Abstract
Background
Cruciate-retaining (CR) prostheses have been considered to produce more physiologic femoral rollback, provide better proprioception, and result in better quadriceps recovery than posterior-stabilized (PS) prostheses after total knee arthroplasty (TKA). However, there are very few studies demonstrating these benefits in an objective manner. We investigated whether CR-TKA could result in (1) better quadriceps recovery; (2) a greater proportion of patients with beyond the preoperative level of recovery; and (3) better clinical outcomes than PS-TKA.
Methods
This was a prospective non-randomized comparative study on the results of CR-TKA and PS-TKA. CR prostheses were used in 51 knees and PS prostheses in 51 knees. Quadriceps force was measured with a dynamometer preoperatively and at postoperative 6 weeks, 3 months, and 6 months consecutively. The Knee Society score (KSS) and range of motion (ROM) were also evaluated.
Results
There were no differences between two groups in terms of the objective quadriceps force during the follow-up period. The proportion of patients with beyond the preoperative level of recovery was similar between groups. Moreover, the KSS and ROM were not significantly different between two groups.
There has been a controversy regarding the selection of prosthesis during total knee arthroplasty (TKA): preservation versus substitution of the posterior cruciate ligament (PCL). The cruciate-retaining (CR) prosthesis has been considered more advantageous in improving proprioception, reproducing physiologic knee biomechanics, and restoring femoral rollback because of the preservation of the native PCL.123) Thus, it has been suggested that the CR prosthesis could improve joint sensation and clinical outcomes. Dorr et al.2) reported that the CR prosthesis was more efficient based on less muscle activity during gait in a dynamic electromyographic study. However, there are also studies with contrary results.45)
Clinical results of TKA are assessed in terms of the range of motion (ROM), the Knee Society score (KSS), the amount of pain with a visual analogue scale (VAS), patient's preference, and the timing of straight leg raising in a relatively subjective manner. Alternatively, kinematic analysis, muscle strength testing, and gait analysis are also performed in postoperative assessment.678) In particular, dynamometry provides numeric data for objective assessment of quadriceps strength.69101112)
Though there have been many comparative studies of the CR and posterior-stabilized (PS) prostheses, most of which used relatively subjective parameters 131415) except for a few studies evaluating objective parameters such as dynamometric muscle force.78) Bolanos et al.7) and Heyse et al.8) assessed quadriceps strength after TKA performed using the two types of prostheses for objective assessment of the postoperative outcomes. However, there were some limitations to these studies. In the former, patients with good or excellent knee scores were selectively included. Hence, the risk of selection bias was high. In the latter, the study was undertaken in vitro.8) Thus, the results should be verified in vivo.
There is a lack of well-designed prospective studies comparing quadriceps recovery after CR-TKA and PS-TKA. Therefore, we undertook a prospective study designed to objectively compare quadriceps recovery after CR-TKA and PS-TKA based on consecutive dynamometric assessment of the quadriceps force. Considering the aforementioned advantages of the CR prosthesis, such as better physiologic function and efficiency,2) it was hypothesized that CR-TKA would produce better quadriceps recovery than PS-TKA in terms of the objective dynamometric results. The purpose of this study was to investigate whether CR-TKA would result in (1) better quadriceps recovery; (2) a greater proportion of patients with beyond the preoperative level of quadriceps strength; and (3) better clinical outcomes than PS-TKA during the 6-month follow-up period.
One hundred and two consecutive unilateral TKAs were evaluated in this study. The 102 knees were allocated into two groups. One group underwent CR-TKA (CR group) and the other group underwent PS-TKA (PS group). Preoperative and postoperative clinical data were collected prospectively. The study was designed as a prospective, nonrandomized comparative study. The study was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong and informed patient consent was obtained. The only inclusion criterion was female patient with primary osteoarthritis of the knee indicated for an arthroplasty. The exclusion criteria were a severe flexion contracture of more than 30°, less than 100° of ROM, more than 80 years of age, valgus deformity of the knee, and previous high tibial osteotomy. Patients were followed for more than 6 months postoperatively. The demographic data were similar between the two groups (Table 1).
