Abstract
Background
Although the valgus subtrochanteric osteotomy is considered as a standard surgical treatment for coxa vara, there is no consensus on the optimal method of fixation and osteotomy technique. Fixation of the osteotomy has been achieved by various methods including external fixation and internal fixation with pins and cerclage and a variety of plates. The aim of this study is the evaluation of the results of developmental coxa treated by Y intertrochanteric valgus osteotomy fixed with a T-buttress plate compared with other methods of fixation in the literature.
Methods
Eighteen corrective valgus intertrochanteric femoral osteotomies were performed in 18 patients (18 hips) for treatment of unilateral developmental coxa vara deformity and fixed with a T plate. There were 12 males and 6 females. The right hip was affected in 10 patients and the left hip in 8 patients. Clinically, patients were evaluated by Larson hip score. Radiographically, anteroposterior view of the pelvis and frog leg lateral views of the affected hip were taken preoperatively and compared with the findings at the final follow-up.
Results
The average follow-up was 29 months (range, 24 to 36 months). Clinical results showed improvement of the mean Larson hip score from 57.8 to 97.0 (p < 0.001). Radiological results showed that all osteotomies were completely united in 2.4 months (range, 2 to 3 months) with the achievement of the planned correction angle. The average correction of Hilgenreiner's epiphyseal angle improved from 78.2° to 27.8° (p < 0.001) at the final follow-up. The femoral neck shaft angle was improved from 93.7° to 129.9° (p < 0.001) at the final follow-up. Shortening of the affected limb was corrected from 2.8 cm to 1.3 cm (p < 0.001) at the last follow-up. No major serious complications were recorded in the present study.
Developmental coxa vara is a hip deformity characterized by a defect in endochondral ossification of the medial portion of the femoral neck, together with the progressive vertical inclination of the proximal femoral physeal plate and shortening and decrease of neck shaft angle.1) The natural history of coxa vara may be debilitating as the child develops progressive limb length discrepancy, limp pain, abductor weakness, and restricted motion. Secondary acetabular dysplasia and genu valgum may compound the problem. With the exception of some forms of developmental coxa vara that can resolve itself, a variety of surgical methods have been developed to deal with progressive coxa vara.2) There is a general agreement in the literature that a valgus osteotomy at a trochanteric or subtrochanteric level is the most definitive method for achieving the surgical correction, which means the correction of the neck shaft angle and horizontal reorientation of the growth plate. Nevertheless, there is no consensus in the literature regarding the details of osteotomy and fixation method.1234) The purpose of the present study was to evaluate the short-term results of the intertrochanteric valgus Y osteotomy with internal fixation using a contoured T plate.
Informed consent was obtained from all parents of the individual participants included in the present study. This prospective study was conducted from January 2010 to December 2013 at Zagazig University Hospitals. Eighteen corrective intertrochanteric valgus Y femoral osteotomies were performed in 18 patients (18 hips) for treatment of unilateral developmental coxa vara deformity fixed with a T-buttress plate for stabilization. The main indications of intertrochanteric valgus Y femoral osteotomies were the presence of shortening and the inferomedial triangular fragment of the neck that was not clear in all cases. They were 12 males and 6 females. The right hip was affected in 10 patients and the left hip in 8 patients. The average age at first presentation was 6.1 years (range, 5 to 7 years). All the patients included in the study had developmental coxa vara. Any patients with coxa vara of other etiologies, congenital, dysplastic, or acquired as infection or trauma were excluded from the study. The patient's chief complaints were limping with minimal or no pain. The signs that were revealed by physical examinations in all patients were short leg gait with an abductor lurch, positive Trendelenburg test, and limitation of abduction and internal rotation of the involved hip. The patients were evaluated clinically by Larson score (Iowa hip score).5) Anteroposterior (AP) view of the pelvis was obtained to measure the Hilgenreiner-epiphyseal angle (HEA) and the femoral neck-shaft angle (FNSA) and the frog leg lateral view for the assessment of the femoral anteversion was taken preoperatively, then monthly until 1-year postoperatively, and at the final follow-up. Limb scanograms for measurement of limb length discrepancy were done preoperatively and at the last follow-up in all patients.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statistical analysis was performed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Wilcoxon signed-rank test was used for statistical analysis of the results and p < 0.05 was considered statistically significant.
The angle of correction was determined by tracing paper on the plain AP radiographs of the pelvis taken with both hips in neutral rotation. The surgery was performed using the straight lateral approach to the proximal femur. The T-shaped plate (Synthesis plate and screw; Tantawi Medical Co., Cairo, Egypt) was contoured to the desired angle of correction. After removal of a triangular wedge, the osteotomy was closed. The most proximal screw was tightened and the second screw in the femoral neck was inserted. The distal fragment was secured to the plate by at least four screws starting by the proximal oblique screw in the oval hole just below the planned osteotomy site to allow compression at the osteotomy site. Wound was closed in a usual manner and drain was removed 48 hours after surgery. Postoperative immobilization in a hip spica cast was performed for 6 weeks. Full weight bearing was delayed up to 2 months after surgery.
The average follow-up was 29 months (range, 24 to 36 months). The clinical results showed improvement of the mean Larson (Iowa) hip score from 57.8 to 97.0 (p < 0.001) at the last follow-up. The radiological results showed that all the osteotomies were completely united in 2.4 months (range, 2 to 3 months), with the achievement of the planned correction angle. The average correction of the HEA was improved from 78.2° to 27.8° (p < 0.001) at the last follow-up. The FNSA was improved from 93.7° to 129.9° (p < 0.001) at the last follow-up. The shortening of the affected limb was corrected from 2.8 cm to 1.3 cm (p < 0.001) at the last follow-up measured using scanograms. Avascular necrosis, hip subluxation, premature proximal femoral physeal closure, or any serious complications were not encountered. Three patients developed keloid formation of the surgical scar. At the last follow-up, no significant or minimal recurrence of deformity was reported (Tables 1 and 2, Figs. 1, 2, 3).
