Abstract
Background
Nonoperative management of midshaft clavicle fractures has resulted in widely disparate outcomes and there is growing evidence that clavicle shortening poses the risk of unsatisfactory functional outcomes due to shoulder weakness and nonunion. Unfortunately, the literature does not clearly demonstrate the superiority of one particular method for measuring clavicle shortening. The purpose of this study was to compare the accuracy of clavicle shortening measurements based on plain radiographs with those based on computed tomography (CT) reconstructed images of the clavicle.
Methods
A total of 51 patients with midshaft clavicle fractures who underwent both a chest CT scan and standardized anteroposterior chest radiography on the day of admission were included in this study. Both an orthopedic surgeon and a musculoskeletal radiologist measured clavicle shortening for all included patients. We then determined the accuracy and intraclass correlation coefficients for the imaging modalities. Bland-Altman plots were created to analyze agreement between the modalities and a paired t-test was used to determine any significant difference between measurements.
Results
For injured clavicles, radiographic measurements significantly overestimated the clavicular length by a mean of 8.2 mm (standard deviation [SD], ± 10.2; confidence interval [CI], 95%) compared to CT-based measurements (p < 0.001). The intraclass correlation was 0.96 for both plain radiograph- and CT-based measurements (p = 0.17).
Midshaft clavicle fractures (Orthopaedic Trauma Association 15-b)1) are common injuries and may represent up to 10% of all fractures in adults.23) Historically, these injuries have been treated conservatively with acceptable results.45) However, more recent studies demonstrate widely disparate outcomes for patients undergoing nonoperative management of midshaft clavicle fractures6789) and the ideal management of these injuries remains controversial. A growing body of evidence indicates that clavicle shortening may result in unsatisfactory outcomes due to shoulder weakness and nonunion678101112) and that open reduction and internal fixation reduces this risk of poor outcomes.13141516)
The decision to pursue operative versus nonoperative management of midshaft clavicle fractures depends on several factors. Significant clavicle shortening, which has been associated with nonunion and unsatisfactory patient outcomes,7) is an indication for operative management. Therefore, accurate measurement of clavicle shortening is of paramount importance when deciding between different treatment approaches. Typically, clavicle fracture shortening has been measured on dedicated anteroposterior (AP) imaging of the clavicle or shoulder girdle17181920) although posteroanterior (PA) films of the chest have been shown to be equally useful for this purpose.812) However, Jones et al.21) recently concluded that using unilateral radiographs of the fractured clavicle was insufficient for determining the true degree of fracture shortening and suggested that other modalities may be more appropriate for determining the extent of fracture shortening.
Computed tomography (CT) imaging of the clavicle has previously been regarded as the gold standard for measurement of true clavicular length12) and an important modeling tool to establish clavicular morphology2223) CT allows for clavicle imaging in multiple planes without projection abnormalities and therefore, some believe that CT may be a more reliable modality for evaluating clavicular fracture shortening.
Despite the importance of accurately measuring clavicle fracture shortening, there exists a paucity of research comparing the accuracy of different imaging modalities for clavicle fracture shortening measurement. The purpose of this study was to compare the accuracy of clavicle shortening measurements based on plain radiographs with that of measurements based on CT-reconstructed images of the clavicle. We also aimed to determine the interobserver reliability of both imaging modalities. We hypothesized that plain radiography-based clavicle shortening measurements will be less accurate than those based on CT imaging and that CT-based measurements will demonstrate greater interobserver reliability.
After obtaining University of Southern California Keck School of Medicine Institutional Review Board approval (#HS-14-00929), our institution's orthopaedic trauma database was queried for patients with midshaft clavicle fracture.
Each patient's imaging was accessed using the picture archiving and communication system (PACS-Synapse; Fujifilm Medical Systems, Stamford, CT, USA). Patients with fractures of the midshaft clavicle were included if they received both a CT scan of the chest and a standardized supine AP view of the chest on the day of admission. Patients with fractures of the proximal or distal third region of the clavicle were excluded, as were those with bilateral clavicle fractures, previous clavicle fractures, and CT imaging that did not include both sternoclavicular and acromioclavicular joints. All radiographs were obtained by a standardized protocol developed by the department of radiology.
All measurements were performed by both an orthopaedic surgeon and a fellowship-trained musculoskeletal radiologist. Clavicle length was measured, using AP radiographs in the coronal plane, as the distance between two points placed on the center of the proximal and distal ends of the clavicle (Fig. 1). The center was determined by choosing a point that was halfway between the superior- and inferior- most aspects of the proximal end of the clavicle. The same was repeated from the distal clavicular end. The length of both clavicles was measured for each patient and the difference was recorded as the relative shortening.
