK, Zicat BA. Squeaking in large diameter ceramic-on-ceramic bearings in total hip arthroplasty. J Arthroplasty. 2015; 30(2):282–285.

24. Kang BJ, Ha YC, Hwang SC, Lee YK, Koo KH. Midterm results of large diameter Biolox forte ceramic head on delta ceramic liner articulation in total hip arthroplasty. J Arthroplasty. 2014; 29(12):2412–2414.

25. Park KS, Seon JK, Yoon TR. The survival analysis in third-generation ceramic-on-ceramic total hip arthroplasty. J Arthroplasty. 2015; 30(11):1976–1980.

26. Nevelos J, Ingham E, Doyle C, et al. Microseparation of the centers of alumina-alumina artificial hip joints during simulator testing produces clinically relevant wear rates and patterns. J Arthroplasty. 2000; 15(6):793–795.

27. Glaser D, Komistek RD, Cates HE, Mahfouz MR. A noninvasive acoustic and vibration analysis technique for evaluation of hip joint conditions. J Biomech. 2010; 43(3):426–432.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download