There are limited choices of implants that allow secure fixation of the underlying proximal femoral osteotomy, and the selection can be particularly small in young children. Furthermore, any fixation device needs to avoid the proximal femoral growth plate, leaving a limited length of bone available for secure fixation.134) Even in cases of well-performed osteotomies, the literature cites recurrence rates of 30%–70%.6) When the HEA was corrected to < 38°, 95% of children had no recurrence of varus deformity. Some authors also recommended an overcorrection of the HEA to the normal (anatomic) value of 22° to ensure no recurrences.7) In contrast, the head-shaft angle was not found to be a reliable indicator of appropriate correction. The recurrence was mainly due to the loss of correction angle resulting from a weak fixation. Carroll et al.7) found no strong correlation between the postoperative neck shaft angle and lasting good clinical outcomes. They reported that the most consistent and reliable predictor of outcome was the HEA. Typically, an ideal implant should be rigidly applied to the underlying bone, making appropriate lateral translation of the distal fragment to avoid medial displacement of the osteotomy, which would exacerbate loading of the lateral compartment and distal femoral physis.8) Depending on the postoperative stability, some of these children may need a hip spica cast for several weeks after surgery to prevent any displacement at the osteotomy site.9) The objective of this study was to evaluate the application of a contoured T plate for fixation of intertrochanteric valgus Y osteotomy in treatment of developmental coxa vara; therefore, the focus was set on this specific implant and its handling. The T plate was designed by the Arbeitsgemeinschaft für Osteosynthesefragen (AO) group to meet the anatomic biomechanical requirement mainly in the metaphyseal areas of the bone.10) It was designed to buttress a thin cortex, to prevent a defect in cancellous bone from collapsing, or to be occasionally used as a tension band plate so as to simply prevent axial deformity resulting from shear or bending. Thus, it must be applied to the cortex that has been broken, osteomatized, or under load. In spite of being relatively thin, this plate can be found sufficiently strong if used for proper indications.
The T plate has an oval hole. This hole permits some up and down adjustments and also an oblique lag screw to be inserted through to bring the osteotomy under interfragmentary compression, enabling the plate to be used as a tension band plate.10)
The treatment of choice for developmental coxa vara has followed the recommendations of early work by Amstutz, Freiberger and Wilson in the use of either subtrochanteric or intertrochanteric osteotomies.23) Both methods have their own merits and defects.123468111213) Regarding the intertrochanteric osteotomies, the Pauwels' Y-shaped and Langenskiold valgus-producing osteotomies have been shown to provide good results. However, these osteotomies have a somewhat limited ability to correct the associated femoral neck retroversion.1415)
The subtrochanteric valgus-producing osteotomies used by many authors also have provided good and lasting clinical results. The great advantages of the intertrochanteric osteotomy over the subtrochanteric osteotomy include that it is done in the metaphyseal highly cancellous proximal femoral bone with high power of union, which is nearer to the site of the hip deformity with easier deformity correction and also it obviates radiologic disadvantage of a subtrochanteric osteotomy, which is the creation of a secondary angular deformity in the form of femoral shaft kinking distal to the primary deformity.78141617) On the other hand the authors reported that this radiological kinking remodels significantly and has no negative influence on hip function.4) In the present study, the length of the oblique limb of the Y-shaped osteotomy was fixed to be one-half of the diameter of the femur at the level of the osteotomy. This modification was taken from the original Pauwels' osteotomy where the length of the oblique limb of the Y-shaped osteotomy is determined based on the inferomedial triangular fragment of the neck which is not clear in all cases. In addition, the procedure requires smaller bone resection at the base of the wedge on the lateral cortex, consequently resulting in less postoperative shortening.8) In the present study, the average correction of HEA was significant, with insignificant or minimal recurrence of the deformity in all cases and significant improvement at the last follow-up of the mean Larson (Iowa) hip score. This was also evident in the biomechanical works of Pauwels11) and Carroll et al.7): the correction of the HEA to less than or equal to 45° with secure postoperative fixation is a crucial factor for prevention of deformity recurrence or loss of correction. In this study, we also faced some limitations that had been faced by other authors in the literature: the small study population and the lack of long-term fellow-up. In summary, the type of osteotomy may be less important than achievement of surgical correction, especially correction of the neck shaft angle to a more physiologic angle and HEA to less than 35°–40°, correction of femoral anteversion (or retroversion) to more normal values, ossification and healing of the defective inferomedial femoral neck fragment, and reconstitution of the abductor mechanism through the replacement of its normal length-tension relationship.718) Furthermore, there are successful reports on a new locking compression pediatric hip plate, which allows corrective osteotomies of the proximal femur and surgical treatment of femoral neck fractures in a safe way and provides the possibility of weight bearing based on biomechanical properties of locking screws.19)
In conclusion, the use of T plate for fixation of trochanteric valgus osteotomy in the treatment of the developmental coxa vara appears to be a reliable treatment and good solution for stable fixation of the osteotomy without nonunion, loss of correction, or deformity recurrence.
Figures and Tables
 | Fig. 1The preoperative planning and drawing of the wedge for the Y-shaped intertrochanteric osteotomy. |
 | Fig. 2The postoperative anteroposterior (A) and frog leg lateral (B) radiographs showed complete osteotomy union at 3 months follow-up. |
Table 1
Preoperative, Postoperative, and Last Follow-up Data with Mean Statistical Significance
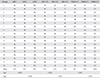
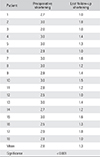
Table 2
Preoperative and Last Follow-up Shortening
ACKNOWLEDGEMENTS
We would like to express sincere thanks to Amgad Mohamed Elghreeb (an orthopedic surgery specialist in Damietta Specialized Hospital, Damietta, Egypt) and Professor Dr. Ola Hegab for their help and support in preparation of this study.
References
1. Herring JA. Tachdjian's pediatric orthopaedics: from the Texas Scottish Rite Hospital for children. 3rd ed. Philadelphia, PA: W.B. Saunders Company;2002. p. 193–195.
2. Hefny H, Elmoatasem EM, Nassar W. Valgus osteotomy by external fixation for treatment for developmental coxa vara. Strategies Trauma Limb Reconstr. 2013; 8(3):161–167.