CT images in the axial plane were reformatted using the multiplanar reconstruction function of Synapse PACS software in order to make CT-based clavicle shortening measurements. A clavicle-specific plane was created by orienting an oblique reconstruction through the center of the sternoclavicular joint proximally (Fig. 2A) and the center of the acromioclavicular joint distally (Fig. 2B). The resulting oblique plane visualized the entire functional length of the clavicle in its own axis (Fig. 2C). As with the plain film measurements, the length of each clavicle and the relative shortening between the two sides were recorded. Measurements were performed from the midpoint (a point that was both halfway between the superior most/inferior most aspects of the medial end of the clavicle and the anterior most/posterior most aspects of the medial end of the clavicle. The same was repeated for the lateral clavicular end).
Intraclass correlation coefficients (ICC) were then determined to compare measurements made by the two observers for each imaging modality (with 1 representing perfect reliability and 0 indicating no reliability). Bland-Altman plots were used to calculate the mean variance in measurements between the two imaging modalities and scatterplot linear regression was used to calculate the coefficient of determination (R2) between the modalities. Finally, a paired Student t-test was used to evaluate significant differences. IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA) was used for all statistical analysis.
A search of the orthopaedic trauma database revealed 194 patients diagnosed with midshaft clavicle fractures that had both an AP chest radiograph and a chest CT scan on their date of admission between January 2010 and November 2013. Of these, 134 were excluded because both acromioclavicular joints were not included in the images. An additional 8 patients were excluded because the AP chest radiograph taken on the date of admission did not include both acromioclavicular joints. One patient was excluded after closer evaluation of the imaging revealed no clavicle fracture. In total, 51 patients were included in the study (35 males and 16 females). The average age was 40 years (range, 18 to 88 years).
Table 1 demonstrates that the interobserver reliability for each of the two modalities was similar, with ICC of 0.96 for plain radiograph measurements and 0.96 for CT measurements. This difference was not significant (p = 0.17). Correlation coefficients determined from scatterplots based on the two sets of measurements confirmed this similarity (R2 = 0.93 for CT and R2 = 0.91 for radiographs).
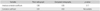
The overall length measurements differed between the two modalities. For injured clavicles, radiographic measurements overestimated the clavicular length by a mean of 8.22 mm (standard deviation [SD], ± 10.16; confidence interval [CI], 95%), which resulted in underestimation of clavicle shortening due to fracture. On average, radiographic measurements also overestimated the length of the uninjured clavicle by 6.42 mm (SD, ± 8.70; CI, 95%) compared to CT-based measurements. In both cases, the variance between the measurements based on the two modalities was significant (p < 0.001 and p < 0.001). The scatterplot shown in Fig. 3 illustrates the poor overall correlation between the two imaging modalities with a coefficient of determination of 0.34.
In our retrospective cohort study, we aimed to compare the accuracy of clavicle shortening measurements based on plain radiographs with that of measurements based on CT reconstructed images of the clavicle. We found that the use of AP plain radiographs is inaccurate when measuring clavicle fracture shortening.
Historically, closed midshaft clavicle fractures have been treated nonoperatively with excellent clinical results.45) But recently, it has been well established that clavicle fractures treated in this manner are predisposed to radiographic malunion,6789) though the clinical consequences of malunion remains controversial. Much attention has been drawn towards the effect of fracture shortening, especially unsatisfactory outcomes and fracture-related complications.67101924) Several studies have indicated that shortening of 1.5 cm6810) or 2 cm7) is associated with both poor functional outcomes and altered biomechanics.25) However, these studies were based on heterogeneous imaging modalities, including plain radiographs,78) CT scans,10) and cadaver models.25) Using a unique approach, De Giorgi et al.26) attempted to redefine shortening as a proportional value rather than an absolute measurement of length and found that a loss of length of approximately 10% (in comparison to the contralateral, uninjured clavicle) is predictive of problematic malunion.
The debate regarding the significance of fracture shortening has recently expanded to determining which imaging modality is most appropriate and, more specifically, which radiographic projection provides the most reliable data. Previous studies have utilized PA views of the chest812) or dedicated images of the clavicle15171821) or shoulder girdle.20) A more recent study by Smekal et al.12) found that standard PA chest views provided the most reliable measurements even when using chest CT imaging as a gold standard reference. Smekal et al.12) posited that the AP view, due to the greater distance between the clavicle and X-ray film, may be subject to greater projection artifact, amplification effects, and measurement errors due to positioning and rotation. Notably, their study utilized only healed clavicle fractures with varying degrees of shortened malunion.