All operations were performed through the midvastus approach using the same technique by a single surgeon (KIK). All prostheses were implanted with bone cement and CR or PS prostheses were used in each group. The implants used were Triathlon (Stryker Orthopaedics, Mahwah, NJ, USA) in 57.8% and PFC sigma (DePuy Synthes, Warsaw, IN, USA) in 42.2%. CR prostheses were implanted in the knees with mild to moderate deformities (flexion contracture and varus deformity of less than 15°) and an intact PCL, whereas PS prostheses were inserted in the knees with more severe deformities and/or a deficient PCL.
Rehabilitation was started with continuous passive motion and active dangling exercises on the first postoperative day. Partial weight bearing using crutches or a walker was allowed from the second postoperative day. Discharge was recommended on the seventh postoperative day.
The knees were evaluated preoperatively and at 6 weeks, 3 months, and 6 months postoperatively. Baltimore Therapeutic Equipment (BTE Primus; BTE, Baltimore, MD, USA) was used for an objective assessment of the quadriceps force at each follow-up. Prior to the dynamometric examination, patients were informed of the measurement protocol, and trials were conducted to verify patients' understanding. For the BTE evaluation, the patient was seated on a chair and immobilized with straps. The fulcrum of the lever was aligned parallel to the lateral femoral condyle. Quadriceps force was measured during isometric contraction at 90° knee flexion. Three maximal isometric contractions were recorded for each knee. The examiner (KYC) reviewed the records and selected two closest values. The average of these two values was used for the analysis of quadriceps force.
All postoperative radiographs were assessed for implant position and overall alignment. At each follow-up, the ROM and KSS were recorded.
The required sample size was calculated based on our pilot study. Assuming a two-sided type I error protection of 0.05 and a power of 0.95, 42 cases in each group were required. Taking into account 10% follow-up loss and 10% discontinuance of the dynamometric examination, 51 cases were collected in each group to obtain sufficient data for the analysis. There was no case lost to follow-up, so the final statistical analysis was based on 51 knees in each group.
Independent samples t-tests were used to compare variables including age and preoperative body mass index (BMI), ROM, KSS and quadriceps force between the groups. Analysis of covariance (ANCOVA) was performed to identify factors influencing the postoperative quadriceps force after removing the preoperative quadriceps force and age as covariates at each follow-up. Repeated measures analysis of variance (ANOVA) was conducted to verify the difference in quadriceps force, KSS, and ROM during the follow-up period between the groups. A chi-square test was used to compare the proportion of patients with beyond the preoperative level of maximal quadriceps force at each follow-up. A p-value < 0.05 was considered statistically significant.
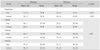
The mean preoperative ROM was significantly greater in the CR group (p = 0.027). This was because patients with more severe arthritis of the knee were assigned to the PS-TKA group. However, the mean difference was only about 6°, and there was no notable intergroup difference with regard to flexion contracture and further flexion separately. During the entire follow-up period, the objective quadriceps force did not show significant difference between the groups (Table 2). No significant intergroup difference could be found in the proportion of patients whose quadriceps force was recovered beyond the preoperative level (Fig. 1). Moreover, there were no differences between the two groups regarding the KSS and postoperative ROM (Tables 3 and 4, respectively). Although no statistical significance could be established, the mean age of the patients in the CR-TKA group was younger and the quadriceps force at postoperative 6 months was greater in the CR-TKA group. In spite of statistical insignificance, the proportion of patients with recovery of quadriceps force beyond the preoperative level was greater at 3 months and 6 months postoperatively in the CR-TKA group. Only one significant finding from the ANCONA of the dynamometric evaluation is that the preoperative quadriceps strength would affect the postoperative quadriceps force regardless of the type of prosthesis (p < 0.001). There were no intraoperative complications or postoperative infections in either group. Radiographic analyses did not reveal any differences in postoperative alignment between two groups.