3. Dobbs MB, Morcuende JA. Other condition of the hip: coxa vara. In : Morrissy RT, Weinstein SL, editors. Lovell and Winter's pediatric orthopaedics. 6th ed. New York, NY: Lippincott Williams & Wilkins;2005. p. 1126–1134.
4. El-Sobky T. Subtrochanteric valgus osteotomy in developmental coxa vara. Indian J Orthop. 2011; 45(4):320–323.

6. Galante VN, Caiaffa V, Franchin F, Colasuonno R. The treatment of infantile coxa vara with the external circular fixator. Ital J Orthop Traumatol. 1990; 16(4):491–500.
7. Carroll K, Coleman S, Stevens PM. Coxa vara: surgical outcomes of valgus osteotomies. J Pediatr Orthop. 1997; 17(2):220–224.

8. Cordes S, Dickens DR, Cole WG. Correction of coxa vara in childhood: the use of Pauwels' Y-shaped osteotomy. J Bone Joint Surg Br. 1991; 73(1):3–6.

9. Amstutz HC. Developmental (infantile) coxa vara: a distinct entity. Report of two patients with previously normal roentgenograms. Clin Orthop Relat Res. 1970; 72:242–247.
10. Muller ME, Allgower M, Schneider R, Willenegger H. Manual of internal fixation: techniques recommened by the AOASIF group. 3rd ed. Berlin: Springer-Verlag;1991. p. 210–213.
11. Pauwels F. Biomechanics of the normal and diseased hip: theoretical foundation, technique and results of treatment. Berlin: Springer-Verlag;1976.
12. Behrens FF, Sabharwal S. Deformity correction and reconstructive procedures using percutaneous techniques. Clin Orthop Relat Res. 2000; (375):133–139.

13. Sabharwal S, Mittal R, Cox G. Percutaneous triplanar femoral osteotomy correction for developmental coxa vara: a new technique. J Pediatr Orthop. 2005; 25(1):28–33.

14. Amstutz HC, Freiberger RH. Coxa vara in children. Clin Orthop. 1962; 22:73–92.
15. Amstutz HC, Wilson PD Jr. Dysgenesis of the proximal femur (coxa vara) and its surgical management. J Bone Joint Surg Am. 1962; 44(1):1–24.

16. Dhar SA, Dar TA, Sultan A, Malik AR, Mir MR. The reciprocal ledge closing wedge osteotomy for post traumatic coxa vara. Strategies Trauma Limb Reconstr. 2011; 6(3):155–158.

17. Bartonicek J, Vavra J. Valgus intertrochanteric osteotomy for coxa vara of Bucholz-Ogden Types II and III in patients older than 30 years. Arch Orthop Trauma Surg. 2011; 131(9):1211–1217.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download