Jones et al.21) found low interobserver reliability for measurements of length using a unilateral dedicated clavicle view, supporting the argument that this view is not reliable for measuring clavicle fracture shortening. The authors also recommended obtaining an additional chest radiograph to better define proportional shortening or, more simply, to use displacement and comminution rather than shortening as the primary indications for operative intervention.
Similar to the results found by Smekal et al.,12) we found a high interobserver correlation for both plain radiograph- and CT-based clavicle shortening measurements. The correlation between observers was minimally higher for CT images than radiographs, but this difference was not significant. This high reliability is likely due to the use of images that included the contralateral, uninjured clavicle, thereby providing a reference for fracture-related loss of length and supporting the findings of Jones et al.21) and De Giorgi et al.26) Measurements made using chest radiographs were poorly correlated with those made based on the CT gold standard and this variability was significant. We posit that such variability can be explained by the fact that no standard radiographic projection captures the length of the clavicle in its own oblique plane as can be done with a CT reconstruction. While the clinical significance of length overestimation and subsequent miscalculation of the true shortened deformity were not investigated in this study, we found that using plain chest radiography does not yield accurate measurements of clavicular length.
There are limitations to this study, most notably its retrospective design. In addition, CT imaging is obtained with the patient in a supine position, which relaxes the musculature of the shoulder girdle and may minimize the shortening deformity. Further, our evaluation was limited to only chest radiographs and evaluation of other radiographic views in comparison to CT scans may have been useful. We focused on chest radiographs because this view is most commonly used to evaluate radiographic shortening. Also, reconstruction of CT imaging in the clavicle-specific plane has not previously been standard practice. While this task has been greatly facilitated by the use of modern imaging software platforms, there may be a learning curve in its adoption and we concede that the clinical applicability is unclear at this time. Finally, we recognize that many studies, that demonstrated adverse clinical outcomes with clavicle malunion, determined shortening with the use of plain radiographs.67811) Therefore, the true shortening as measured on CT scan may overestimate the indications for surgery if these cut off values are utilized as an indication for surgery. However, there are also several other studies that utilized measurements based on CT or cadaver models when evaluating the effect of clavicle malunion on functional outcomes or scapular kinematics.1025)
The strength of this study lies in its use of CT imaging, an accepted gold standard for evaluating bony anatomy and morphology. In fact, many regard CT as the most reliable imaging modality for evaluating clavicular fracture shortening.81221) To our knowledge, our study is the first to investigate the use of a clavicle-specific oblique plane for determining clavicle fracture shortening. This technique of planar reconstruction offers accurate imaging of bony structures that may be poorly visualized on standard radiographic projections and we believe that it will find utility in other musculoskeletal applications. Further, by using a chest AP radiograph we were able to utilize a standardized protocol for radiographs that allowed for visualization of both clavicles at the time of injury.
In conclusion, chest radiography is a precise, but inaccurate modality for evaluating clavicle fracture shortening in the acute setting. Although we do not recommend routine use of CT scans to evaluate clavicle fractures, CT-based clavicle shortening measurements are more accurate and should be used in a setting where CT imaging is readily available and has already been obtained in the course of the trauma workup. Further, if clavicle shortening is to be used as a surgical indication, we recommend the use of CT-reconstructed images in a clavicle-specific oblique plane.
Figures and Tables
 | Fig. 1A depiction of how clavicle length was measured on anteroposterior chest radiographs. The length of each clavicle was measured between the center of the proximal and distal ends of the clavicle. |
 | Fig. 2Depictions of how clavicle length was measured using computed tomography. A clavicle-specific plane was created using Synapse Picture Archiving and Communication System (PACS-Synapse; Fujifilm Medical Systems) software using the center of the proximal end of the clavicle (A) and the distal end of the clavicle (B). (C) The resulting coronal oblique plane image showing the entire length of the clavicle. |
 | Fig. 3A linear regression scatter plot of computed tomography length measurements versus X-ray radiographic length measurements. The coefficient of determination (R2) value of 0.34 indicates poor correlation between the two modalities. |
Table 1
Intraclass Correlation Coefficient Values and Correlation Coefficients Determined from Plain Radiograph and Computed Tomography Scan Measurements for Clavicle Shortening
| Variable | Plain radiograph | Computed tomography | p-value |
|---|---|---|---|
| Intraclass correlation coefficient | 0.96 | 0.96 | 0.17 |
| Correlation coefficient | 0.91 | 0.93 | Not available |
References
1. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007; 21:10 Suppl. S1–S133.
2. Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002; 11(5):452–456.