The findings of the current study with serial follow-up of quadriceps recovery for the postoperative 6 months did not support our hypotheses. This might be explained with different points of view about the proprioception and femoral rollback. There is a diversity of opinion on the preservation versus substitution of the PCL.25141617) The CR prosthesis has been considered more advantageous in restoring proprioception.23) In stair climbing, enhanced proprioception from preservation of the PCL would facilitate better function. Some previous studies showed favorable results of CR-TKA, but comparable results of PS-TKA have also been reported.1716) Regarding the proprioception, some authors reported there was no difference between the two types of prostheses.45) They suggested sensory denervation of the PCL begins early in arthritis and thus the prospect of repopulation and enhancement of mechanoreceptors is limited.45) One of the distinguishing features of the PS prosthesis is the presence of femoral cam and tibial post. The PCL in the CR prosthesis produces relatively natural femoral rollback, whereas the cam and post system in the PS prosthesis replaces the PCL and creates femoral rollback. Such a posterior movement during knee flexion moves the contact point between the femur and the tibia posteriorly, resulting in a longer moment arm of the patella and the extensor mechanism.1618) For extension of the knee, the moment provided by the patellar tendon and quadriceps is a main factor, hence the reliable femoral rollback is essential for efficient knee function. Since the physiologic femoral rollback similar to that of the natural knee is more feasible with the CR prosthesis, it has been regarded as more effective in enhancing functional recovery.216) However, the paradoxical anterior femoral translation during flexion of the knee with a CR prosthesis was demonstrated in kinematic studies, which was proposed as a cause of worsening the effectiveness of the lever arm of the extensor mechanism.81920) Due to these dynamic alterations, greater quadriceps force would be needed during knee extension after CR-TKA.82122) This can be inversely interpreted as the lengthening effect of the moment arm of the extensor mechanism by femoral rollback and the lower requirement of quadriceps force during extension in knees with a PS prosthesis.1618) Proponents of the PS prosthesis have argued that rehabilitation could be achieved more easily after PS-TKA in this respect.
In the current study, the results were similar with regard to the KSS and ROM as well as quadriceps recovery between the two types of prostheses as in previous reports.131417) Thus, our results could lend support to some previous reports. Although there was a risk of selection bias due to enrollment of patients with only good or excellent KSS or Hospital for Special Surgery (HSS) scores, Bolanos et al.7) reported results similar to those of the current study. They investigated various parameters for the isokinetic muscle testing such as peak torque percent body weight, endurance, angle of peak torque, and torque acceleration energy for both quadriceps and hamstrings, which revealed no significant differences between the CR design and the PS design. Furthermore, there were no significant differences in gait analysis, ROM, and electromyographic waveforms during level walking and stair climbing.
With regard to ROM, the femoral rollback mechanism would result in posterior shift of the femur on the tibia and thus enhance posterior clearance during knee flexion.117) Consequently, this could contribute to the prevention of femorotibial impingement and achievement of a greater ROM. Also a controversy exists on this issue. Proponents of the PS prosthesis stated that constant reproduction of femoral rollback could result in superior ROM as shown in some studies.1518) In addition, a recent meta-analysis showed a significant difference in knee flexion and ROM in favor of the PS prosthesis.23) However, these studies could not conclusively demonstrate the clinical importance of the superiority of the PS prosthesis since advantages of the greater ROM was not remarkable and there was some possibility of the difference of ROM decreasing to a clinically insignificant level. In contrast, there are studies showing a greater ROM in knees with a CR prosthesis or similar ROM regardless of the prosthesis type.2716) The results of the current study also showed no significant difference in ROM between the two prostheses. Thus, we could not determine the superiority of either prosthesis in terms of ROM.
Standardized outcome measurements after TKA involve ROM, HSS, KSS, WOMAC (Western Ontario McMasters Osteoarthritis) index and SF-36 (Short Form 36) health survey. Since these conventional methods have subjective characteristics and allow insufficient distinction between study groups,1024) some authors made an effort to conduct an objective and/or intimate investigation based on evaluation of the kinematics, proprioception, quadriceps force, and alternative questionnaires.57814) Conditt et al.14) used the patient-administered Total Knee Function Questionnaire (TKFQ). The TKFQ revealed functional differences between the PS design and the CR design in spite of the similar ROM and KSS. Dynamometric evaluation could be an alternative for evaluation of the post-arthroplasty function, especially for quadriceps strength that has been recognized as a close reflection of the functional performance.12) The only previous in vivo study comparing quadriceps strength between the CR knees and PS knees reported there was no significant difference in the isokinetic muscle testing;7) however, evaluation was performed only once during the follow-up period, so changes over time were not reflected in the study. Hence, we performed serial dynamometric evaluation in the current study. There was no significant difference in quadriceps force between the two groups along the time course No significant difference was observed either when covariates such as preoperative quadriceps strength and age were excluded. Therefore, we could not conclude that one prosthesis was superior to the other prosthesis through the muscle strength testing.
This study has some limitations. Firstly, the duration of study is relatively short till the postoperative 6 months and seems to be insufficient. However, quadriceps recovery to the level of preoperative status was achieved between postoperative 3 months and 6 months as reported in previous research.1112) Therefore, the follow-up length can be considered adequate for observation of quadriceps recovery. Secondly, some selection bias was inherent in the study design. The type of prosthesis implanted in TKA was determined based on specific indications not by randomization: CR-TKA was performed on less severely affected patients. The patients in the CR group was slightly younger than those in the PS group even though the difference was not significant. Though the preoperative difference was excluded from the statistical analysis at the final follow-up, the outstanding trend of quadriceps recovery was observed in the CR group at the 6 months follow-up without significant difference. The proportion of patients with beyond the preoperative level of recovery was also greater at 3 months postoperatively in spite of statistical insignificance.
In addition, the postoperative quadriceps strength was significantly related to the preoperative strength regardless of the type of prostheses in the current study. In other words, preoperative quadriceps strength is an important influencing factor of postoperative quadriceps function. Postoperative weakness of the quadriceps muscle following TKA has been shown in several studies.6912) The importance of quadriceps strength after TKA should not be underestimated because better functional outcome is related with better quadriceps function.925) Hence, preoperative recognition of quadriceps weakness and participation of muscle strengthening exercises should be considered in preparation of TKA.25) Furthermore, more emphasis should be placed on postoperative quadriceps rehabilitation for better functional results.9)
In conclusion, CR-TKA was not more effective in restoring quadriceps strength than PS-TKA. In addition, postoperative KSS and ROM were similar between the groups. In other words, PS-TKA could result in comparable quadriceps recovery and clinical outcomes despite the greater preoperative weaknesses, such as more limited ROM, older age, and more severe osteoarthritis of the knee.
Figures and Tables
 | Fig. 1Bar graph showing the proportion of patients with beyond the preoperative level of quadriceps force. CR: cruciate-retaining, PS: posterior-stabilized. |
Table 1
Preoperative Patient Demographics
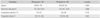
Table 2
Dynamometric Results of Quadriceps Force
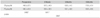
Table 3
Preoperative and Postoperative Knee Society Score
References
1. Andriacchi TP, Galante JO. Retention of the posterior cruciate in total knee arthroplasty. J Arthroplasty. 1988; 3 Suppl. S13–S19.