3. Robinson CM. Fractures of the clavicle in the adult: epidemiology and classification. J Bone Joint Surg Br. 1998; 80(3):476–484.
4. Neer CS 2nd. Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968; 58:43–50.
5. Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968; 58:29–42.
6. Eskola A, Vainionpaa S, Myllynen P, Patiala H, Rokkanen P. Outcome of clavicular fracture in 89 patients. Arch Orthop Trauma Surg. 1986; 105(6):337–338.

7. Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997; 79(4):537–539.

8. Lazarides S, Zafiropoulos G. Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. J Shoulder Elbow Surg. 2006; 15(2):191–194.

9. Nordqvist A, Petersson CJ, Redlund-Johnell I. Mid-clavicle fractures in adults: end result study after conservative treatment. J Orthop Trauma. 1998; 12(8):572–576.

10. Ledger M, Leeks N, Ackland T, Wang A. Short malunions of the clavicle: an anatomic and functional study. J Shoulder Elbow Surg. 2005; 14(4):349–354.

11. McKee MD, Pedersen EM, Jones C, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am. 2006; 88(1):35–40.

12. Smekal V, Deml C, Irenberger A, et al. Length determination in midshaft clavicle fractures: validation of measurement. J Orthop Trauma. 2008; 22(7):458–462.

13. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: a multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007; 89(1):1–10.
14. Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004; 86-A(7):1359–1365.

15. McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012; 94(8):675–684.

16. Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD. Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005; 19(7):504–507.

17. Jubel A, Andermahr J, Prokop A, Isenberg J, Rehm KE. Minimal invasive biological osteosynthesis of the clavicle with a titanium nail. Kongressbd Dtsch Ges Chir Kongr. 2002; 119:485–490.
18. Jubel A, Andermahr J, Prokop A, Lee JI, Schiffer G, Rehm KE. Treatment of mid-clavicular fractures in adults: early results after rucksack bandage or elastic stable intramedullary nailing. Unfallchirurg. 2005; 108(9):707–714.
19. McKee MD, Wild LM, Schemitsch EH. Midshaft malunions of the clavicle: surgical technique. J Bone Joint Surg Am. 2004; 86:Suppl 1. 37–43.
20. Walz M, Kolbow B, Auerbach F. Elastic, stable intramedullary nailing in midclavicular fractures: a change in treatment strategies? Unfallchirurg. 2006; 109(3):200–211.

21. Jones GL, Bishop JY, Lewis B, Pedroza AD. MOON Shoulder Group. Intraobserver and interobserver agreement in the classification and treatment of midshaft clavicle fractures. Am J Sports Med. 2014; 42(5):1176–1181.

22. Bachoura A, Deane AS, Wise JN, Kamineni S. Clavicle morphometry revisited: a 3-dimensional study with relevance to operative fixation. J Shoulder Elbow Surg. 2013; 22(1):e15–e21.

23. King PR, Scheepers S, Ikram A. Anatomy of the clavicle and its medullary canal: a computed tomography study. Eur J Orthop Surg Traumatol. 2014; 24(1):37–42.

24. Nowak J, Holgersson M, Larsson S. Can we predict longterm sequelae after fractures of the clavicle based on initial findings? A prospective study with nine to ten years of follow-up. J Shoulder Elbow Surg. 2004; 13(5):479–486.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download