2. Dorr LD, Ochsner JL, Gronley J, Perry J. Functional comparison of posterior cruciate-retained versus cruciate-sacrificed total knee arthroplasty. Clin Orthop Relat Res. 1988; (236):36–43.
3. Warren PJ, Olanlokun TK, Cobb AG, Bentley G. Proprioception after knee arthroplasty: the influence of prosthetic design. Clin Orthop Relat Res. 1993; (297):182–187.
4. Simmons S, Lephart S, Rubash H, Borsa P, Barrack RL. Proprioception following total knee arthroplasty with and without the posterior cruciate ligament. J Arthroplasty. 1996; 11(7):763–768.

5. Swanik CB, Lephart SM, Rubash HE. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am. 2004; 86(2):328–334.

6. Berman AT, Bosacco SJ, Israelite C. Evaluation of total knee arthroplasty using isokinetic testing. Clin Orthop Relat Res. 1991; (271):106–113.

7. Bolanos AA, Colizza WA, McCann PD, et al. A comparison of isokinetic strength testing and gait analysis in patients with posterior cruciate-retaining and substituting knee arthroplasties. J Arthroplasty. 1998; 13(8):906–915.

8. Heyse TJ, Becher C, Kron N, et al. Quadriceps force in relation of intrinsic anteroposterior stability of TKA design. Arch Orthop Trauma Surg. 2010; 130(1):1–9.

9. Silva M, Shepherd EF, Jackson WO, Pratt JA, McClung CD, Schmalzried TP. Knee strength after total knee arthroplasty. J Arthroplasty. 2003; 18(5):605–611.

10. Tashiro Y, Miura H, Matsuda S, Okazaki K, Iwamoto Y. Minimally invasive versus standard approach in total knee arthroplasty. Clin Orthop Relat Res. 2007; 463:144–150.

11. Stevens-Lapsley JE, Balter JE, Kohrt WM, Eckhoff DG. Quadriceps and hamstrings muscle dysfunction after total knee arthroplasty. Clin Orthop Relat Res. 2010; 468(9):2460–2468.

12. Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther. 2005; 35(7):424–436.

13. Clark CR, Rorabeck CH, MacDonald S, MacDonald D, Swafford J, Cleland D. Posterior-stabilized and cruciate-retaining total knee replacement: a randomized study. Clin Orthop Relat Res. 2001; (392):208–212.
14. Conditt MA, Noble PC, Bertolusso R, Woody J, Parsley BS. The PCL significantly affects the functional outcome of total knee arthroplasty. J Arthroplasty. 2004; 19:7 Suppl 2. 107–112.

15. Lozano-Calderón SA, Shen J, Doumato DF, Greene DA, Zelicof SB. Cruciate-retaining vs posterior-substituting inserts in total knee arthroplasty: functional outcome comparison. J Arthroplasty. 2013; 28(2):234–242.e1.
16. Andriacchi TP, Galante JO, Fermier RW. The influence of total knee-replacement design on walking and stair-climbing. J Bone Joint Surg Am. 1982; 64(9):1328–1335.

17. Parsley BS, Conditt MA, Bertolusso R, Noble PC. Posterior cruciate ligament substitution is not essential for excellent postoperative outcomes in total knee arthroplasty. J Arthroplasty. 2006; 21:6 Suppl 2. 127–131.

18. Insall JN, Lachiewicz PF, Burstein AH. The posterior stabilized condylar prosthesis: a modification of the total condylar design. Two to four-year clinical experience. J Bone Joint Surg Am. 1982; 64(9):1317–1323.
19. Dennis DA, Komistek RD, Mahfouz MR. In vivo fluoroscopic analysis of fixed-bearing total knee replacements. Clin Orthop Relat Res. 2003; (410):114–130.

20. Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB. Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2003; (416):37–57.
21. Dennis DA, Komistek RD, Hoff WA, Gabriel SM. In vivo knee kinematics derived using an inverse perspective technique. Clin Orthop Relat Res. 1996; (331):107–117.

22. Matsuda S, Whiteside LA, White SE, McCarthy DS. Knee kinematics of posterior cruciate ligament sacrificed total knee arthroplasty. Clin Orthop Relat Res. 1997; (341):257–266.

23. Bercik MJ, Joshi A, Parvizi J. Posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty: a meta-analysis. J Arthroplasty. 2013; 28(3):439–444.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download